Canadian Consensus Criteria
The Canadian consensus criteria (CCC) or the Canadian working definition are a proposed clinical criteria for ME/CFS, published in 2003, and frequently used as a case definition in research.[1] The Canadian definition is a strictest diagnostic criteria, selecting a smaller group of patients than the Fukuda criteria and a more severely impaired population.[2] Adults are diagnosed after a minimum of six months of illness and children after a minimum of three months.
Definition
| A patient with ME/CFS will meet the criteria for fatigue, post-exertional malaise and/or fatigue, sleep dysfunction and pain; have two or more neurological/cognitive manifestations and one or more symptoms from two of the categories of (a) autonomic, (b) neuroendocrine and (c) immune manifestations; and adhere to item 7. | ||
| 1 | Fatigue Required |
The patient must have a significant degree of new onset, unexplained, persistent, or recurrent physical and mental fatigue that substantially reduces activity level. |
| 2 | Post-Exertional Malaise and/or Post-Exertional Fatigue Required |
There is an inappropriate loss of physical and mental stamina, rapid muscular and cognitive fatigability, post-exertional malaise and/or post-exertional fatigue and a tendency for other associated symptoms within the patient’s cluster of symptoms to worsen.
There is a pathologically slow recovery period – usually 24 hours or longer. |
| 3 | Sleep Dysfunction (*) Required |
There is unrefreshing sleep or sleep quantity or rhythm disturbances such as reversed or chaotic diurnal sleep rhythms. Note that patients without sleep dysfunction can still meet the diagnostic criteria if their illness began with an infection — see (*) below. |
| 4 | Pain (*) Required |
There is a significant degree of myalgia. Pain can be experienced in the muscles, and/or joints, and is often widespread and migratory in nature. Often there are significant headaches of new type, pattern or severity. Note that patients without pain can still meet the diagnostic criteria if their illness began with an infection — see (*) below. |
| 5 | Neurological / Cognitive Manifestations Two or more |
Two or more of the following difficulties should be present:
Ataxia, muscle weakness and fasciculations are common. There may be overload1 phenomena: cognitive overload, sensory overload (for example photophobia and hypersensitivity to noise) and/or emotional overload, which may lead to crash2 periods and/or anxiety. |
| 6 | At Least One Symptom From Two of the Following Three Categories (autonomic, neuroendocrine, immune) |
At Least One Symptom From Two of the Following Three Categories: |
(a) Autonomic Manifestations
| ||
(b) Neuroendocrine Manifestations
| ||
(c) Immune Manifestations
| ||
| 7 | The Illness Persists for at Least Six Months Required |
It usually has a distinct onset, (**) although it may be gradual. Preliminary diagnosis may be possible earlier. Three months is appropriate for children. |
To be included, the symptoms must have begun or have been significantly altered after the onset of this illness. It is unlikely that a patient will suffer from all symptoms in criteria 5 & 6. The disturbances tend to form symptom clusters that may fluctuate and change over time. Children often have numerous prominent symptoms but their order of severity tends to vary from day to day.
(*) There is a small number of patients who have no pain or sleep dysfunction, but no other diagnosis fits except ME/CFS. A diagnosis of ME/CFS can be entertained when this group has an infectious illness type onset.
(**) Some patients have been unhealthy for other reasons prior to the onset of ME/ CFS and lack detectable triggers at onset or have more gradual or insidious onset.
1"Overload" refers to hypersensitivities to stimuli that have changed from pre-illness status.
2 "Crash" refers to a temporary period of immobilizing physical and /or cognitive fatigue.
Idiopathic chronic fatigue
People with chronic fatigue (lasting at least six months) but not meeting the criteria for ME/CFS should be diagnosed with idiopathic chronic fatigue instead.
Authors
Bruce Carruthers, Anil Kumar Jain, Kenny de Meirleir, Daniel Peterson, Nancy Klimas, A Martin Lerner, Alison Bested, Pierre Flor-Henry, Pradip Joshi, A C Peter Powles, Jeffrey Sherkey, Marjorie van de Sande[4]
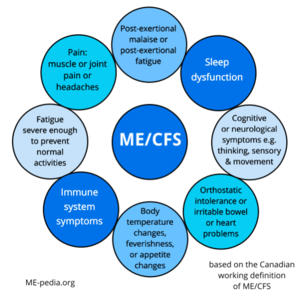
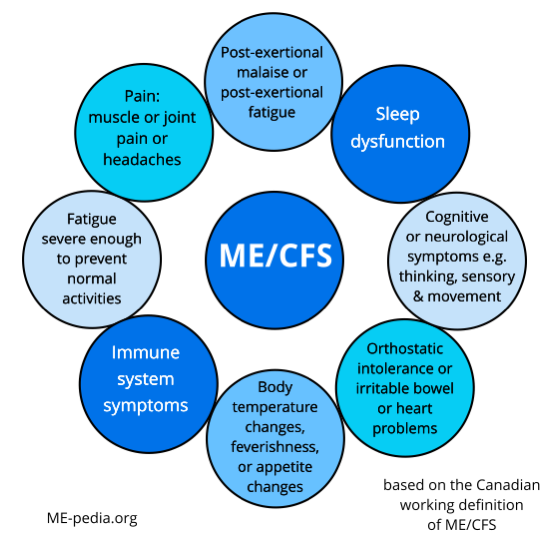
Diagram of ME/CFS symptoms
See also
Generally accepted criteria for diagnosis
- Canadian consensus criteria (CCC).[1] A diagnosis of moderate and severe forms of ME/CFS are accurately made using these criteria. Adults can be diagnosed at 6 months while pediatric cases are diagnosed at three months.
