Blood
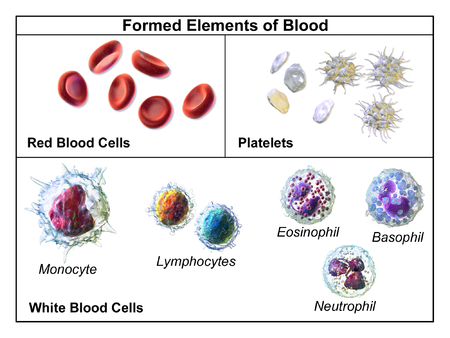
Blood consists of red blood cells, different kinds of white blood cells, plasma and platelets (fragments of blood cells).
Abnormalities in red blood cell shape, red blood cells not being able to change shape properly, and altered blood flow have been detected in patients with ME/CFS. Treatments that address blood flow issues may lead to improvement in symptoms for some patients.
A number of studies have found differences in certain white blood cells. A potential biomarker has been identified by stressing a subset of white blood cells known as PMBCs.
Abnormalities
Low blood volume
A high proportion of ME/CFS patients have been shown via a Dual Tag Test to have significantly lower blood volume than healthy controls.[1][2] A 2018 study using a standard dual isotope erythrocyte labelling technique to determine blood volume, erythrocyte and plasma volume found significantly lower measured blood volume and red blood cell volume per body weight in female ME/CFS with clinical symptoms of orthostatic intolerance (OI) as compared to female ME/CFS patients without a clinical symptoms of orthostatic intolerance (OI).[3]
Less red blood cell deformability
Multiple studies have found unusual properties of red blood cells, including issues with deformability.[4][5][citation needed] Deformability is the ability of a red blood cell to change shape. This is necessary because some capillaries are narrower than the red blood cells themselves. If red blood cells are not deformable enough, blood flow slows down.
More misshapen red blood cells
The shape of red blood cells has been found to be unusual in ME/CFS patients in several studies.[citation needed] This can also slow blood flow, as well as change how molecules dock on the surface of a red blood cell. One study found significantly increased quantities of stomatocytes in the blood of CFS patients. Stomatocytes are red blood cells that have lost their concave shape, usually due to a membrane defect.[6]
Both changes in deformability and changes in shape can be related to the way nutrients are or are not being processed in the body. For example, excess cholesterol can change the shape of red blood cells in some conditions by adhering to the outside of the membrane.[7]
While deformability and unusual red blood cell shape can be indicative of ME/CFS, these abnormalities also occur in other conditions. For example, red blood cell deformability is affected in parasitic infections such as malaria, and metabolic disorders such as diabetes;[8] and unusual red blood cell shape is found in several nutritional deficiencies.[9] While unusual shape and decreased deformability may be said to be signs of illness, they are not characteristic of ME/CFS alone.
Plasma and impaired metabolic in ME/CFS
A biomarker being investigated for ME/CFS found that plasma together with several types of white blood cells, known as collectively as peripheral blood mononuclear cells (PBMCs), reacted differently to plasma and white blood cells from healthy controls when put under a salt stress test designed to mimic post-exertional malaise. The PBMCs from the blood of ME/CFS patients was then put in plasma from healthy controls, which significantly improved their response to the biological stress.[10]
The original hypothesis being tested was that "extensive consumption and potential depletion of ATP, a high-energy metabolite" would be found in the blood of ME/CFS patients, and this was confirmed, along with finding a unique metabolic signature that correctly identified all patients and no healthy controls.[10]
Symptoms Resulting from Abnormalities
Orthostatic intolerance (OI), or difficulty tolerating changes in position, has been estimated to occur in up to 97% of ME/CFS patients.[11] OI is linked to under-oxygenation of the brain[citation needed] due to a combination of red blood cell abnormalities and low blood volume. It has also been suggested that blood pressure and other circulatory system abnormalities contribute to this under-oxygenation.[citation needed]
Proposed Causes for Blood Abnormalities
Abnormality Treatments and Adjustments
Notable studies
- 2016, Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome [12] - (Full text)
- 2018, A new approach to find biomarkers in chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) by single-cell Raman micro-spectroscopy[13] - (Abstract)
- 2018, Erythrocyte Deformability As a Potential Biomarker for Chronic Fatigue Syndrome[4] - (Full text)
- 2018, Blood Volume Status in ME/CFS Correlates With the Presence or Absence of Orthostatic Symptoms: Preliminary Results[14] - (Full text)
- 2018, Blood Volume Status in Patients with Chronic Fatigue Syndrome: Relation to Complaints[3] - (Full text)
- 2019, A nanoelectronics-blood-based diagnostic biomarker for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)[10] - (Full text)
- 2019,Red Blood Cell Deformability is diminished in patients with Chronic Fatigue Syndrome, by Anand Ramasubramanian, PhD and Ronald Davis, PhD, Stanford Collaboration/
Articles and blogs
- 2019, Something in the blood - Simon McGrath
Learn more
See also
- A nanoelectronics-blood-based diagnostic biomarker for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
- Diagnostic biomarker
- Open Medicine Foundation
- Red blood cell
References
- ↑ Hurwitz, BE; Coryell, VT; Parker, M; Martin, P; LaPerriere ...., A; Bilsker, MS. "Chronic fatigue syndrome: illness severity, sedentary lifestyle, blood volume and evidence of diminished cardiac function". Clinical Science. 118 (2): 125–135.
