Neurology of ME/CFS
Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is a complex neurological disease,[1] that is often considered to be neuroimmune, or more recently, neurovascular.[2][3] Myriad neurological abnormalities have been found, such as changes in brain structure and metabolism, and autonomic nervous system dysfunction. Neuroinflammation, indicated by elevated brain lactate and choline, is suggested as a key mechanism, though evidence is mixed.[4][5]
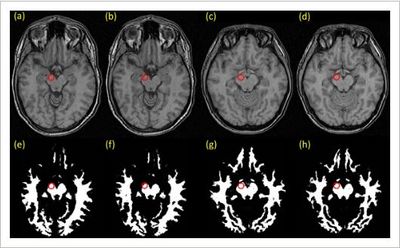
Brain imaging[edit | edit source]
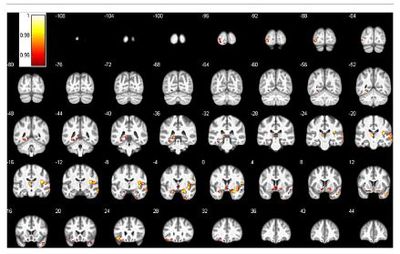
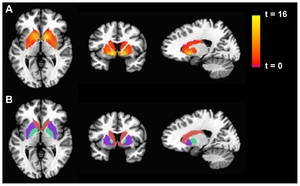
Source: Miller et al. (2014). PLoS ONE 9(5): e98156. doi:10.1371/journal.pone.0098156
Spine[edit | edit source]
Neural strain[edit | edit source]
In a study of neuromuscular strain in ME/CFS, 60 people with ME/CFS and 20 healthy controls randomly were assigned to undergo a neuromuscular strain maneuver or sham maneuver. Those with ME/CFS in the strain condition group had significantly increased symptoms for up to 24 hours.[8]
Causes of neurological symptoms[edit | edit source]
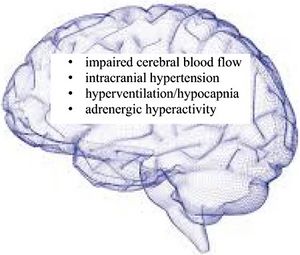
Source:
Wirth, K.J., Scheibenbogen, C. & Paul, F. An attempt to explain the neurological symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. J Transl Med 19, 471 (2021). https://doi.org/10.1186/s12967-021-03143-3
Causes of neurological symptoms in ME/CFS include:
- hyperventilation/hypnocapnia (reduced carbon dioxide levels in the blood)
- intracranial hypertension (increased pressure within the skull and around brain)
- reduced blood flow to the brain
- brain inflammation may also be a factor[2]
These can explain cognitive impairment, brain fog, headache, psychomotor slowing, ataxia and loss of coordination of movements, hypersensitivity, sleep disturbances and dysautonomia.[2]
Neurovascular symptoms[edit | edit source]
Research by Wirth, Scheibenbogen, and colleagues has found evidence of neurovascular abnormalities which are potentially the key cause of most neurological symptoms in ME/CFS, in particular ß2 adrenergic receptor antibodies.[2] Evidence of abnormal neurovascular coupling (NVC) has also been found in ME/CFS patients.[3]
Notable studies[edit | edit source]
- 2021, An attempt to explain the neurological symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[2] - (Full text)
- 2022, Neurovascular dysregulation and acute exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome: a randomized, placebo-controlled trial of pyridostigmine[3] - (Full text)
Talks and interviews[edit | edit source]
- 2016, 77. ME & the brain, part 1 / ME & de hersenen, deel 1 - Dr. Neil Harrison[9]
- 2016, 78. ME & the brain, part 2 / ME & de hersenen, deel 2 - Dr. Neil Harrison[10]
- 2016, 79. ME & inflammation, part 1 / ME & inflammatie, deel 1 - Dr Harrison[11]
- 2018, ME/CFS Involves Brain Inflammation: Results from a Ramsay Pilot Study, sponsored by Solve ME/CFS Initiative[12]
See also[edit | edit source]
- Brain
- Basal ganglia
- Microglia
- QEEG
- Neuroinflammation
- List of abnormal findings in chronic fatigue syndrome and myalgic encephalomyelitis
Researchers[edit | edit source]
Learn more[edit | edit source]
- 2016, Laggard: Is an Under-Active Brain the Problem in Chronic Fatigue Syndrome (ME/CFS)[13]
- 2017, Reference List of Neurology studies ME CFS 2017.pdf[14]
- 2018, Brain on Fire: Widespread Neuroinflammation Found in Chronic Fatigue Syndrome (ME/CFS)[15]
- 2019, Brain Imaging and Behavior publication from Dr. Jarred Younger’s SMCI Ramsay pilot study supports involvement of neuroinflammation in ME/CFS[16]
References[edit | edit source]
- ↑ World Health Organization. "Postviral fatigue syndrome". ICD-11 - Mortality and Morbidity Statistics. Retrieved October 14, 2018.
