Post-COVID-19 illness
There have been some reports of long term illness in survivors of COVID-19; it is unclear how many people are affected at this stage.[1][2][3] A small early study from Wuhan, China, found that survivors of COVID-19 who tested negative twice before discharge from hospital still had some abnormalities in metabolism and liver function markers when discharged.[4]
Long COVID[edit | edit source]
Many patients, dubbed long haulers, have described continuing symptoms of COVID-19, often described as long COVID, which include chronic, severe fatigue, brain fog (thinking and concentration problems), breathlessness, muscle pain, inability to exercise and other symptoms.[5][6] Several studies have found groups of patients continuing to experience many symptoms of COVID-19,[7][8] including patients who were not ill enough to be hospitalized.[6] There is an absence of medical advice and little information on the likely prognosis for these patients.[5]
Relapse or reinfection[edit | edit source]
Some patients have described feeling fully recovered, then experiencing COVID-19 symptoms again, and feeling like their lungs were "on fire" for some weeks afterwards.[3] There has been uncertainty about whether this is a relapse due to the virus remaining at low levels in the body and being reactivated, an immune system rebound response, or a reinfection; a relapsing / remitting pattern of COVID-19 became known as Long COVID.[9][10][11]
Post-SARS illness[edit | edit source]
COVID-19 is caused by the SARS-CoV-2 virus; the similar SARS-CoV coronavirus causes SARS, and SARS is known to have caused long term illness in some survivors, including chronic fatigue syndrome and a post-SARS syndrome similar to fibromyalgia involving chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep.[12][13]
Severe COVID-19 survivors[edit | edit source]
Post-Intensive Care Syndrome[edit | edit source]
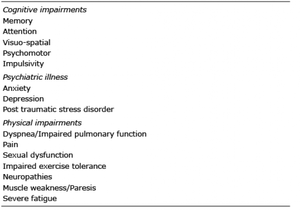
Long term physical, cognitive and mental health problems have also been found to be relatively common in patients discharged from intensive care from illnesses other than COVID-19, with the length of time in intensive care influencing the long term health impacts.[14]
Post Intensive Care Syndrome (PICS) is one of several conditions that can result, including Critical Illness Polyneuropathy (CIP) and Critical Illness Myopathy (CIM), and requires both short and medium term rehabilitation treatments.[15]
COVID-19 pneumonia and SARI[edit | edit source]
Moderately ill patients with COVID-19 may develop mild viral pneumonia.[16] Severe acute respiratory infection (SARI) is known to develop in some people severely ill with COVID-19. SARI resulting from other illnesses has been studied.[17]
Acute respiratory distress syndrome[edit | edit source]
Acute respiratory distress syndrome (ARDS) is a life-threatening condition that involves the patient's lungs becoming inflamed, and being unable to produce enough oxygen for the body's vital organs.[18] ARDS develops in 17-29% of hospitalized COVID-19 patients and is known to have long term effects.[19][20][16] ARDS can cause nerve and muscle damage, which causes pain and weakness.[18]
Mechanical ventilator effects[edit | edit source]
Invasive ventilation using a mechanical ventilator was needed by 47-71% of patients admitted to Intensive Care Units.[19]
COVID-19 complications[edit | edit source]
These include:
- Anecdotal reports of DVT and pulmonary embolism in critically ill patients
- Central nervous system encephalitis and encephalomyelitis
- anecdotal evidence of pulmonary aspergillosis
- pneumonia
- hypoxemic respiratory failure/ARDS
- sepsis and septic shock
- cardiomyopathy and arrhythmia
- acute kidney injury
- complications from prolonged hospitalization including:
- secondary infections including bacterial and fungal infections
- thromboembolism
- gastrointestinal bleeding
- critical illness polyneuropathy/myopathy.[19][16][21]
Fatigue after COVID-19[edit | edit source]
COVID-19 can cause severe fatigue, however experiencing fatigue after recovering from the virus should not be the considered the same as the illness chronic fatigue syndrome (CFS) or myalgic encephalomyelitis (ME), a neurological disease involving multiple bodily systems and sustained symptoms over an extended period of time.[22][23] Post-viral fatigue which does not meet the criteria for CFS or ME and lasts at least 6 months is known as chronic fatigue (without the "syndrome"), or idiopathic chronic fatigue if the cause is unknown.[24][25][23]
Potential brain damage[edit | edit source]
Scientists warn of a potential wave of coronavirus-related brain damage as new evidence suggests COVID-19 can lead to severe neurological complications, including brain inflammation, psychosis and delirium.[26][21]
“Whether we will see an epidemic on a large scale of brain damage linked to the pandemic – perhaps similar to the encephalitis lethargica outbreak in the 1920s and 1930s after the 1918 influenza pandemic – remains to be seen,” said Michael Zandi, from UCL’s Institute of Neurology, who co-led the study.[26]
Reuters reported:
A study by researchers at University College London (UCL) described 43 cases of patients with COVID-19 who suffered either temporary brain dysfunction, strokes, nerve damage or other serious brain effects.