- ↑ Streeten, DHP; Bell, D (1998). "Circulating Blood Volume in Chronic Fatigue Syndrome". Journal of Chronic Fatigue Syndrome. 4: 3–11.
- ↑ 3.0 3.1 Campen, C. (Linda) M. C. van; Visser, Frans C. (2018). "Blood Volume Status in Patients with Chronic Fatigue Syndrome: Relation to Complaints". International Journal of Clinical Medicine. 09 (11): 809–819. doi:10.4236/ijcm.2018.911067. ISSN 2158-284X.
- ↑ 4.0 4.1 Saha, Amit K; Schmidt, Brendan R; Wilhelmy, Julie; Nguyen, Vy; Do, Justin; Suja, Vineeth C; Nemat-Gorgani, Mohsen; Ramasubramanian, Anand K; Davis, Ronald W (November 2018). "Erythrocyte Deformability As a Potential Biomarker for Chronic Fatigue Syndrome". Blood (132): 4874. doi:10.1182/blood-2018-99-117260.
- ↑ Saha, Amit K.; Schmidt, Brendan R.; Wilhelmy, Julie; Nguyen, Vy; Abugherir, Abed; Do, Justin K.; Nemat-Gorgani, Mohsen; Davis, Ronald W.; Ramasubramanian, Anand K. "Red blood cell deformability is diminished in patients with Chronic Fatigue Syndrome". Clinical Hemorheology and Microcirculation. 71 (1): 113–116. doi:10.3233/CH-180469. ISSN 1386-0291. PMC 6398549. PMID 30594919.
- ↑ Richards, RS; Wang, L; Jelinek, H (January 2007). "Erythrocyte oxidative damage in chronic fatigue syndrome". Archives of Medical Research. 38 (1): 94–98.
- ↑ Owen, J.S.; Brown, D.J.; Harry, D.S.; Beaven, G.H.; McIntyre, N ....; Gratzer, W.B. (December 1985). "Erythrocyte echinocytosis in liver disease. Role of abnormal plasma high density lipoproteins". J Clin Invest. 76 (6): 2275–2285.
- ↑ Tomaiuolo, G. (2014). "Biomechanical properties of red blood cells in health and disease towards microfluidics". Biomicrofluidics. 8 (5).
- ↑ "Poikilocytosis -- Abnormal RBC shape". Laboratory Info. 2017.
- ↑ 10.0 10.1 10.2 Davis, R. W.; Wilhelmy, J.; Nemat-Gorgani, M.; Kashi, A.; Esfandyarpour, R. (April 25, 2019). "A nanoelectronics-blood-based diagnostic biomarker for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)". Proceedings of the National Academy of Sciences. 116 (21): 10250–10257. doi:10.1073/pnas.1901274116. ISSN 0027-8424. PMID 31036648.
- ↑ Miwa, K (July 2015). "Cardiac dysfunction and orthostatic intolerance in patients with myalgic encephalomyelitis and a small left ventricle". Heart and Vessels. 30 (4): 484–489.
- ↑ Fluge, Øystein; Mella, Olav; Bruland, Ove; Risa, Kristin; Dyrstad, Sissel E.; Alme, Kine; Rekeland, Ingrid G.; Sapkota, Dipak; Røsland, Gro V. (December 22, 2016). "Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome". JCI insight. 1 (21): e89376. doi:10.1172/jci.insight.89376. ISSN 2379-3708. PMC 5161229. PMID 28018972.
- ↑ Xu, Jiabao; Potter, Michelle; Tomas, Cara; Elson, Jo; Morten, Karl; Poulton, Joanna; Wang, Ning; Jin, Hanqing; Hou, Zhaoxu (2018). "A new approach to find biomarkers in chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) by single-cell Raman micro-spectroscopy". The Analyst. doi:10.1039/C8AN01437J. ISSN 0003-2654.
- ↑ van Campen, C. (Linda) M. C.; Rowe, Peter C.; Visser, Frans C. (November 15, 2018). "Blood Volume Status in ME/CFS Correlates With the Presence or Absence of Orthostatic Symptoms: Preliminary Results". Frontiers in Pediatrics. 6. doi:10.3389/fped.2018.00352. ISSN 2296-2360.

