Natural killer cell
Natural killer (NK) cells are a type of white blood cell that forms part of the innate immune system. Their function involves the recognition and destruction of tumor and virally infected cells.[1] Numerous studies have found evidence of reduced natural killer cell function in patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).[2][3][4][5][6]
Function
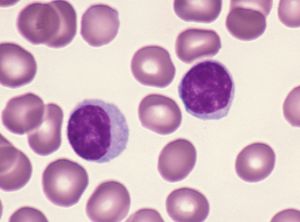
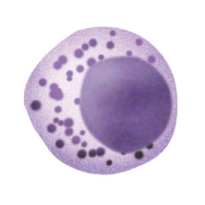
The majority of lymphocytes, a leucocyte subgroup, are B or T cells but approximately 15% of the lymphocyte population lack B or T cell receptors; these are NK cells.[1] The latter develop in the bone marrow and have a half-life of approximately 7 days.[7] Most NK cells are found in the blood, spleen or liver and enter tissues at sites of inflammation following infection. There are two NK cell subgroups dependent on the expression of either CD16 (FcγRIII) or CD56 cell surface receptors.[8]
NK cells play a major role in eliminating virally infected cells. Following infection, viruses block cell synthesis of major histocompatibility complex class I (MHCI) molecules.[1] Presentation of MHC class I molecules at an infected cell’s surface is used by cytotoxic T cells (Tc cells) to target and destroy the cell. By preventing MHC class I presentation, viruses ensure the cell is unrecognised and escapes elimination by Tc cells: this is where NK cells prove vitally important in the body’s immune response.[1] NK cells express specialized receptors – killer inhibitory receptors (KIRs) – which can identify MHC class I molecules. Following recognition of the MHC class I molecule, the KIR inhibits NK cell cytotoxic activity and destruction of the target.[1] Virally infected cells, lacking the surface expression of MHC class I molecules, can be targeted and eliminated by NK cells.
NK cells can also target virally infected cells via expression of the IgG receptor CD16. This receptor binds antibodies attached to viral molecules on infected cell surfaces in a process called antibody-dependent cell mediated cytotoxicity (ADCC).[1]
NK Cell Cytotoxic Mechanisms
NK cells can terminate an infected cell via several mechanisms including:
- Direct cell-to-cell contact
- Cytokine synthesis and release[1]
As Large Granular Lymphocytes (LGLs), NK cells utilize their granular structure to kill infected cells. On fusing with virally infected cells’ plasma membranes, granules release their contents into the cell[1]. These contents include the protein perforin, which perforates the infected cell's membrane, enabling entry of specialized ‘suicide’ enzymes, including granzyme B, into the virally infected cell; these initiate apoptosis (programmed cell death).[1][7] Granzymes can also damage the infected cell directly and play a vital role in virally infected cell destruction. Apoptosis can also be triggered via the attachment of Fas ligands (FasL) on the NK cell surface to Fas proteins on the target cell, activating apoptosis-inducing signalling.[7]
NK cells express two receptor types:
- Activating
- Inhibitory
Activating receptors induce NK cells to eliminate infected cells, while inhibitory receptors block killing mechanisms[7]. Resting NK cells synthesize cytokines and are capable of destroying virally infected cells but activated NK cells produce higher numbers of cytokines and are more efficient at eliminating infected cells[7].
Factors Leading to NK cell Activation
Several elements can produce NK cell activation, including:
- The detection of lipopolysaccharide (LPS, a bacterial cell wall constituent)
LPS is bound by NK cell surface receptors, inducing responses including IFN-γ synthesis, which can prepare macrophages for activation. Following activation, macrophages synthesize TNF (tumour necrosis factor), which binds a macrophage’s own surface receptors[7]. This initiates IL-12 (interleukin-12) activation. The combination of TNF and IL-12 expression induces increased NK cell synthesis of IFN-γ leading to more macrophage priming, an example of an enhanced immune response via a positive feedback loop[7]. TNF synthesis by macrophages also upregulates IL-2 expression on NK cell surfaces, NK cells respond to their own IL-2 synthesis and undergo rapid division[7].