Previous research has also shown COVID-19 could damage the brain in some patients.[26][21]
Post-viral syndrome[edit | edit source]
Post-viral syndrome or post-viral state is sometimes used to refer to symptoms that occur as a result of a virus, which take longer than a few weeks to resolve. The older term Post-infective fatigue is no longer in use. Post-viral syndrome may include shortness of breath, fatigue, difficulty thinking, aches and pains, or other symptoms, and typically improves gradually over time. People who remain ill after 6 months may meet the criteria for postviral fatigue syndrome (PVFS), which is more commonly diagnosed as chronic fatigue syndrome or myalgic encephalomyelitis, although it may be possible to diagnose this sooner using the international consensus criteria.[23][25][24] For most people, this is a very disabling, long-term (chronic) illness.[1][22][23][25]
Dr. Anthony Fauci, the United States top infectious disease expert, acknowledged that many unrecovered COVID-19 patients may have ME, also known as chronic fatigue syndrome, or ME/CFS.[27][28] Dr. Fauci stated: “There may well be a post-viral syndrome associated with Covid-19,...If you look anecdotally, there is no question that there are a considerable number of individuals who have a post-viral syndrome that in many respects incapacitates them for weeks and weeks following so-called recovery,”[28] At the International AIDS conference, Fauci stated: "Brain fog, fatigue, and difficulty in concentrating. So this is something we really need to seriously look at because it very well might be a post-viral syndrome associated with COVID-19.[29]
An internist at Texas Health Presbyterian Hospital, Dr. Donna Casey, said “We can now see documented abnormalities in your nervous system, immune, and metabolic systems. So we’re seeing abnormalities in all three that create myalgic encephalomyelitis.”[30] Dr. Casey did say that we are not at the six month mark[31][32] for COVID, but she does see ongoing improvement in her hospitalized patients.[30] Dr. Amir K. Ghiassi, a pulmonologist with St. Joseph Hospital in Orange County, California said of the ongoing symptoms they were uncertain if it had to do with the virus or “because of the immune system reacting the way it does that causes symptoms.”[30]
Postviral fatigue syndrome and ME/CFS[edit | edit source]
Myalgic encephalomyelitis, better known as ME, is a neurological disease that commonly begins after a virus, although other possible triggers include bacterial infections, injuries, surgery and other events.[24][23][33] Some researchers and some patients use the term chronic fatigue syndrome (CFS), or ME/CFS to refer to ME, although CFS has different diagnostic criteria.[25][24][23] The older term Postviral fatigue syndrome (PVFS) is rarely used, although the World Health Organization recognize PVFS, ME, and CFS using the same diagnostic code. Some countries including the United States, deviate from this.[33][34]
This term was introduced during the eariy 1980s in Britain as an alternative to ME. It remains a useful description for anyone whose illness can clearly be traced back to an acute viral infection. The drawback to PVFS is that it cannot be used to describe cases where some other factor (e.g. vaccination or pesticide) acted as the principal trigger.[35]
Moldofsky et al. (2011) conducted a long term follow up of 21 SARS survivors in Toronto, Canada, all of who remained too ill to return to work, and concluded that that chronic post-SARS was similar to fibromyalgia.[13] Lam et al. (2009) conducted a much larger long term follow-up of SARS survivors in Hong Kong, and reported that 27% had chronic fatigue syndrome, 40% had chronic fatigue, and 40% has depression.[12] A number of the SARS survivors unable to return to work were previously healthy health-care workers.[12] The high rates of chronic fatigue could not be accounted got by depression or psychiatric illness.[12]
Treatment[edit | edit source]
No treatment studies have yet been published, despite this and the uncertainty over long term physical and psychological health consequences of coronavirus disease 19 (COVID-19), some self-help advice has already been published.[22]
A group of over 20 ME and chronic fatigue syndrome specialists and patient groups have recommended fatigue after COVID-19 should be treated/managed using:
- pacing
- nutrition and
