Coxsackie B virus
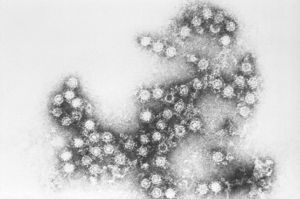
Coxsackie B (also written coxsackievirus B) is a group of six types of enterovirus belonging to the Picornaviridae family. They cause symptoms ranging from gastrointestinal distress to aseptic meningitis, pericarditis and myocarditis. Like other enteroviruses, Coxsackie B viruses have a tropism for muscle cells and have been linked to myalgic encephalomyelitis and chronic fatigue syndrome, fibromyalgia,[1] as well as Type 1 Diabetes.
Symptoms
Symptoms of infection with viruses in the Coxsackie B grouping include fever, headache, sore throat, gastrointestinal distress, extreme fatigue as well as chest and muscle pain. It can also lead to spasms in arms and legs.
Types
Coxsackie B1
Coxsackievirus B1 has been associated with β-cell autoimmunity leading to Type 1 diabetes, as well as neonatal myocarditis.[2][3] CVB1 has also been linked to outbreaks of aseptic meningitis and pleurodynia.[4]
Coxsackie B2
Coxsackievirus B2 has been associated with aseptic meningitis, myocarditis, and neonatal systemic illness.[4]
Coxsackie B3
Coxsackie B3 is found in 20-25% of patients with cardiomyopathy and myocarditis.[5][6][7][5] CVB3 has also been associated with aseptic meningitis, neonatal systemic illness, meningoencephalitis in immunodeficient persons, herpangina, and rash illnesses.[4]
Coxsackie B4
Coxsackievirus B4 has a cell tropism for natural killer cells and pancreatic islet cells.[8] Associated illnesses include aseptic meningitis, encephalitis, myopericarditis, neonatal infections, febrile rash illnesses, and respiratory manifestations.[4] It has been shown that CVB4 has a higher fatality rate than other enterovirus serotypes.[4]
Coxsackie B5
Coxsackievirus B5 is associated with myopericarditis and neonatal systemic illness (encephalomyocarditis syndrome), aseptic meningitis, meningoencephalitis, and acute flaccid paralysis. In a study of CVB5 reports from 1970 to 2005, approximately half of all coxsackievirus B5 detections come from young infants.[4]
Coxcackie B6
Immune system
In a mouse model of myocarditis, Coxsackievirus infection was found to upregulate Toll-like receptor 4 on mast cells and macrophages immediately following infection. It also increased numbers of mast cells.[9]
The induction of interferon signaling and the induction of apoptosis are required for normal control of a Coxsackie B3 infection. Coxsackievirus B3 cleaves Mitochondrial Antiviral Signaling (MAVS) protein and Toll/IL-1 receptor domain-containing adaptor inducing interferon-beta TRIF to inhibit type I interferon induction and evade host immunity.[10] Conversely, upregulation of MAVS inhibits Coxsackie B3 by increasing type-1 interferon production.[11]
Mitochondria
Coxsackievirus B3 cleaves Mitochondrial Antiviral Signaling (MAVS) protein to inhibit type I interferon induction.[10] Conversely, upregulation of MAVS inhibits coxsackie B3 by increasing type-1 interfrenctial.
Exercise
Several studies of a mouse model of Coxsackie B3 myocarditis have found that exercise increases the virulence of the infection and results in poorer outcomes.[12][13][14][15][16] These studies compare two groups of mice, both infected with CVB3, one that is exercised and the other, sedentary. They found:
- Exercised mice died of congestive heart failure (the majority while swimming) and had 530X the amount of virus.[15]
- Exercised mice had increased viral titers, mortality and fiber necrosis.[13]
- Exercised mice had higher viremia and virus in the hearts and no circulating interferon; non-exercised mice had detectable interferon activity, higher levels of neutralizing antibodies[16]
- Exercised mice died at much higher rates (52% v. 0 sedentary mice), but not if they were immunosuppressed.[12]
- Increased T cytotoxic, T suppressor, and T cytotoxic, suppressor/T helper cell ratio, and myocardial inflammatory and necrotic lesions with exercise at 48 hours after infection. "Failure to restrict physical activity in the acute phase of this infection may well contribute to the progression of the disease."[14]
Chronic infection
Coxsackievirus B is able to establish a chronic intracellular non-cytolytic infection which can persist for years. Non-cytolytic enterovirus infection does not involve the destruction of infected cells. Non-cytolytic infection is difficult to measure in the serum as viral particles remain in the cell membranes of tissues.