In human disease
ME/CFS
Numerous studies of myalgic encephalomyelitis and chronic fatigue syndrome have found evidence of reduced natural killer cell function.[2][3][4][5][6] Some studies have showed natural killer cell function correlates with illness severity.[9] One study found increased differentiation in NK cells.[10] Inconsistency in laboratory preparation and analysis have made it difficult to compare results between laboratories or use NK function as a consistent biomarker.[citation needed]
In 2015, David Strayer, et al., published "Low NK Cell Activity in Chronic Fatigue Syndrome (CFS) and Relationship to Symptom Severity," in the Journal of Clinical & Cellular Immunology. The study reviewed previous studies that concluded that the more decreased the natural killer cell cytotoxicity was in patients, the greater the severity of the disease. The study also reported that in vitro exposure of peripheral blood mononuclear cells from CFS patients (who fulfilled both the CDC 1988 and 1994 case definitions) to Ampligen increased natural killer cell cytotoxicity 100-178%. The conclusion of the study was that low NK cell cytotoxicity is commonly seen in CFS and was associated with increased symptom severity.[11]
Causes
The following mechanisms have some degree of evidence that they cause NK dysfunction in ME:
- Altered MAPK signaling.[12][13]
- Calcium channel dysfunction.[14]
- MicroRNAs. Transfecting primary NK cells with microRNAs that were upregulated in ME, resulted in gene expression changes consistent with NK cell activation but diminished cytotoxicity.[15]
Relevance
It's currently unknown what the consequences are of NK dysfunction in ME, and how significant they are. One potential consequences is impaired clearance of pathogens.
Multiple sclerosis
In 2009 a team led by Dr Hugh Brady from the Department of Life Sciences at Imperial College London, identified a master gene E4bp4 which causes blood stem cells to turn into disease-fighting 'Natural Killer' autoimmune cells. Using a mouse model scientists successfully 'knocked out' the gene known as E4bp4, creating the world's first animal model entirely lacking 'Natural Killer' cells, leaving all other blood cells and immune cells intact. This breakthrough model should help solve the mystery of the role that Natural Killer cells play in autoimmune diseases, such as diabetes and multiple sclerosis. This could now lead to new ways of treating these conditions with a drugs which will react with the protein expressed by their E4bp4 gene.[16][17]
Brain and spinal cord injury
Low NK function is associated with pathologies and experimental models of neural strain.[citation needed], including spinal cord injury.[citation needed]
Modulating NK function
Probiotics
Some probiotics have been shown to increase NK function, including Lactobacillus rhamnosus HN001,[18] Bifidobacterium lactis HN019[18][19] and Lactobacillus casei Shirota[20][21][22]
AHCC
In animal models, Active Hexose Correlated Compound (AHCC) has been show to increase NK activity.[23] A randomized, controlled trial of healthy volunteers found no significant effect of AHCC on NK function.[24]
Stress
There is evidence in humans and animal models that psychological stress[25][26] and physical stress, for example surgery,[27][28] decreases NK function and promotes tumor development and metastasis.[28] Mindfulness based meditation or stress reduction may increase natural killer cell function.[29]
Smoking
Smoking decreases natural killer cell function.[22]
Ampligen
In 2015, David Strayer, et al., published a study that in vitro exposure of peripheral blood mononuclear cells from CFS patients (fulfilling both the CDC 1988 and 1994 case definitions) to Ampligen increased Natural Killer cell cytotoxicity 100-178%.[11]
Nutritional deficiencies
Vitamin B12 deficiency may be associated with decreased natural killer cell activity.[30]
Notable studies
- 1987, Phenotypic and functional deficiency of natural killer cells in patients with chronic fatigue syndrome (Abstract)
- 2003, Predictive immunophenotypes: Disease-related profile in chronic fatigue syndrome (Full Text)
- 2015, Low NK Cell Activity in Chronic Fatigue Syndrome (CFS) and Relationship to Symptom Severity (Full Text)
- May 2015 - Characterisation of cell functions and receptors in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis (CFS/ME), BMC Immunology, 2015 16:35
- May 2015 - Examination of Single Nucleotide Polymorphisms (SNPs) in Transient Receptor Potential (TRP) Ion Channels in Chronic Fatigue Syndrome Patients[31] (small study - 115 people with ME/CFS)