- sleep hygiene, stating that should help reduce the risk of developing ME/CFS after COVID-19.[36][22]
Pacing[edit | edit source]
Less controversially, the self-help leaflet mentions pacing, a symptom-management approach also without evidence for COVID-19 survivors, but which is used by many people with chronic fatigue, chronic pain, and/or persistent illness that limits their everyday activities.[37] ME patient associations surveys have found pacing helped most, but not all, patients.[38][39]
CBT and GET not recommended for fatigue[edit | edit source]
The Oxford Health NHS Foundation Trust published a Coping with Coronavirus: Fatigue leaflet referring to chronic fatigue syndrome, a neurological disease, as a possible mental health consequence of COVID-19, and confusing fatigue after COVID-19 illness with chronic fatigue syndrome. The leaflet recommenddations included the highly controversial use of cognitive behavioral therapy (CBT) and graded exercise therapy (GET) to address the physical symptoms of chronic fatigue syndrome. The leaflet was withdrawn after public health expert David Tuller asked for the evidence based used by it, details of its authorship, and strongly criticised the advice given in it. An open letter opposing the leaflet was signed by a large number of medical professionals and UK patient groups at around the same time.[22]
CBT for fatigue is a psychological therapy focused on treating a presumed illness beliefs such as a fear of activity and GET is exercise/activity based, both treatments rely on the assumption that there is no lasting physical damage or underlying illness process that could prevent full recovery. GET is particularly controversial and has been found to cause most patients with chronic fatigue syndrome (not resulting from COVID-19) to deteriorate, sometimes permanently.[22] CBT and GET are no longer recommended by the CDC, and their use within the UK's National Health Service is currently under review, with many concerns having been raised about high rates of patient harm resulting from these treatments, and a lack of effectiveness.[38][40][41][39] CBT and GET they are not recommended by the UK's ME Association, Action for ME, Invest in ME Research, The MEAction Network, or The 25% ME Group.[40][41][42][39][41] CBT may be useful for depression or generalized anxiety.[43][44]
Recovery advice[edit | edit source]
- MEA Information on Post-viral fatigue (PVF) and Post-viral fatigue syndrome (PVFS) following coronovirus infection - ME Association (May 2020)
- Post Covid-19 Rehabilitation - Physios for ME, Workwell Foundation, and ME Association (May 2020)
Notable studies on the short- and long-term effects of COVID-19[edit | edit source]
- Jun 25, 2020, Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study[21] - (Full text) from the CoroNerve platform
- Jun 29, 2020 (pre-print), Blood parameters measured on admission as predictors of outcome for COVID-19; a prospective UK cohort study[45] - (Full text) - from the DISCOVER study
- Jul 8, 2020, Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation[7] - (Full text)
- Jul 8, 2020, The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings[46] - (Full text)
- Aug 14, 2020 (pre-print), Patient outcomes after hospitalisation with COVID-19 and implications for follow-up; results from a prospective UK cohort[8] - (Full text) - from the DISCOVER project
Notable studies announced or in progress[edit | edit source]
- CoroNerve Study Group - by collaboration of specialists in neurology, psychiatry, stroke and intensive care run by Perspectum, Oxford University Hospitals NHS Trust and the Mayo Clinic, UK - website
- COVID-19 and ME/CFS - severely ill hospitalised patients will be followed through recovery and rehabilitation, with biological samples taken at different stages, to look at how patients who develop ME/CFS and post-viral fatigue triggered by COVID-19 do so, and to look at monitor other illness which may develop eg fibromyalgia - run by the Open Medicine Foundation charity - US and Sweden - Website
- DISCOVER - DIagnostic and Severity markers of COVid-19 to Enable Rapid triage
- University of Bristol, UK - DISCOVER announcement
- COVID Symptom Study and the related COVID Symptom Study App by ZOE, with KCL and the NHS - COVID Symptom Study website
- The world's largest set of data for investigating Long COVID[47] Lead by Tim Spector.