The molecular mechanisms of non-cytolytic infection were examined in a small study comparing Coxsackie B2 virus cultured in vitro to RNA extracted via muscle biopsy from eight patients with a chronic fatigue syndrome diagnosis. All patients had symptoms of muscle fatiguability. Four of these samples tested positive for enteroviral RNA. In all four patients with enteroviral-specific RNA, the enteroviral RNA had equal amounts of positive sense and negative sense RNA. By contrast, CVB2 virus in culture produced positive sense RNA at a ratio of 100:1. An equal ratio of positive to negative sense RNA would inhibit the translation of virus-specific gene products, explaining the failure to attract a response from the host immune system, and might account for how CVB2 could establish a persistent infection in these four patients.[17]
Models of persistent infection of the heart[18] and brain[19] have also been studied in mice and in thyroid carcinoma.
In human disease
Viruses in the Coxsackie B family progress to myocarditis or pericarditis, which can result in permanent heart damage or death. Coxsackie B virus infection may also cause aseptic meningitis.[20] As a group, they are the most common cause of unexpected sudden death, and may account for up to 50% of such cases.[citation needed]
Myalgic Encephalomyelitis
Some researchers and clinicians postulate that ME is caused by an enteroviral infection. Several studies have found patients with ME to have persistently elevated levels of Coxsackie B IgM or IgG antibodies, circulating immune complexes containing viral antigen, or presence of enterovirus by PCR or culture, all indicating the possible presence of a persistent infection.[21][22] Others studies failed to find a difference in rates of positivity between patients and controls. Differences in study outcomes may be due to the criteria used to define study cohorts as well as the techniques used.
Blood testing
Elevated Coxsackie B antibodies have been found in patients in at least two ME outbreaks.[23][24] In a retrospective cohort study[25] by Melvin Ramsay and Elizabeth Dowsett, 31% of the patients were found to have elevated enteroviral IgM antibody levels. Sixteen of these patients were retested annually over three years and all showed persistently elevated Coxsackie B neutralizing antibody levels and intermittently positive enteroviral IgM, suggesting a persistent infection was present.
Similarly, a study of of 76 patients with postviral fatigue syndrome (PVFS) found that 76% had detectible IgM responses to enteroviruses. 22% had positive cultures (compared to 7% controls) and VP1 antigen was detected in 51%, all pointing to a chronic infection in many post-viral patients.[26] However, a larger study in Scotland of 243 PVFS patients and matched controls found no difference in IgM and IgG positivity between patients and controls.[27]
PCR
In a study of serum samples from 100 CFS patients and 100 healthy controls, 42% of patients were positive for Coxsackie B sequences by PCR, compared to only 9% of the comparison group.[28]
Also using PCR, a study of 236 patients by John Chia found enteroviral RNA in 48% of patients as compared to 8% of controls.To date, Chia reports finding enteroviral RNA in 35% of 518 patients.[22]
Muscle biopsy
Several muscle biopsy studies have also found the presence of Coxsackie B RNA sequences in CFS patients as compared to controls. A study of 60 post-viral fatigue syndrome patients found 53% had enteroviral RNA in muscle compared to 15% of controls.[29] However, a follow-up study comparing CFS patients to patients with other neuromuscular disorders failed to find a statistically significant difference.[30]
Fibromyalgia
Type 1 diabetes
Several studies have suggested a relationship between Coxsackie B4 and the onset of Type 1 diabetes.[31][32][33]
A study of patients with Type 1 Diabetes found that Coxsackie B4 was found to infect the β cells in the pancreatic islets of the pancreas and cause inflammation mediated by natural killer cells.[34]
Testing
In the United States, ARUP Laboratories offers a serum microneutralization assay that is designed to measure the concentration of serum antibodies to six serotypes of the virus; B1 through B6. This specific assay has been shown to be sensitive for detection of chronic infections in ME patients. A persistent fourfold or greater rise in antibody titer is often found in these patients, which is not often found in healthy controls.
A complement fixation assay for Coxsackie B serotypes is available in the United States from LabCorp and Quest Diagnostics, however this specific type of assay has not been found to be sensitive for the chronic infections found in ME patients.