- ↑ 2.0 2.1 2.2 2.3 2.4 Wirth, Klaus J.; Scheibenbogen, Carmen; Paul, Friedemann (November 22, 2021). "An attempt to explain the neurological symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Journal of Translational Medicine. 19 (1): 471. doi:10.1186/s12967-021-03143-3. ISSN 1479-5876. PMC 8607226. PMID 34809664.
- ↑ 3.0 3.1 3.2 Joseph, Phillip; Pari, Rosa; Miller, Sarah; Warren, Arabella; Stovall, Mary Catherine; Squires, Johanna; Chang, Chia-Jung; Xiao, Wenzhong; Waxman, Aaron B.; Systrom, David M. (November 2022). "Neurovascular Dysregulation and Acute Exercise Intolerance in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". CHEST. 162 (5): 1116–1126. doi:10.1016/j.chest.2022.04.146. ISSN 0012-3692.
- ↑ Grach, Stephanie L.; Seltzer, Jaime; Chon, Tony Y.; Ganesh, Ravindra (2023-10). "Diagnosis and Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Mayo Clinic Proceedings. 98 (10): 1544–1551. doi:10.1016/j.mayocp.2023.07.032. ISSN 0025-6196. Check date values in:
|date=(help) - ↑ Lee, Jin-Seok; Sato, Wakiro; Son, Chang-Gue (2024-02). "Brain-regional characteristics and neuroinflammation in ME/CFS patients from neuroimaging: A systematic review and meta-analysis". Autoimmunity Reviews. 23 (2): 103484. doi:10.1016/j.autrev.2023.103484. ISSN 1568-9972. Check date values in:
|date=(help) - ↑ Shan, ZY; Kwiatek, R; Burnet, R; Del Fante, P; Staines, DR; Marshall-Gradisnik, SM; Barnden, LR (April 28, 2016), "Progressive brain changes in patients with chronic fatigue syndrome: A longitudinal MRI study", Journal of magnetic resonance imaging: JMRI, doi:10.1002/jmri.25283, PMID 27123773
- ↑ Finkelmeyer, Andreas; He, Jiabao; Maclachlan, Laura; Watson, Stuart; Gallagher, Peter; Newton, Julia L.; Blamire, Andrew M. (2018), "Grey and white matter differences in Chronic Fatigue Syndrome – A voxel-based morphometry study", NeuroImage: Clinical, 17: 24-30, doi:10.1016/j.nicl.2017.09.024, PMID 29021956
- ↑ Violand, Richard L.; Thompson, Carol B.; Moni, Malini; Marden, Colleen L.; Jasion, Samantha E.; Lauver, Megan; Fontaine, Kevin R.; Rowe, Peter C. (July 18, 2016). "Neuromuscular Strain Increases Symptom Intensity in Chronic Fatigue Syndrome". PLOS ONE. 11 (7): e0159386. doi:10.1371/journal.pone.0159386. ISSN 1932-6203.
- ↑ "77. ME & the brain, part 1 / ME & de hersenen, deel 1 - Dr. Neil Harrison". YouTube. Wetenschap voor Patienten - ME/cvs Vereniging. April 5, 2016.
- ↑ "78. ME & the brain, part 2 / ME & de hersenen, deel 2 - Dr. Neil Harrison". YouTube. Wetenschap voor Patienten - ME/cvs Vereniging. April 19, 2016.
- ↑ Harrison, Neil (May 3, 2016). "79. ME & inflammation, part 1 / ME & inflammatie, deel 1 - Dr Harrison". YouTube. Wetenschap voor Patienten - ME/cvs Vereniging.
- ↑ "ME/CFS Involves Brain Inflammation: Results from a Ramsay Pilot Study". YouTube. SolveCFS. December 14, 2018.
- ↑ Johnson, Cort (July 25, 2016). "Laggard: Is an Under-Active Brain the Problem in Chronic Fatigue Syndrome (ME/CFS)". Health Rising. Retrieved November 29, 2018.
- ↑ Chapman, Suzy (2017). "Reference List of Neurology studies - ME CFS 2017" (PDF). Dropbox. Retrieved November 29, 2018.
- ↑ Johnson, Cort (September 24, 2018). "Brain on Fire: Widespread Neuroinflammation Found in Chronic Fatigue Syndrome (ME/CFS)". Health Rising. Retrieved November 29, 2018.
- ↑ "Brain Imaging and Behavior publication from Dr. Jarred Younger's SMCI Ramsay pilot study supports involvement of neuroinflammation in ME/CFS". go.solvecfs.org. Retrieved January 17, 2019.