- Covid-19 Symptômes persistants enquête - France
- COVIDENCE UK Research Study
- A UK-wide study with a number of different aims, including monitoring long term complications of COVID-19, recovery, and wider physical, mental and economic wellbeing.[48] - COVIDENCE website
- PHOSP-COVID - Post-HOSPitalisation COVID - PHOSP-COVID website
- "a consortium of leading researchers and clinicians from across the UK working together to understand and improve long-term health outcomes for patients who have been in hospital with confirmed or suspected COVID-19", University of Leicester, UK
- List of Long Covid studies - ME Action
News articles and blogs[edit | edit source]
- Aug 20, 2020, Coronavirus patients still suffering from complications three months later, study finds - The Independent
- Aug 19, 2020, Long haulers are redefining COVID-19[49] - The Atlantic
- Jul 29, 2020, COVID-19 'long-haulers' report nearly 100 symptoms for more than 100 days[50] - Erika Edwards, NBC News
- Jul 9, 2020, Coronavirus may cause fatigue syndrome, Fauci says
- Jul 1, 2020, Three Months In, These Patients Are Still Ravaged by Covid’s Fallout - Wall Street Journal
- May 18, 2020, Paul Garner: Covid-19 and fatigue—a game of snakes and ladders - The BMJ
- May 4, 2020, Fever, fatigue, fear: For some recovering COVID-19 patients, weeks of illness, uncertainty - Erika Edwards, NBC News
- Apr 17, 2020, Coronavirus survivors say they fear long-term effects - Melissa Malamut, New York Post
- Apr 17, 2020, What we know about coronavirus' long-term effects[51] - Erin Shumaker, ABC news
- Apr 16, 2020, Trial By Error: Oxford-NHS Recommends GET/CBT for Post-COVID “CFS” Patients[37] - David Tuller
- Apr 16, 2020, Those Who Get COVID-19 and Get Healed Can Face Another Disease After A Few Years - Daniel Kucher - SOMAG news
- Apr 15, 2020, Could the coronavirus trigger post-viral fatigue syndromes?[1] - Clare Wilson, New Scientist
- Apr 15, 2020, Coronavirus destroys lungs. But doctors are finding its damage in kidneys, hearts and elsewhere[52] - Lenny Bernstein, Carolyn Y. Johnson, Sarah Kaplan and Laurie McGinley, Washington Post
- Apr 13, 2020, We Need to Talk About What Coronavirus Recoveries Look Like[53] - Fiona Lowenstein and Hannah Davis, New York Times Opinion
- Apr 2, 2020, Will COVID-19 -19 leave an explosion of ME/CFS cases in its wake? - blog by Cort Johnson
- Mar 28, 2020, 'Post intensive-care syndrome': Why some COVID-19 patients may face problems even after recovery[14] - Erika Edwards, NBC News
See also[edit | edit source]
- Chris Brightling
- COVID-19 (Coronavirus disease 19)
- Long COVID
- Myalgic encephalomyelitis
- Chronic fatigue syndrome - the neurological disease
- Postviral fatigue syndrome
- Chronic fatigue - a symptom of many illnesses