Antivirals and immunomodulators for coxsackievirus B
Interferon
Treatment of enterovirus-associated ME/CFS with a course of Interferon (or interferon plus the antiviral Ribavirin) over a few months results in dramatic improvements, allowing many severe bedbound ME/CFS patients being able to return to work. However, these improvements achieved with interferon typically only last for a short period of a few months to a year, after which relapse usually occurs.[35] Repeated treatment with interferon is usually not feasible, as patients typically eventually develop antibodies against recombinant interferon, which disables this drug. Thus interferon clearly demonstrates that inhibiting the enteroviruses associated with ME/CFS results in large improvements in symptoms; but interferon type 1 and 2 is not effective as a cure or long-term treatment of ME/CFS.
Dr John Chia finds interferon type 1 and 2 works for ME/CFS associated with coxsackievirus B3 and B5, but is not effective against coxsackievirus B4.[36]
Oxymatrine
The mainstay of Dr Chia's treatment of enterovirus-associated ME/CFS is the immunomodulator oxymatrine, which Chia found in an informal study leads to 30% of ME/CFS patients making a major improvement, and another 20% will make more minor improvements. Dr Chia often adds the immunomodulator inosine to oxymatrine. He also uses the antiviral Epivir (lamivudine) to treat enterovirus ME/CFS.[37]
Ampligen
The immunomodulatory drug Ampligen (rintatolimod) is a treatment that has proven effective for ME/CFS in clinical trials, and in mouse models, Ampligen was found to be protective of coxsackievirus B3 myocarditis.[38]
Pleconaril
One ME/CFS patient with coxsackievirus B4 experienced moderate improvement on the antiviral drug Pleconaril for one month, along with a fourfold decrease of antibody titers for CVB4 and echoviruses 7 and 11. However on discontinuation of the drug the patient relapsed about one month later, and did not respond to a further month of treatment. Pleconaril is no longer available for investigational use.[22]
Rega Compound
Two potent new antiviral drugs for coxsackievirus B code named Rega Compound A and Rega Compound 17 are expected to become available in around 2021. These two drugs were originally developed by the Rega Institute in Belgium (info here). Dr Chia believes these drugs may be effective treatments for enterovirus-associated ME/CFS.
Supplements
Selenium deficiency increases the virulence of coxsackievirus B3 infections in a mouse model.[39] Drugs and supplements which may have some mild in vivo antiviral effects (at least in murine studies) against coxsackievirus B include:
Sophoridine (Sophora root extract),[40] Arbidol (umifenovir),[41][42] astragaloside IV (from Astragalus membranous),[43] cinnamic acid (a metabolite of cinnamon spice),[44] emodin (from Rheum palmatum),[45] dihydroquercetin (DHQ),[46] arsenic trioxide,[47] Spatholobus suberectus (Ji Xue Teng),[48] salidroside (from Rhodiola rosea),[49] and quercetin.[50]
N-acetyl cysteine (NAC) has been proven to effectively treat Coxsackivirus B3 in vivo.[51]
Factors which worsen coxsackievirus B infection
Exercise has been shown to be a risk factor that often worsens coxsackievirus B infection.[13][14][15][16]
See also
- Enterovirus
- Non-cytolytic enterovirus
- Coxsackie A
- Echovirus
- Viral testing in ME/CFS
- Epidemic myalgic encephalomyelitis
- Enteroviral infection hypothesis
- List of enterovirus infection studies
- Post-mortem brain studies
References
- ↑ Nash, P.; Chard, M.; Hazleman, B. (November 1989). "Chronic coxsackie B infection mimicking primary fibromyalgia". The Journal of Rheumatology. 16 (11): 1506–1508. ISSN 0315-162X. PMID 2557447.
- ↑ Laitinen, Olli H.; Honkanen, Hanna; Pakkanen, Outi; Oikarinen, Sami; Hankaniemi, Minna M.; Huhtala, Heini; Ruokoranta, Tanja; Lecouturier, Valérie; André, Philippe (February 1, 2014). "Coxsackievirus B1 Is Associated With Induction of β-Cell Autoimmunity That Portends Type 1 Diabetes". Diabetes. 63 (2): 446–455. doi:10.2337/db13-0619. ISSN 0012-1797. PMID 23974921.
- ↑ Verma, Natasha A.; Zheng, Xiaotian T.; Harris, Michelle U.; Cadichon, Sandra B.; Melin-Aldana, Hector; Khetsuriani, Nino; Oberste, M. Steven; Shulman, Stanford T. (September 1, 2009). "Outbreak of Life-Threatening Coxsackievirus B1 Myocarditis in Neonates". Clinical Infectious Diseases. 49 (5): 759–763. doi:10.1086/605089. ISSN 1058-4838.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 "Enterovirus Surveillance --- United States, 1970--2005". Centers for Disease Control and Prevention. Retrieved October 19, 2020.