- May 2015 - Examination of Single Nucleotide Polymorphisms (SNPs) in Transient Receptor Potential (TRP) Ion Channels in Chronic Fatigue Syndrome Patients, Immunology and Immunogenetics Insights, 2015:7 1-6. (small study - 115 people with ME/CFS)
- Dec 2015, Pilot Study of Natural Killer Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis[32] (Abstract)
- Jan 2016, Genotype Frequencies of Transient Receptor Potential Melastatin M3 Ion Channels and Acetylcholine Muscarinic M3 Receptor Gene Polymorphisms in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Patients Genotype Frequencies of Transient Receptor Potential Melastatin M3 Ion Channels and Acetylcholine Muscarinic M3 Receptor Gene Polymorphisms in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Patients[33] (Full text)
- Apr 2016, ERK1/2, MEK1/2 and p38 downstream signalling molecules impaired in CD56dimCD16+ and CD56brightCD16dim/− natural killer cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients[13] (Full text)
- May 2016, Novel identification and characterisation of Transient receptor potential melastatin 3 ion channels on Natural Killer cells and B lymphocytes: effects on cell signalling in Chronic fatigue syndrome/Myalgic encephalomyelitis patients[34] (Full text)
- 2016, Dysregulation of Protein Kinase Gene Expression in NK Cells from Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Patients[12] (Full Text)
- 2016, Natural killer cells and single nucleotide polymorphisms of specific ion channels and receptor genes in myalgic encephalomyelitis/chronic fatigue syndrome (Full Text)
- 2016, Killer Cell Immunoglobulin-like Receptor Genotype and Haplotype Investigation of Natural Killer Cells from an Australian Population of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Patients (Full Text)
- 2016, MicroRNAs hsa-miR-99b, hsa-miR-330, hsa-miR-126 and hsa-miR-30c: Potential Diagnostic Biomarkers in Natural Killer (NK) Cells of Patients with Chronic Fatigue Syndrome (CFS)/ Myalgic Encephalomyelitis (ME)[15]
- 2018, Association of T and NK cell phenotype with the diagnosis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)[35] (Abstract)
- 2018, Rituximab impedes natural killer cell function in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients: A pilot in vitro investigation[36] (Full Text)
- Aug 2018, Loss of Transient Receptor Potential Melastatin 3 ion channel function in natural killer cells from Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients[37] (Full text)
- May 2019, Validation of impaired Transient Receptor Potential Melastatin 3 ion channel activity in natural killer cells from Chronic Fatigue Syndrome/ Myalgic Encephalomyelitis patients[38] (Full text)
Learn more
- Wikipedia - Natural killer cell
- Crash Course - The Immune System Part 1
- 2016, What was the research into immune responses in CFS/M.E. you funded about?
- 2016, Immune cell 'switch' discovery raises hopes in cancer fight[39]
See also
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Male, D (2007), Immunology, Milton Keynes: The Open University
- ↑ 2.0 2.1 Barker, Edward; Fujimura, Sue F.; Fadem, Mitchell B.; Landay, Alan L.; Levy, Jay A. (1994). "Immunologic Abnormalities Associated with Chronic Fatigue Syndrome". Clin Infect Dis. 18 (Suppl 1): S136–S141. doi:10.1093/clinids/18.Supplement_1.S136.
- ↑ 3.0 3.1 Whiteside, TL; Friberg, D (1998), "Natural killer cells and natural killer cell activity in chronic fatigue syndrome.", Am J Med, 105 (3A): 27S–34S, PMID 9790479
- ↑ 4.0 4.1 Brenu, EW; Huth, TK; Hardcastle, SL; Fuller, K; Kaur, M; Johnston, S; Ramos, S; Staines, D; Marshall-Gradisnik, S (2014). "The Role of adaptive and innate immune cells in chronic fatigue syndrome/myalgic encephalomyelitis". International Immunology. 26 (4): 233–42. doi:10.1093/intimm/dxt068. PMID 24343819.
- ↑ 5.0 5.1 Fletcher, Mary Ann; Maher, Kevin J; Klimas, Nancy (April 2002), "Natural killer cell function in chronic fatigue syndrome", Clinical and Applied Immunology Reviews, 2 (2): 129–139, doi:10.1016/S1529-1049(01)00047-2
- ↑ 6.0 6.1 Brenu, Ekua W; van Driel, Mieke L; Staines, Donald R; Ashton, Kevin J; Hardcastle, Sharni L; Keane, James; Tajouri, Lotti; Peterson, Daniel; Ramos, Sandra B; Marshall-Gradisnik, Sonya M (2012), "Longitudinal investigation of natural killer cells and cytokines in chronic fatigue syndrome/myalgic encephalomyelitis", Journal of Translational Medicine, 10: 88, doi:10.1186/1479-5876-10-88
- ↑ 7.0 7.1 7.2 7.3 7.4 7.5 7.6 7.7 Sompayrac, L (2008). How the Immune System Works. Oxford, Blackwell Publishing.