- Opposition to to Oxford Health NHS Foundation Trust: "Coping with Coronavirus: Fatigue"
- Fibromyalgia
- Living with M.E.[35] - Dr Charles Shepherd (book)
Learn more[edit | edit source]
- Sep 2020, COVID-19: Long Term Health Effects - NHS
- May 2020, MEA Information on Post-viral fatigue (PVF) and Post-viral fatigue syndrome (PVFS) following coronovirus infection[54] - ME Association
- May 2020, Post Covid-19 Rehabilitation[55] - Physios for ME, Workwell Foundation, and ME Association
- May 2020, Patients at higher risk of developing ME after COVID-19 diagnosis - University of Leicester
- Apr 30, 2020, Covid-19 and Post-viral Fatigue Syndrome[56] - Charles Shepherd, ME Association
- Coronavirus disease 19 (SARS-CoV-2) - John Hopkins University
- List of Long Covid studies - ME Action
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Wilson, Clare (April 15, 2020). "Could the coronavirus trigger post-viral fatigue syndromes?". New Scientist.
- ↑ Kucher, Daniel (April 16, 2020). "User Those Who Get COVID-19 and Get Healed Can Face Another Disease After A Few Years". SOMAG news.
- ↑ 3.0 3.1 Malamut, Melissa (April 17, 2020). "Coronavirus survivors say they fear long-term effects". New York Post.
- ↑ Wu, Di; Shu, Ting; Yang, Xiaobo; Song, Jian-Xin; Zhang, Mingliang; Yao, Chengye; Wen, Liu; Huang, Muhan; Yu, Yuan (April 21, 2020). "Plasma Metabolomic and Lipidomic Alterations Associated with COVID-19". medRxiv: 2020.04.05.20053819. doi:10.1101/2020.04.05.20053819.
- ↑ 5.0 5.1 Yelin, Dana; Wirtheim, Eytan; Vetter, Pauline; Kalil, Andre C.; Bruchfeld, Judith; Runold, Michael; Guaraldi, Giovanni; Mussini, Cristina; Gudiol, Carlota (October 1, 2020). "Long-term consequences of COVID-19: research needs". The Lancet Infectious Diseases. 20 (10): 1115–1117. doi:10.1016/S1473-3099(20)30701-5. ISSN 1473-3099. PMID 32888409.
- ↑ 6.0 6.1 National Health Service (September 7, 2020). "COVID-19 Long Term Health Effects".
- ↑ 7.0 7.1 Halpin, Stephen J.; McIvor, Claire; Whyatt, Gemma; Adams, Anastasia; Harvey, Olivia; McLean, Lyndsay; Walshaw, Christopher; Kemp, Steven; Corrado, Joanna. "Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation". Journal of Medical Virology. 93 (2): 1013–1022. doi:10.1002/jmv.26368. ISSN 1096-9071.
- ↑ 8.0 8.1 Arnold, David T.; Hamilton, Fergus W.; Milne, Alice; Morley, Anna; Viner, Jason; Attwood, Marie; Noel, Alan; Gunning, Samuel; Hatrick, Jessica (August 14, 2020). "Patient outcomes after hospitalisation with COVID-19 and implications for follow-up; results from a prospective UK cohort". medRxiv: 2020.08.12.20173526. doi:10.1101/2020.08.12.20173526.
- ↑ Whitaker, Phil. "What I've learned on the front line against Long Covid". New Statesman. Retrieved October 7, 2020.