- ↑ 5.0 5.1 Jin O, Sole MJ, Butany JW, Chia WK, McLaughlin PR, et al. (1990) Detection of enterovirus RNA in myocardial biopsies from patients with myocarditis and cardiomyopathy using gene amplification by polymerase chain reaction. Circulation 82: 8–16.
- ↑ Bowles NE, Richardson PJ, Olsen EG, Archard LC (1986) Detection of Coxsackie-B-virus-specific RNA sequences in myocardial biopsy samples from patients with myocarditis and dilated cardiomyopathy. Lancet 1: 1120–1123.
- ↑ Martin AB, Webber S, Fricker FJ, Jaffe R, Demmler G, et al. (1994) Acute myocarditis. Rapid diagnosis by PCR in children. Circulation 90: 330–339.
- ↑ Dotta, Francesco; Censini, Stefano; Halteren, Astrid G. S. van; Marselli, Lorella; Masini, Matilde; Dionisi, Sabrina; Mosca, Franco; Boggi, Ugo; Muda, Andrea Onetti (March 20, 2007). "Coxsackie B4 virus infection of β cells and natural killer cell insulitis in recent-onset type 1 diabetic patients". Proceedings of the National Academy of Sciences. 104 (12): 5115–5120. doi:10.1073/pnas.0700442104. ISSN 0027-8424. PMID 17360338.
- ↑ http://www.ncbi.nlm.nih.gov/pubmed/15386590
- ↑ 10.0 10.1 Mukherjee, A (March 2011). "The coxsackievirus B 3C protease cleaves MAVS and TRIF to attenuate host type I interferon and apoptotic signaling". PLoS Pathology. 7.
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3546859/
- ↑ 12.0 12.1 Cabinian AE, Kiel RJ, Smith F, Ho KL, Khatib R, Reyes MR. Modification of exercise-aggravated coxsackie virus B3 murine myocarditis by T-lymphocyte suppression in an inbred model. J. Lab. Clin. Med. 1990; 115: 454– 62.
- ↑ 13.0 13.1 13.2 Kiel RJ, Smith FE, Chason J, Khatib R, Reyes MD. Coxsackie B3 myocarditis in C3H/HeJ mice: Description of an inbred model and the effect of exercise on the virulence. Eur. J. Epidemiol. 1989; 5: 248– 67.
- ↑ 14.0 14.1 14.2 Ilbäck, NG (June 1989). "Exercise in coxsackie B3 myocarditis: Effects on heart lymphocyte subpopulations and the inflammatory reaction". American Heart Journal. 117: 1298–302.
- ↑ 15.0 15.1 15.2 Gatmaitan, Bienvenido (June 1, 1970). "Augmentation of the Virulence of Murine Coxsackie Virus B-3 Myocardiopathy by Exercise". Journal of Experimental Medicine. 131: 1121.
- ↑ 16.0 16.1 16.2 Reyes, MP (February 1976). "Interferon and neutralizing antibody in sera of exercised mice with coxsackievirus B-3 myocarditis". Proceedings of the Society for Experimental Biology and Medicine. 151: 333–8.
- ↑ Cunningham, Louise (1990). "Persistence of enteroviral RNA in chronic fatigue syndrome is associated with the abnormal production of equal amounts of positive and negative strands of enteroviral RNA". Journal of General Virology. 71: 1399–1402.
- ↑ Chapman N.M., Kim K.S. (2008) Persistent Coxsackievirus Infection: Enterovirus Persistence in Chronic Myocarditis and Dilated Cardiomyopathy. In: Tracy S., Oberste M.S., Drescher K.M. (eds) Group B Coxsackieviruses. Current Topics in Microbiology and Immunology, vol 323. Springer, Berlin, Heidelberg
- ↑ Feuer, Ralph (September 2009). "Viral Persistence and Chronic Immunopathology in the Adult Central Nervous System following Coxsackievirus Infection during the Neonatal Period". Journal of Virology. 83: 9356–9369.
- ↑ Tariq N, Kyriakopoulos C. Group B Coxsackie Virus. Jul 16, 2021. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 Jan-.
- ↑ Landay, AL (September 1991). "Chronic fatigue syndrome: clinical condition associated with immune activation". Lancet.
- ↑ 22.0 22.1 22.2 Chia, John (November 2005). "The role of enterovirus in chronic fatigue syndrome". Journal of Clinical Pathology.
