Dysbiosis
This article needs cleanup to meet MEpedia's guidelines. The reason given is: References needed (May 2019) |
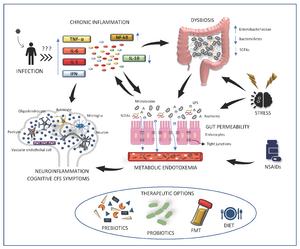
Dysbiosis is an imbalance in the microbial ecosystem in a part of the body, usually the gut, that is associated with disease processes.[1]
Gut microbiota must be normal for immune homeostasis.[1]
Causes of gut dysbiosis
Psychological stress
Psychological stress can alter the gut microbiota, decreasing numbers of Bifidobacteria and Lactobacilli.[2]
Infection
Antibiotic use
Antibiotics negatively alter the healthy combination of phyla within the gut microbiota, e.g. by reducing the ratio of Firmicutes to Bacteroidetes, and increasing levels of Proteobacteria.[3] The antibiotics ciprofloxacin, vancomycin, ampicillin, cefazolin and cefoperazone reduce the diversity of gut microbiota, although in one study ciprofloxacin increased rather than decreased the Firmicutes to Bacteroidetes ratio.[3] Combination antibiotics cause more severe dysbiosis than using a single antibiotic.[3]
Lifetime antibiotic use alters the gut microbiome and is a proposed risk factor for ME/CFS.[4]
Long-term probiotic use
Degirolamo et al (2014) states that Bifidobacterium and Lactobacillus probiotic strains may provide additional good bacteria, reducing the harm from antibiotics, but in long term use may also disturb the balance of gut microbiota.[3]
ME/CFS
Source: Varesi, A; Deumer, U-S; Ananth, S; Ricevuti, G (October 29, 2021). "The Emerging Role of Gut Microbiota in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Current Evidence and Potential Therapeutic Applications". Journal of Clinical Medicine. 10 (21): 5077. doi: 10.3390/jcm10215077]
There is evidence that dysbiosis or an imbalance in the microbial ecology of the gut plays a role in the symptoms of ME/CFS. On average, ME/CFS patients have lower levels of Bifidobacteria, Escherichia coli and higher levels of aerobic bacteria,[2] in particular Enterococcus and Streptococcus species.[5] The latter produce D-lactate, a form of lactic acid only produced by non-human cells that is poorly metabolized in humans. D lactate is associated with a wide variety of cognitive and neurological symptoms, such as in patients who suffer from D-lactic acidosis. A study found that higher levels of Enterococcus bacteria in CFS patients were associated with more severe neurological and cognitive dysfunction.[6][2]
"In one study researchers were able to classify 83% of the ME/CFS patients correctly based on their dysbiosis in gut and increased inflammatory markers in blood as a consequence of microbial translocation (13)."[4]
A study by Pimentel et al. (2000) found that 77% of CFS patients may suffer from small intestinal bacterial overgrowth (SIBO), which is a significantly higher rate than in the general population.[7]
One hypothesized consequence of dysobiosis is an overproduction of hydrogen sulfide (H2S) by pathogenic bacteria. H2S can inhibit mitochondrial respiration by blocking cytochrome c oxidase.[citation needed]
Sheedy et al. (2009) studied Norwegian and Belgian ME/CFS patients and found significantly decreased proportions of Firmicutes genera Holdemania and increased proportions of bacteroidetes genera Alistipes in the Norwegian but not the Belgian sample. Significantly increased proportions of Firmicutes genera Lactonifactor were found in both.[8]
Notable studies
- 2003, Chronic fatigue syndrome: lactic acid bacteria may be of therapeutic value[2] - (Full text)
- 2007, Normalization of the increased translocation of endotoxin from gram negative enterobacteria (leaky gut) is accompanied by a remission of chronic fatigue syndrome[9] - (Full text)
- 2007, Increased serum IgA and IgM against LPS of enterobacteria in chronic fatigue syn- drome (CFS): indication for the involvement of gram-negative enterobacteria in the etiology of CFS and for the presence of an increased gut-intestinal permeability[10] - (Full text)