- ↑ Buskermolen, Maaike; Te Paske, Karlijn; Van Beek, Janko; Kortbeek, Titia; Götz, Hannelore; Fanoy, Ewout; Feenstra, Sabiena; Richardus, Jan Hendrik; Vollaard, Albert (June 17, 2021). "Relapse in the first 8 weeks after onset of COVID-19 disease in outpatients: Viral reactivation or inflammatory rebound?". Journal of Infection. doi:10.1016/j.jinf.2021.06.015. ISSN 0163-4453. PMID 34147529.
- ↑ Tang, Xiujuan; Musa, Salihu S.; Zhao, Shi; He, Daihai (June 11, 2021). "Reinfection or Reactivation of Severe Acute Respiratory Syndrome Coronavirus 2: A Systematic Review". Frontiers in Public Health. 9. doi:10.3389/fpubh.2021.663045. ISSN 2296-2565. PMC 8226004. PMID 34178920.
- ↑ 12.0 12.1 12.2 12.3 Lam, Marco Ho-Bun; Wing, Yun-Kwok; Yu, Mandy Wai-Man; Leung, Chi-Ming; Ma, Ronald C.W.; Kong, Alice P.S.; So, W.Y.; Fong, Samson Yat-Yuk; Lam, Siu-Ping (December 14, 2009). "Mental Morbidities and Chronic Fatigue in Severe Acute Respiratory Syndrome Survivors: Long-term Follow-up". Archives of Internal Medicine. 169 (22): 2142–2147. doi:10.1001/archinternmed.2009.384. ISSN 0003-9926.
- ↑ 13.0 13.1 Moldofsky, Harvey; Patcai, John (March 24, 2011). "Chronic widespread musculoskeletal pain, fatigue, depression and disordered sleep in chronic post-SARS syndrome; a case-controlled study". BMC Neurology. 11 (1): 37. doi:10.1186/1471-2377-11-37. ISSN 1471-2377. PMC 3071317. PMID 21435231.
- ↑ 14.0 14.1 Edwards, Erika (March 28, 2020). "Potential Post intensive-care syndrome': Why some COVID-19 patients may face problems even after recovery". NBC News.
- ↑ Stam, H J; Stucki, G; J, Bickenbach (April 15, 2020). "Covid-19 and Post Intensive Care Syndrome: A Call for Action". Journal of rehabilitation medicine. doi:10.2340/16501977-2677. PMID 32286675. Retrieved April 23, 2020.
- ↑ 16.0 16.1 16.2 CDC (February 11, 2020). "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. Retrieved April 22, 2020.
- ↑ Zhang, Chen; Zhu, Na; Xie, Zhengde; Lu, Roujian; He, Bin; Liu, Chunyan; Ma, Xuejun; Tan, Wenjie (August 22, 2013). "Viral Etiology and Clinical Profiles of Children with Severe Acute Respiratory Infections in China". PLOS ONE. 8 (8): e72606. doi:10.1371/journal.pone.0072606. ISSN 1932-6203. PMC 3750056. PMID 23991128.
- ↑ 18.0 18.1 National Health Service (October 17, 2017). "Acute respiratory distress syndrome (ARDS)". nhs.uk. Retrieved April 1, 2020.
- ↑ 19.0 19.1 19.2 Auwaerter, Paul G. (April 8, 2020). "Coronavirus COVID-19 (SARS-CoV-2)". Retrieved April 17, 2020.
- ↑ CDC COVID-19 Response Team (March 27, 2020), "Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19) — United States, February 12–March 16, 2020", MMWR Morb Mortal Wkly Rep 2020, 69 (12): 343–346, doi:10.15585/mmwr.mm6912e2, PMID 32214079
- ↑ 21.0 21.1 21.2 21.3 Varatharaj, Aravinthan; Thomas, Naomi; Ellul, Mark A; Davies, Nicholas W S; Pollak, Thomas A; Tenorio, Elizabeth L; Sultan, Mustafa; Easton, Ava; Breen, Gerome (June 2020). "Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study". The Lancet Psychiatry. 7: 875–82. doi:10.1016/s2215-0366(20)30287-x. ISSN 2215-0366. PMC 7316461. PMID 32593341.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 "Opposition to Oxford Health NHS Foundation Trust: "Coping with Coronavirus: Fatigue"" (PDF). April 20, 2020.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 Fukuda, K.; Straus, S.E.; Hickie, I.; Sharpe, M.C.; Dobbins, J.G.; Komaroff, A. (December 15, 1994). "The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group" (PDF). Annals of Internal Medicine. American College of Physicians. 121 (12): 953–959. ISSN 0003-4819. PMID 7978722.