- ↑ Robson, NC; Hidalgo, L; McAlpine, T; Wei, H; Martínez, VG; Entrena, A; Melen, GJ; MacDonald, AS; Phythian-Adams, A; Sacedón, R; Maraskovsky, E; Cebon, J; Ramírez, M; Vicente, A; Varas, A (2014), "Optimal Effector Functions in Human Natural Killer Cells rely upon Autocrine Bone Morphogenetic Protein Signaling", Cancer Res., 74 (18): 5019–5031, doi:10.1158/0008-5472.CAN-13-2845
- ↑ Ojo-Amaize, Emmanuel A.; Conley, Edward J.; Peter, James B. (1994), "Decreased Natural Killer Cell Activity Is Associated with Severity of Chronic Fatigue Immune Dysfunction Syndrome", Clin Infect Dis, 18 (Supplement 1): S157–S159, doi:10.1093/clinids/18.Supplement_1.S157
- ↑ Huth, TK; Brenu, EW; Ramos, S; Nguyen, T; Broadley, S; Staines, D; Marshall-Gradisnik, S (January 2016), "Pilot Study of Natural Killer Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis", Scand J Immunol, 83 (1): 44–51, doi:10.1111/sji.12388, PMID 26381393
- ↑ 11.0 11.1 Strayer, David; Scott, Victoria; Carter, William (July 29, 2015), "Low NK Cell Activity in Chronic Fatigue Syndrome (CFS) and Relationship to Symptom Severity", Journal of Clinical & Cellular Immunology: 1–9, doi:10.4172/2155-9899.1000348, ISSN 2155-9899, retrieved December 19, 2016
- ↑ 12.0 12.1 Chacko, Anu; Staines, Donald R.; Johnston, Samantha C.; Marshall-Gradisnik, Sonya M. (2016). "Dysregulation of Protein Kinase Gene Expression in NK Cells from Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Patients". Gene Regulation and System Biology (10): 85–93. doi:10.4137/GRSB.S40036. PMID 27594784.
- ↑ 13.0 13.1 Huth, Teilah Kathryn; Staines, Donald; Marshall-Gradisnik, Sonya (April 21, 2016). "ERK1/2, MEK1/2 and p38 downstream signalling molecules impaired in CD56dimCD16+ and CD56brightCD16dim/− natural killer cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients". Journal of Translational Medicine. 14 (1): 97. doi:10.1186/s12967-016-0859-z. ISSN 1479-5876. PMC 4839077. PMID 27098723.
- ↑ Eaton-Fitch, Natalie; Du Preez, Stanley; Cabanas, Hélène; Muraki, Katsuhiko; Staines, Donald; Marshall-Gradisnik, Sonya (February 16, 2022). "Impaired TRPM3-dependent calcium influx and restoration using Naltrexone in natural killer cells of myalgic encephalomyelitis/chronic fatigue syndrome patients". Journal of Translational Medicine. 20 (1): 94. doi:10.1186/s12967-022-03297-8. ISSN 1479-5876. PMC 8848670. PMID 35172836.
- ↑ 15.0 15.1 Petty, Robert D.; McCarthy, Neil E.; Le Dieu, Rifca; Kerr, Jonathan R. (2016). "MicroRNAs hsa-miR-99b, hsa-miR-330, hsa-miR-126 and hsa-miR-30c: Potential Diagnostic Biomarkers in Natural Killer (NK) Cells of Patients with Chronic Fatigue Syndrome (CFS)/ Myalgic Encephalomyelitis (ME)". PLOS One. doi:10.1371/journal.pone.0150904. PMID 26967895.
- ↑ "Master gene that switches on disease-fighting cells identified by scientists - Press release". Imperial College London. September 15, 2009. Retrieved September 14, 2022.