- 2009, Increased d-lactic Acid intestinal bacteria in patients with chronic fatigue syndrome[5] - (Full text)
- 2013, High-throughput 16S rRNA gene sequencing reveals alterations of intestinal microbiota in myalgic encephalomyelitis/chronic fatigue syndrome patients[8] - (Full text)
- 2015, Increased expression of activation antigens on CD8+ T lymphocytes in Myalgic Encephalomyelitis/chronic fatigue syndrome: inverse associations with lowered CD19+ expression and CD4+/CD8+ ratio, but no associations with (auto) immune, leaky gut, oxidative and nitrosative stress biomarkers[11] - (Abstract)
- 2015, Changes in gut and plasma microbiome following exercise challenge in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)[12] - (Full text)
- 2016, The role of microbiota and intestinal permeability in the pathophysiology of autoimmune and neuroimmune processes with an emphasis on inflammatory bowel disease type 1 diabetes and chronic fatigue syndrome[13] - (Full text)
- 2016, A role for the intestinal microbiota and virome in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)[14] - (Full text)
- 2016, The association of fecal microbiota and fecal, blood serum and urine metabolites in myalgic encephalomyelitis/chronic fatigue syndrome[15] - (Full text)
- 2016, Reduced Diversity and Altered Composition of the Gut Microbiome in Individuals With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[16] - (Full text)
- 2017, Fecal Metagenomic Profiles in Subgroups of Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[17] - (Full text)
- 2018, The Emerging Role of Gut Microbiota in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Current Evidence and Potential Therapeutic Applications[18] - (Full text)
- 2018, A role for a leaky gut and the intestinal microbiota in the pathophysiology of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)[19] - (Thesis - Full text)
- 2020, The “Leaky Gut”: Tight Junctions but Loose Associations?[20] - (Full text)
- 2020, Mitochondria and immunity in chronic fatigue syndrome[21] - (Full text)
- 2021, The Emerging Role of Gut Microbiota in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Current Evidence and Potential Therapeutic Applications[22] - (Full text)
- 2021, Tryptophan Metabolites, Cytokines, and Fatty Acid Binding Protein 2 in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[23] - (Full text)
- 2022, The Gut Microbiome in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS)[4] - (Full text)
See also
- Intestinal permeability (leaky gut)
- Dr Markov's chronic bacterial intoxication syndrome (CBIS) theory of ME/CFS (Dr Markov has evidence that ME/CFS is caused by a dysbiosis in the kidneys)
Learn more
- 2017, Intestinal dysbiosis in ME/CFS patients - Vincent Racaniello, Virology blog
References
- ↑ 1.0 1.1 Wu, Gary D.; Lewis, James D. (July 1, 2013). "Analysis of the Human Gut Microbiome and Association With Disease". Clinical Gastroenterology and Hepatology. 11 (7): 774–777. doi:10.1016/j.cgh.2013.03.038. ISSN 1542-3565.
- ↑ 2.0 2.1 2.2 2.3 Logan, Alan C; Venket Rao, A; Irani, Dinaz (June 1, 2003). "Chronic fatigue syndrome: lactic acid bacteria may be of therapeutic value". Medical Hypotheses. 60 (6): 915–923. doi:10.1016/S0306-9877(03)00096-3. ISSN 0306-9877.
- ↑ 3.0 3.1 3.2 3.3 Khan, Tariq Jamal; Hasan, Mohammed Nihal; Azhar, Esam I.; Yasir, Muhammad (March 1, 2019). "Association of gut dysbiosis with intestinal metabolites in response to antibiotic treatment". Human Microbiome Journal. 11: 100054. doi:10.1016/j.humic.2018.11.004. ISSN 2452-2317.
- ↑ 4.0 4.1 4.2 König, Rahel S.; Albrich, Werner C.; Kahlert, Christian R.; Bahr, Lina Samira; Löber, Ulrike; Vernazza, Pietro; Scheibenbogen, Carmen; Forslund, Sofia K. (2022). "The Gut Microbiome in Myalgic Encephalomyelitis (ME)/Chronic Fatigue Syndrome (CFS)". Frontiers in Immunology. 12. doi:10.3389/fimmu.2021.628741/full. ISSN 1664-3224. PMC 8761622. PMID 35046929.