- ↑ 24.0 24.1 24.2 24.3 Carruthers, BM; van de Sande, MI; De Meirleir, KL; Klimas, NG; Broderick, G; Mitchell, T; Staines, D; Powles, ACP; Speight, N; Vallings, R; Bateman, L; Bell, DS; Carlo-Stella, N; Chia, J; Darragh, A; Gerken, A; Jo, D; Lewis, DP; Light, AR; Light, KC; Marshall-Gradisnik, S; McLaren-Howard, J; Mena, I; Miwa, K; Murovska, M; Stevens, SR (2012), Myalgic encephalomyelitis: Adult & Paediatric: International Consensus Primer for Medical Practitioners (PDF), ISBN 978-0-9739335-3-6
- ↑ 25.0 25.1 25.2 25.3 Carruthers, Bruce M.; Jain, Anil Kumar; De Meirleir, Kenny L.; Peterson, Daniel L.; Klimas, Nancy G.; Lerner, A. Martin; Bested, Alison C.; Flor-Henry, Pierre; Joshi, Pradip; Powles, AC Peter; Sherkey, Jeffrey A.; van de Sande, Marjorie I. (2003), "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols" (PDF), Journal of Chronic Fatigue Syndrome, 11 (2): 7–115, doi:10.1300/J092v11n01_02
- ↑ 26.0 26.1 26.2 "Scientists warn of potential wave of COVID-linked brain damage". Reuters. July 7, 2020. Retrieved July 8, 2020.
- ↑ "Post-Covid syndrome prompts new look at chronic fatigue syndrome". STAT. July 21, 2020. Retrieved July 21, 2020.
- ↑ 28.0 28.1 Berlinger, Joshua; McKeehan, Brett; Kottasová, Ivana; Upright, Ed; Wagner, Meg; Macaya, Melissa (July 9, 2020). "Coronavirus may cause fatigue syndrome, Fauci says". CNN. Retrieved July 21, 2020.
- ↑ https://www.youtube.com/watch?v=UMmT48IC0us
- ↑ 30.0 30.1 30.2 Ramaswamy, Divya (July 17, 2020). "Fauci Warns Of 'Post-Viral Syndrome' Among COVID-19 Patients That Causes Fatigue, Brain Fog After Recovery". International Business Times. Retrieved July 21, 2020.
- ↑ "IOM 2015 Diagnostic Criteria | Diagnosis | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. November 19, 2019. Retrieved July 21, 2020.
- ↑ "Diagnostic Algorithm for ME/CFS". National Academy of Medicine (Formerly the Institute of Medicine).
- ↑ 33.0 33.1 World Health Organization. "ICD-10: Version 2016". World Health Organization.
- ↑ Centers for Disease Control. "ICD-10-CM". Centers for Disease Control and Prevention. Retrieved April 17, 2020.
- ↑ 35.0 35.1 Shepherd, Charles (December 5, 2008). Living With M.E.. Random House. ISBN 978-1-4090-2095-0.
- ↑ Vink, Mark; Vink-Niese, Alexandra (September 20, 2019). "Work Rehabilitation and Medical Retirement for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. A Review and Appraisal of Diagnostic Strategies". Diagnostics. 9 (4): 124. doi:10.3390/diagnostics9040124. ISSN 2075-4418.
- ↑ 37.0 37.1 Tuller, David (April 16, 2020). "Trial By Error: Oxford-NHS Recommends GET/CBT for Post-COVID "CFS" Patients". Virology blog.