- ↑ Gascoyne, Duncan M; Long, Elaine; Veiga-Fernandes, Henrique; de Boer, Jasper; Williams, Owen; Seddon, Benedict; Coles, Mark; Kioussis, Dimitris; Brady, Hugh JM (September 13, 2009), "The basic leucine zipper transcription factor E4BP4 is essential for natural killer cell development", Nature Immunol, 10: 1118–1124, doi:10.1038/ni.1787, PMID 19749763
- ↑ 18.0 18.1 Gill, HS; Rutherfurd, KJ; Cross, ML (July 2001), "Dietary probiotic supplementation enhances natural killer cell activity in the elderly: an investigation of age-related immunological changes", J Clin Immunol, 21 (4): 264–71, PMID 11506196
- ↑ Chiang, BL; Sheih, YH; Wang, LH; Liao, CK; Gill, HS (2000), "Enhancing immunity by dietary consumption of a probiotic lactic acid bacterium (Bifidobacterium lactis HN019): optimization and definition of cellular immune responses]", European Journal of Clinical Nutrition, 54 (11): 849–855, doi:10.1038/sj.ejcn.1601093
- ↑ Takagi, Akimitsu; Matsuzaki, Takeshi; Sato, Mikiko; Nomoto, Koji; Morotomi, Masami; Yokokura, Teruo (2001), "Enhancement of natural killer cytotoxicity delayed murine carcinogenesis by a probiotic microorganism", Carcinogenesis, 22 (4): 599–605, doi:10.1093/carcin/22.4.599
- ↑ Takeda, K; Suzuki, T; Shimada, SI; Shida, K; Nanno, M; Okumura, K (October 2006), "Interleukin‐12 is involved in the enhancement of human natural killer cell activity by Lactobacillus casei Shirota", Clin Exp Immunol, 146 (1): 109–15, PMID 16968405
- ↑ 22.0 22.1 Morimoto, Kanehisa; Takeshita, Tatsuya; Nanno, Masanobu; Tokudome, Shinkan; Nakayama, Kunio (May 2005), "Modulation of natural killer cell activity by supplementation of fermented milk containing Lactobacillus casei in habitual smokers", Preventive Medicine, 40 (5): 589–594, doi:10.1016/j.ypmed.2004.07.019
- ↑ Ritz, Barry W.; Nogusa, Shoko; Ackerman, Elizabeth A.; Gardner, Elizabeth M. (November 2006), "Supplementation with Active Hexose Correlated Compound Increases the Innate Immune Response of Young Mice to Primary Influenza Infection", J. Nutr., 136 (11): 2868–2873, PMID 17056815
- ↑ Terakawa, Naoyoshi; Matsui, Yoichi; Satoi, Sohei; Yanagimoto, Hiroaki; Takahashi, Kanji; Yamamoto, Tomohisa; Yamao, Jun; Takai, Soichiro; Kwon, A-Hon; Kamiyama, Yasuo (2008), "Immunological Effect of Active Hexose Correlated Compound (AHCC) in Healthy Volunteers: A Double-Blind, Placebo-Controlled Trial", Nutrition and Cancer, 60 (5), doi:10.1080/01635580801993280
- ↑ Glaser, Ronald; Rice, John; Speicher, Carl E.; Stout, Julie C.; Kiecolt-Glaser, Janice K. (October 1986), "Stress depresses interferon production by leukocytes concomitant with a decrease in natural killer cell activity.", Behavioral Neuroscience, 100 (5): 675–678, doi:10.1037/0735-7044.100.5.675
- ↑ Sieber, William J.; Rodin, Judith; Larson, Lynn; Ortega, Susan; Cummings, Nancy; Levy, Sandra; Whiteside, Theresa; Herberman, Ronald (June 1992), "Modulation of human natural killer cell activity by exposure to uncontrollable stress", Brain, Behavior, and Immunity, 6 (2): 141–156, doi:10.1016/0889-1591(92)90014-F
- ↑ Pollock, Raphael E.; Lotzová, Eva; Stanford, Susan D. (1991), "Mechanism of Surgical Stress Impairment of Human Perioperative Natural Killer Cell Cytotoxicity", Arch Surg, 126 (3): 338–342, doi:10.1001/archsurg.1991.01410270082013
- ↑ 28.0 28.1 Pollock, Raphael E.; Babcock, George F.; Romsdahl, Marvin M.; Nishioka, Kenji (September 1, 1984), "Surgical Stress-mediated Suppression of Murine Natural Killer Cell Cytotoxicity", Cancer Research, 44 (9): 3888–3891, ISSN 0008-5472, PMID 6744305, retrieved December 19, 2016
- ↑ Witek-Janusek, Linda; Albuquerque, Kevin; Chroniak, Karen Rambo; Chroniak, Christopher; Durazo, Ramon; Mathews, Herbert L. (August 2008), "Effect of Mindfulness Based Stress Reduction on Immune Function, Quality of Life and Coping In Women Newly Diagnosed with Early Stage Breast Cancer", Brain, behavior, and immunity, 22 (6): 969–981, doi:10.1016/j.bbi.2008.01.012, ISSN 0889-1591, PMID 18359186
- ↑ Tamura, J.; Kubota, K.; Murakami, H.; Sawamura, M.; Matsushima, T.; Tamura, T.; Saitoh, T.; Kurabayshi, H.; Naruse, T. (April 1, 1999), "Immunomodulation by vitamin B12: augmentation of CD8+ T lymphocytes and natural killer (NK) cell activity in vitamin B12-deficient patients by methyl-B12 treatment", Clinical & Experimental Immunology, 116 (1): 28–32, doi:10.1046/j.1365-2249.1999.00870.x, ISSN 1365-2249, retrieved December 19, 2016
- ↑ Marshall-Gradisnik, Sonya M.; Smith, Peter; Brenu, Ekua W.; Nilius, Bernd; Ramos, Sandra B.; Staines, Donald R. (January 1, 2015). "Examination of Single Nucleotide Polymorphisms (SNPs) in Transient Receptor Potential (TRP) Ion Channels in Chronic Fatigue Syndrome Patients". Immunology and Immunogenetics Insights. 7: III.S25147. doi:10.4137/III.S25147. ISSN 1178-6345.