- ↑ 5.0 5.1 Sheedy, John R; Wettenhall, Richard EH; Scanlon, Denis; Gooley, Paul R; Lewis, Donald P; McGregor, Neil; Stapleton, David I; Butt, Henry L; De Meirleir, Kenny L (July 2009). "Increased d-lactic Acid intestinal bacteria in patients with chronic fatigue syndrome". In Vivo. 23 (4): 621–628. PMID 19567398.
- ↑ Ring, Jenny, ed. (2002). Myalgic encephalopathy--chronic fatigue syndrome : the medical practitioners'--challenge informed accurate diagnosis : proceedings of international clinical and scientific meeting, Sydney, Australia, 1-2, December 2001. Bowral, Australia: Alison Hunter Memorial Foundation. ISBN 9780958186506. OCLC 52595685.
- ↑ Pimentel, M; Hallegua, D; Chow, EJ; Wallace, D; Bonorris, G; Lin, HC (April 1, 2000). "Eradication of small intestinal bacterial overgrowth decreases symptoms in chronic fatigue syndrome: A double blind, randomized study". Gastroenterology. 118 (4): 414. doi:10.1016/S0016-5085(00)83765-8.
- ↑ 8.0 8.1 Frémont, Marc; Coomans, Danny; Massart, Sebastien; De Meirleir, Kenny (August 1, 2013). "High-throughput 16S rRNA gene sequencing reveals alterations of intestinal microbiota in myalgic encephalomyelitis/chronic fatigue syndrome patients". Anaerobe. 22: 50–56. doi:10.1016/j.anaerobe.2013.06.002. ISSN 1075-9964.
- ↑ Maes, Michael; Coucke, Francis; Leunis, Jean-Claude (December 2007). "Normalization of the increased translocation of endotoxin from gram negative enterobacteria (leaky gut) is accompanied by a remission of chronic fatigue syndrome". Neuro Endocrinology Letters. 28 (6): 739–744. ISSN 0172-780X. PMID 18063928.
- ↑ Maes, Michael; Mihaylova, Ivana; Leunis, Jean-Claude (April 1, 2007). "Increased serum IgA and IgM against LPS of enterobacteria in chronic fatigue syndrome (CFS): Indication for the involvement of gram-negative enterobacteria in the etiology of CFS and for the presence of an increased gut–intestinal permeability". Journal of Affective Disorders. 99 (1): 237–240. doi:10.1016/j.jad.2006.08.021. ISSN 0165-0327.
- ↑ Maes, Michael; Bosmans, Eugene; Kubera, Marta (2015). "Increased expression of activation antigens on CD8+ T lymphocytes in Myalgic Encephalomyelitis/chronic fatigue syndrome: inverse associations with lowered CD19+ expression and CD4+/CD8+ ratio, but no associations with (auto)immune, leaky gut, oxidative and nitrosative stress biomarkers". Neuro Endocrinology Letters. 36 (5): 439–446. ISSN 0172-780X. PMID 26707044.
- ↑ Shukla, Sanjay K.; Cook, Dane; Meyer, Jacob; Vernon, Suzanne D.; Le, Thao; Clevidence, Derek; Robertson, Charles E.; Schrodi, Steven J.; Yale, Steven; Frank, Daniel N. (December 18, 2015). "Changes in Gut and Plasma Microbiome following Exercise Challenge in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". PLOS ONE. 10 (12): e0145453. doi:10.1371/journal.pone.0145453. ISSN 1932-6203. PMC 4684203. PMID 26683192.
- ↑ Morris, Gerwyn; Berk, Michael; Carvalho, André F.; Caso, Javier R.; Sanz, Yolanda; Maes, Michael (2016). "The Role of Microbiota and Intestinal Permeability in the Pathophysiology of Autoimmune and Neuroimmune Processes with an Emphasis on Inflammatory Bowel Disease Type 1 Diabetes and Chronic Fatigue Syndrome". Current Pharmaceutical Design. 22 (40): 6058–6075. doi:10.2174/1381612822666160914182822. ISSN 1873-4286. PMID 27634186.