- ↑ 38.0 38.1 ME Association (April 3, 2019). "Forward-ME and Oxford Brookes University announce results of Patient Survey on CBT and GET in ME/CFS | 3 April 2019".
- ↑ 39.0 39.1 39.2 Invest in ME Research (July 17, 2017). "Response to NICE 10 year surveillance (2017) – Chronic fatigue syndrome/myalgic encephalomyelitis". Invest in ME Research. Retrieved February 7, 2019.
- ↑ 40.0 40.1 The ME Association (May 30, 2015). "ME/CFS Illness Management Survey Results "No decisions about me without me"" (PDF).
- ↑ 41.0 41.1 41.2 Action for ME (2014). "Time to deliver: initial findings of Action for ME's 2014 survey" (PDF). Retrieved July 1, 2016.
- ↑ Action for ME (May 17, 2017). "Our Board of Trustees on CBT, GET and PACE". Action for ME.
- ↑ National Health Service (October 24, 2017). "Clinical depression". National Health Service. Retrieved April 29, 2020.
- ↑ National Health Service (July 18, 2018). "Generalised anxiety disorder in adults - Treatment". National Health Service. Retrieved April 29, 2020.
- ↑ Arnold, David T.; Attwood, Marie; Barratt, Shaney; Elvers, Karen; Morley, Anna; McKernon, Jorgen; Oates, Adrian; Donald, Charmaine; Noel, Alan (June 29, 2020). "Blood parameters measured on admission as predictors of outcome for COVID-19; a prospective UK cohort study". medRxiv: 2020.06.25.20137935. doi:10.1101/2020.06.25.20137935.
- ↑ Paterson, Ross W.; Brown, Rachel L.; Benjamin, Laura; Nortley, Ross; Wiethoff, Sarah; Bharucha, Tehmina; Jayaseelan, Dipa L.; Kumar, Guru; Raftopoulos, Rhian E. "The emerging spectrum of COVID-19 neurology: clinical, radiological and laboratory findings". Brain. 143 (2020): 3104–3120. doi:10.1093/brain/awaa240.
- ↑ "Why you need both apps. The COVID Symptom Study app and NHS COVID-19 app are different. Here's why you need both!". joinzoe.com. October 5, 2020.
- ↑ "COVIDENCE UK". qmul.ac.uk. Retrieved July 23, 2021.
- ↑ Yong, Ed (August 19, 2020). "Long-Haulers Are Redefining COVID-19". The Atlantic. ISSN 1072-7825. Retrieved August 21, 2020.
- ↑ Edwards, Erika (July 29, 2020). "COVID-19 'long-haulers' report nearly 100 symptoms for more than 100 days". NBC News. Retrieved August 21, 2020.
- ↑ Shumaker, Erin (April 17, 2020). "What we know about coronavirus' long-term effects". ABC news.
- ↑ Bernstein, Lenny; Johnson, Carolyn Y.; Kaplan, Sarah; McGinley, Laurie (April 15, 2020). "Coronavirus destroys lungs. But doctors are finding its damage in kidneys, hearts and elsewhere". Washington Post.
- ↑ Lowenstein, Fiona; Davis, Hannah (April 13, 2020). "We Need to Talk About What Coronavirus Recoveries Look Like". New York Times.
- ↑ ME Association (May 2020). "MEA INFORMATION ON Post-viral fatigue (PVF) and Post-viral fatigue syndrome (PVFS) following coronovirus infection" (PDF). ME Association. Retrieved May 1, 2020.
- ↑ Physio for ME; Workwell Foundation; ME Association (May 2020). "Post Covid-19 Rehabilitation". Physiosforme. Retrieved May 2, 2020.
- ↑ Charles Shepherd (April 30, 2020). "Covid-19 and Post-viral Fatigue Syndrome by Dr Charles Shepherd". meassociation.org. Retrieved May 1, 2020.