- ↑ Fegan, KG; Behan, PO; Bell, EJ (June 1, 1983), "Myalgic encephalomyelitis — report of an epidemic", J R Coll Gen Pract, 33 (251): 335–337, PMID 6310104
- ↑ Calder, BD; Warnock, PJ (January 1984), "Coxsackie B infection in a Scottish general practice", Jrnl Royal Coll Gen Pract, 34 (258): 15–19, PMID 6319691
- ↑ Dowsett, EG; Ramsay, AM; McCartney, RA; Bell, EJ (July 1, 1990), "Myalgic encephalomyelitis--a persistent enteroviral infection?", Postgraduate Medical Journal, 66 (777): 526–530, doi:10.1136/pgmj.66.777.526, PMID 2170962
- ↑ Yousef, G.E. (January 1988). "CHRONIC ENTEROVIRUS INFECTION IN PATIENTS WITH POSTVIRAL FATIGUE SYNDROME". The Lancet.
- ↑ Miller, N A (1991). "Antibody to Coxsackie B virus in diagnosing postviral fatigue syndrome". The British Medical Journal.
- ↑ Nairn, C (August 1995). "Comparison of coxsackie B neutralisation and enteroviral PCR in chronic fatigue patients". Journal of Medical Virology.
- ↑ Gow, JW. "Enteroviral RNA sequences detected by polymerase chain reaction in muscle of patients with postviral fatigue syndrome". British Medical Journal.
- ↑ Gow, JW (1994). "Studies on enterovirus in patients with chronic fatigue syndrome". Clin Infect Dis. 18 (Supp 1).
- ↑ http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1587352/
- ↑ http://link.springer.com/article/10.1007%2Fs00125-003-1297-z
- ↑ http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0057729
- ↑ http://www.pnas.org/content/104/12/5115.full
- ↑ Chia, J.K.S. (November 1, 2005). "The role of enterovirus in chronic fatigue syndrome". Journal of Clinical Pathology. 58 (11): 1126–1132. doi:10.1136/jcp.2004.020255. ISSN 0021-9746. PMID 16254097.
The results of antiviral treatment provided supportive evidence for the pathogenic role of RNA in patients with CFS.
- ↑ Chia, John (2009). "Diagnosis and Treatment of Myalgic Encephalomyelitis / Chronic Fatigue Syndrome Associated with Chronic Enterovirus Infection. Presentation at the Invest in ME International ME Conference, London 2009 (available on DVD). Timecode: 42:31".
Interestingly enough, my son also has coxsackie B4, and for coxsackie B4, the antibody titer did not change at all, which is what I usually see using ribavirin and interferon; it is ineffective against coxsackie B4.
- ↑ McLaughlin, Christine (February 18, 2014). ""Could This Really Be Happening"? One Year With Dr. Chia – A Chronic Fatigue Syndrome Patient Reports".
- ↑ Padalko, E (January 2004). "The interferon inducer ampligen [poly(I)-poly(C12U)] markedly protects mice against coxsackie B3 virus-induced myocarditis". Antimicrobial Agents and Chemotherapy. 48: 267–74.
- ↑ http://jn.nutrition.org/content/130/2/485S.full
- ↑ Zhang, Yuanyuan; Zhu, Haiyan; Ye, Guan; Huang, Chenggang; Yang, Yingzhen; Chen, Ruizhen; Yu, Yong; Cui, Xiaolan (March 20, 2006). "Antiviral effects of sophoridine against coxsackievirus B3 and its pharmacokinetics in rats". Life Sciences. 78 (17): 1998–2005. doi:10.1016/j.lfs.2005.09.034. ISSN 0024-3205. PMID 16309710.
- ↑ Shi, L.; Xiong, H.; He, J.; Deng, H.; Li, Q.; Zhong, Q.; Hou, W.; Cheng, L.; Xiao, H. (2007). "Antiviral activity of arbidol against influenza A virus, respiratory syncytial virus, rhinovirus, coxsackie virus and adenovirus in vitro and in vivo". Archives of Virology. 152 (8): 1447–1455. doi:10.1007/s00705-007-0974-5. ISSN 0304-8608. PMID 17497238.
- ↑ Zhong, Qiong; Yang, Zhanqiu; Liu, Yuanyuan; Deng, Haiying; Xiao, Hong; Shi, Liqiao; He, Jing (2009). "Antiviral activity of Arbidol against Coxsackie virus B5 in vitro and in vivo". Archives of Virology. 154 (4): 601–607. doi:10.1007/s00705-009-0346-4. ISSN 1432-8798. PMID 19291363.