- ↑ Morris, Gerwyn; Berk, Michael; Carvalho, André F.; Caso, Javier R.; Sanz, Yolanda; Maes, Michael (2016). "The Role of Microbiota and Intestinal Permeability in the Pathophysiology of Autoimmune and Neuroimmune Processes with an Emphasis on Inflammatory Bowel Disease Type 1 Diabetes and Chronic Fatigue Syndrome". Current Pharmaceutical Design. 22 (40): 6058–6075. doi:10.2174/1381612822666160914182822. ISSN 1873-4286. PMID 27634186.
- ↑ Armstrong, Christopher W.; McGregor, Neil R.; Lewis, Donald P.; Butt, Henry L.; Gooley, Paul R. (December 12, 2016). "The association of fecal microbiota and fecal, blood serum and urine metabolites in myalgic encephalomyelitis/chronic fatigue syndrome". Metabolomics. 13 (1): 8. doi:10.1007/s11306-016-1145-z. ISSN 1573-3890.
- ↑ Giloteaux, Ludovic; Goodrich, Julia K.; Walters, William A.; Levine, Susan M.; Ley, Ruth E.; Hanson, Maureen R. (June 23, 2016). "Reduced diversity and altered composition of the gut microbiome in individuals with myalgic encephalomyelitis/chronic fatigue syndrome". Microbiome. 4 (1): 30. doi:10.1186/s40168-016-0171-4. ISSN 2049-2618. PMC 4918027. PMID 27338587.
- ↑ Nagy-Szakal, Dorottya; Williams, Brent L.; Mishra, Nischay; Che, Xiaoyu; Lee, Bohyun; Bateman, Lucinda; Klimas, Nancy G.; Komaroff, Anthony L.; Levine, Susan; Montoya, Jose G.; Peterson, Daniel L. (April 26, 2017). "Fecal metagenomic profiles in subgroups of patients with myalgic encephalomyelitis/chronic fatigue syndrome". Microbiome. 5 (1): 44. doi:10.1186/s40168-017-0261-y. ISSN 2049-2618. PMC 5405467. PMID 28441964.
- ↑ Varesi, Angelica; Deumer, Undine-Sophie; Ananth, Sanjana; Ricevuti, Giovanni (October 29, 2021). "The Emerging Role of Gut Microbiota in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Current Evidence and Potential Therapeutic Applications". Journal of Clinical Medicine. 10 (21): 5077. doi:10.3390/jcm10215077. ISSN 2077-0383. PMC 8584653. PMID 34768601.
- ↑ Vipond, Daniel (2018). "A role for a leaky gut and the intestinal microbiota in the pathophysiology of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)". University of East Anglia.
- ↑ Hollander, Daniel; Kaunitz, Jonathan D. (May 2020). "The "Leaky Gut": Tight Junctions but Loose Associations?". Digestive diseases and sciences. 65 (5): 1277–1287. doi:10.1007/s10620-019-05777-2. ISSN 0163-2116. PMC 7193723. PMID 31471860.
- ↑ Anderson, G.; Maes, M. (December 20, 2020). "Mitochondria and immunity in chronic fatigue syndrome". Progress in Neuro-Psychopharmacology and Biological Psychiatry. 103: 109976. doi:10.1016/j.pnpbp.2020.109976. ISSN 0278-5846. PMID 32470498.
- ↑ Varesi, Angelica; Deumer, Undine-Sophie; Ananth, Sanjana; Ricevuti, Giovanni (October 29, 2021). "The Emerging Role of Gut Microbiota in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS): Current Evidence and Potential Therapeutic Applications". Journal of Clinical Medicine. 10 (21): 5077. doi:10.3390/jcm10215077. ISSN 2077-0383. PMC 8584653. PMID 34768601.
- ↑ Simonato, Manuela; Dall’Acqua, Stefano; Zilli, Caterina; Sut, Stefania; Tenconi, Romano; Gallo, Nicoletta; Sfriso, Paolo; Sartori, Leonardo; Cavallin, Francesco; Fiocco, Ugo; Cogo, Paola (November 19, 2021). "Tryptophan Metabolites, Cytokines, and Fatty Acid Binding Protein 2 in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Biomedicines. 9 (11): 1724. doi:10.3390/biomedicines9111724. ISSN 2227-9059. PMC 8615774. PMID 34829952.