- ↑ Huth, T.K.; Brenu, E.W.; Ramos, S.; Nguyen, T.; Broadley, S.; Staines, D.; Marshall‐Gradisnik, S. (2016). "Pilot Study of Natural Killer Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis". Scandinavian Journal of Immunology. 83 (1): 44–51. doi:10.1111/sji.12388. ISSN 1365-3083.
- ↑ Marshall-Gradisnik, S.M.; Chacko, A.; Johnston, S.; Smith, P.; Nilius, B.; Staines, D.R. (January 1, 2016). "Genotype Frequencies of Transient Receptor Potential Melastatin M3 Ion Channels and Acetylcholine Muscarinic M3 Receptor Gene Polymorphisms in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis Patients". Immunology and Immunogenetics Insights. 8: III.S37042. doi:10.4137/III.S37042. ISSN 1178-6345.
- ↑ Nguyen, T.; Staines, D.; Nilius, B.; Smith, P.; Marshall-Gradisnik, S. (May 31, 2016). "Novel identification and characterisation of Transient receptor potential melastatin 3 ion channels on Natural Killer cells and B lymphocytes: effects on cell signalling in Chronic fatigue syndrome/Myalgic encephalomyelitis patients". Biological Research. 49 (1): 27. doi:10.1186/s40659-016-0087-2. ISSN 0717-6287. PMC 4888729. PMID 27245705.
- ↑ Rivas, Jose Luis; Palencia, Teresa; Fernandez, Guerau; Garcia, Milagros (2018), "Association of T and NK cell phenotype with the diagnosis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)", Frontiers in Immunology, doi:10.3389/fimmu.2018.01028
- ↑ Eaton, Natalie; Cabanas, Hélène; Balinas, Cassandra; Klein, Anne; Staines, Donald R.; Marshall-Gradisnik, Sonya (2018), "Rituximab impedes natural killer cell function in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients: A pilot in vitro investigation", BMC Pharmacology & Toxicology, 19 (12), doi:10.1186/s40360-018-0203-8, PMID 29587879
- ↑ Cabanas, Hélène; Muraki, Katsuhiko; Eaton, Natalie; Balinas, Cassandra; Staines, Donald; Marshall-Gradisnik, Sonya (August 14, 2018). "Loss of Transient Receptor Potential Melastatin 3 ion channel function in natural killer cells from Chronic Fatigue Syndrome/Myalgic Encephalomyelitis patients". Molecular Medicine. 24. doi:10.1186/s10020-018-0046-1. ISSN 1076-1551. PMC 6092868. PMID 30134818.
- ↑ Cabanas, H.; Muraki, K.; Balinas, C.; Eaton-Fitch, N.; Staines, D.; Marshall-Gradisnik, S. (April 23, 2019). "Validation of impaired Transient Receptor Potential Melastatin 3 ion channel activity in natural killer cells from Chronic Fatigue Syndrome/ Myalgic Encephalomyelitis patients". Molecular Medicine. 25. doi:10.1186/s10020-019-0083-4. ISSN 1076-1551. PMC 6480905. PMID 31014226.
- ↑ Walter & Eliza Hall Institute of Medical Research (February 26, 2016), Immune cell 'switch' discovery raises hopes in cancer fight