- ↑ Zhang, Yuanyuan; Zhu, Haiyan; Huang, Chenggang; Cui, Xiaolan; Gao, Yingjie; Huang, Yang; Gong, Wenfeng; Zhao, Ye; Guo, Shanshan (February 2006). "Astragaloside IV exerts antiviral effects against coxsackievirus B3 by upregulating interferon-gamma". Journal of Cardiovascular Pharmacology. 47 (2): 190–195. doi:10.1097/01.fjc.0000199683.43448.64. ISSN 0160-2446. PMID 16495755.
- ↑ Ding, YuanYuan; Qiu, Lin; Zhao, GangTao; Xu, Jingfeng; Wang, Siwang (August 2010). "Influence of cinnamaldehyde on viral myocarditis in mice". The American Journal of the Medical Sciences. 340 (2): 114–120. doi:10.1097/MAJ.0b013e3181dd3b43. ISSN 1538-2990. PMID 20460981.
- ↑ Liu, Zhao; Wei, Fei; Chen, Liang-Jun; Xiong, Hai-Rong; Liu, Yuan-Yuan; Luo, Fan; Hou, Wei; Xiao, Hong; Yang, Zhan-Qiu (September 25, 2013). "In vitro and in vivo studies of the inhibitory effects of emodin isolated from Polygonum cuspidatum on Coxsakievirus B₄". Molecules (Basel, Switzerland). 18 (10): 11842–11858. doi:10.3390/molecules181011842. ISSN 1420-3049. PMID 24071990.
- ↑ Galochkina, Anastasia V.; Anikin, Vadim B.; Babkin, Vasily A.; Ostrouhova, Liudmila A.; Zarubaev, Vladimir V. (April 2016). "Virus-inhibiting activity of dihydroquercetin, a flavonoid from Larix sibirica, against coxsackievirus B4 in a model of viral pancreatitis". Archives of Virology. 161 (4): 929–938. doi:10.1007/s00705-016-2749-3. ISSN 1432-8798. PMID 26780775.
- ↑ Molin, Ylva; Frisk, Peter; Hjelm, Eva; Blomberg, Jonas; Friman, Göran; Ilbäck, Nils-Gunnar (November 2010). "Arsenic trioxide influences viral replication in target organs of coxsackievirus B3-infected mice". Microbes and Infection. 12 (12–13): 1027–1034. doi:10.1016/j.micinf.2010.07.003. ISSN 1769-714X. PMID 20638482.
- ↑ Pang, Ji; Guo, Jin-peng; Jin, Min; Chen, Zhi-qiang; Wang, Xin-wei; Li, Jun-Wen (October 2011). "Antiviral effects of aqueous extract from Spatholobus suberectus Dunn. against coxsackievirus B3 in mice". Chinese Journal of Integrative Medicine. 17 (10): 764–769. doi:10.1007/s11655-011-0642-1. ISSN 1672-0415. PMID 21717161.
- ↑ Wang, Haibo; Ding, Yuanyuan; Zhou, Jun; Sun, Xiaoli; Wang, Siwang (March 2009). "The in vitro and in vivo antiviral effects of salidroside from Rhodiola rosea L. against coxsackievirus B3". Phytomedicine: International Journal of Phytotherapy and Phytopharmacology. 16 (2–3): 146–155. doi:10.1016/j.phymed.2008.07.013. ISSN 1618-095X. PMID 18818064.
- ↑ Colunga Biancatelli, Ruben Manuel Luciano; Berrill, Max; Catravas, John D.; Marik, Paul E. (2020). "Quercetin and Vitamin C: An Experimental, Synergistic Therapy for the Prevention and Treatment of SARS-CoV-2 Related Disease (COVID-19)". Frontiers in Immunology. 11. doi:10.3389/fimmu.2020.01451. ISSN 1664-3224.
- ↑ Wang, Yao; Zhao, Shuoxuan; Chen, Yang; Wang, Ying; Wang, Tianying; Wo, Xiaoman; Dong, Yanyan; Zhang, Jian; Xu, Weizhen (July 1, 2020). "N-Acetyl cysteine effectively alleviates Coxsackievirus B-Induced myocarditis through suppressing viral replication and inflammatory response". Antiviral Research. 179: 104699. doi:10.1016/j.antiviral.2019.104699. ISSN 0166-3542.