- International consensus criteria (ICC).[5] These criteria will accurately diagnose myalgic encephalomyelitis (ME). There is no requirement that the individual have symptoms for a specified period of time for diagnosis, as opposed to CCC, Fukuda, and SEID, which all require 6 months in adults.
- CDC Myalgic Encephalomyelitis/Chronic Fatigue Syndrome 2017 diagnostic criteria - originally known as the Systemic exertion intolerance disease (SEID) criteria[6][7] ME/CFS (SEID) is accurately diagnosed when the core symptoms are met. The Institute of Medicine report as a whole is a comprehensive review of the medical literature available at time of publication (2015). Adults can be diagnosed at 6 months while pediatric cases are diagnosed at three months.
Learn more
- A Clinical Case Definition and Guidelines for Medical Practitioners - An Overview of the Canadian Consensus Document[3] (the above 7 criteria are listed on page 2 of this document).
- Canadian Consensus Report - Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols[1] (full version of the Canadian consensus criteria).
- An Overview of the Canadian Consensus Document in French - Encéphalomyélite myalgique/syndrome de fatigue chronique: Définition clinique et lignes directrices à l’intention des médecins, Abrégé du Consensus canadien[8]
References
- ↑ 1.0 1.1 1.2 Carruthers, Bruce M.; Jain, Anil Kumar; De Meirleir, Kenny L.; Peterson, Daniel L.; Klimas, Nancy G.; Lerner, A. Martin; Bested, Alison C.; Flor-Henry, Pierre; Joshi, Pradip; Powles, AC Peter; Sherkey, Jeffrey A.; van de Sande, Marjorie I. (2003), "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols" (PDF), Journal of Chronic Fatigue Syndrome, 11 (2): 7–115, doi:10.1300/J092v11n01_02
- ↑ http://www.meaction.net/2015/12/10/norwegian-researchers-ask-what-exactly-is-m-e/
- ↑ 3.0 3.1 Carruthers, Bruce; van de Sande, Marjorie. "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Clinical Case Definition and Guidelines for Medical Practitioners - An Overview fo the Canadian Consensus Document" (PDF). Invest in ME Research. p. 4.
Physical or mental exertion often causes debilitating malaise and/or fatigue, generalized pain, deterioration of cognitive functions, and worsening of other symptoms that may occur immediately after activity or be delayed. Patients experience rapid muscle fatigue and lack endurance.
- ↑ http://sacfs.asn.au/download/consensus_overview_me_cfs.pdf
- ↑ Carruthers, Bruce M.; van de Sande, Marjorie I.; De Meirleir, Kenny L.; Klimas, Nancy G.; Broderick, Gordon; Mitchell, Terry; Staines, Donald; Powles, A.C. Peter; Speight, Nigel; Vallings, Rosamund; Bateman, Lucinda; Baumgarten-Austrheim, Barbara; Bell, David; Carlo-Stella, Nicoletta; Chia, John; Darragh, Austin; Jo, Daehyun; Lewis, Donald; Light, Alan; Marshall-Gradisnik, Sonya; Mena, Ismael; Mikovits, Judy; Miwa, Kunihisa; Murovska, Modra; Pall, Martin; Stevens, Staci (August 22, 2011). "Myalgic encephalomyelitis: International Consensus Criteria". Journal of Internal Medicine. 270 (4): 327–338. doi:10.1111/j.1365-2796.2011.02428.x. ISSN 0954-6820. PMC 3427890. PMID 21777306.
- ↑ "Symptoms | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. January 27, 2021. Retrieved February 25, 2021.
- ↑ Clayton, Ellen Wright; Alegria, Margarita; Bateman, Lucinda; Chu, Lily; Cleeland, Charles; Davis, Ronald; Diamond, Betty; Ganiats, Theodore; Keller, Betsy; Klimas, Nancy; Lerner, A. Martin; Mulrow, Cynthia; Natelson, Benjamin; Rowe, Peter; Shelanski, Michael (2015). "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome - Redefining an Illness" (PDF). National Academies.
- ↑ Carruthers, Bruce; van de Sande, Marjorie. "Encéphalomyélite myalgique /syndrome de fatigue chronique: Définition cliniqueet lignes directricesà l'intention des médecins - Abrégé duConsensus canadien" (PDF). IACFS/ME (in français).

