Vagus nerve stimulation
Vagus nerve stimulation or vagal nerve stimulation or VNS is a medical treatment that involves delivering electrical impulses to the vagus nerve via a device that is either implanted or wearable. This VNS device sometimes referred to informally as a "pacemaker for the brain."[1]
The effects of VNS were first observed in the 1880s that massage and compression of the carotid artery in the neck could suppress seizures, an effect attributable to crude, early form of VNS.[2] Currently, VNS is most frequently used as an adjunctive treatment for certain types of intractable epilepsy[3] and treatment-resistant depression.[3][4]
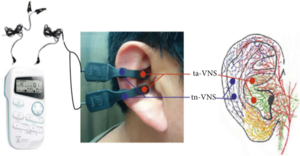
Transcutaneous Vagus Nerve Stimulation[edit | edit source]
Transcutaneous Vagus Nerve Stimulation (t-VNS or ta-VNS), sometimes called auricular Vagus Nerve Stimulation or (aVNS) is a noninvasive method of VNS involving using a device with electrodes attached to the ear to transmit the signal through the skin to stimulate the vagus nerve. Transcutaneous vagus nerve stimulation can be done by patients at home, and the device does not need to be worn continually.[1]
Intranasal Mechanical Stimulation[edit | edit source]
Intranasal mechanical stimulation of the vagus nerve (e.g., using INMEST) is a non-invasive wearable form of vagus nerve stimulation which has been the subject of a small clinical trial in ME/CFS patients who met the Canadian Consensus Criteria. INMEST resulted in an significant improvement in symptoms in moderate and severe ME but no improvement in fatigue.[5]
Surgical VNS[edit | edit source]
VNS can also be delivered via an implantable device, requiring surgery.[1]
It is possible that paced breathing (e.g., via deep breathing exercise, yoga or aerobic exercise) can also influence brain electrical activity, mediated by VNS arising from the diaphragm.
Manual vagus nerve stimulation[edit | edit source]
Some ME/CFS patients have found that regular manual vagus nerve stimulation improves ME/CFS symptoms both in the short and long term, although these reports have not been confirmed by clinicians. In addition to deep breathing[6], these techniques include gargling[7], "The Basic Exercise" (as described by Stanley Rosenberg[8]), and stimulating the diving reflex by immersing the face in cool water.[9] These techniques can be done by the patient at home and are free.
Uses[edit | edit source]
Implantable vagus nerve stimulation has been approved for epilepsy and depression in the US, and a non-invasive vagus nerve stimulation device has been approved for cluster headaches in the US.[4]
In parts of Europe noninvasive vagus nerve stimulation devices have been approved for pain, depression and epilepsy.[4]
While still experimental, researchers are trialing with vagus nerve stimulation as an adjunct therapy on a host of mental health, neurological, and inflammatory illnesses, including anxiety,[10] atrial fibrillation,[11] chronic pain,[12] Crohn's disease,[13] fibromyalgia,[14] heart failure,[15] insomnia sleep problems,[16] migraines,[17] long COVID,[18] and many other conditions.
Kevin J. Tracey, MD and his research group at The Feinstein Institute for Medical Research have shown that vagus nerve stimulation has decreased inflammation in methotrexate-resistant rheumatoid arthritis patients.[19]
Mechanisms[edit | edit source]
The vagus nerve can inhibit cytokine release, via release of the neurotransmitter acetylcholine[20] and thereby prevent tissue injury and death. In research studies, stimulation of the vagus nerve prevents the damaging effects of cytokine release in experimental sepsis, endotoxemia,[21] ischemia/reperfusion injury, hemorrhagic shock, arthritis, and other inflammatory syndromes.[22]
ME/CFS[edit | edit source]
News and articles[edit | edit source]
- 2016, Electronic implant in 'Spock' nerve could reverse rheumatoid arthritis - The Telegraph[23]
- 2016, Vagus Nerve Stimulation, Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS) - Health Rising[24]
- 2014, Can the Nervous System Be Hacked? - The New York Times[25]
Notable studies[edit | edit source]
- 2022, Non-Invasive Transcutaneous Vagus Nerve Stimulation for the Treatment of Fibromyalgia Symptoms: A Study Protocol[26] - (Full text)
- 2022, Neuromodulation for Chronic Daily Headache[27] - (Full text)
- 2021, Vagal nerve stimulation as a possible non-invasive treatment for chronic widespread pain in Gulf Veterans with Gulf War Illness[28] - (Full text)
- 2021, Transcutaneous Auricular Vagus Nerve Stimulation (tVNS) can Reverse the Manifestations of the Long-COVID Syndrome: A Pilot[18] - (Full text, archived)
- AB0051 The Effects Of Non-Invasive Vagus Nerve Stimulation On Immunological Responses And Patient Reported Outcome Measures Of Fatigue In Patients With Chronic Fatigue Syndrome, Fibromyalgia, And Rheumatoid Arthritis[29] - (Abstract)
- gammaCore (made by ElectroCore) is a device for non-invasive vagus nerve stimulation at the left or right side of the neck. Conflicts of interest: Bruce Simon is an employee and shareholder of electroCore, Justyna Blake is an employee of electroCore, and receives stock ownership.
- 2020, Achieving symptom relief in patients with Myalgic encephalomyelitis by targeting the neuro-immune interface and inducing disease tolerance[5] - (Full text)]
- 2020, Effect of Transcutaneous Vagus Nerve Stimulation at Auricular Concha for Insomnia: A Randomized Clinical Trial[16] - (Full text)
- 2020, The Impact of Auricular Vagus Nerve Stimulation on Pain and Life Quality in Patients with Fibromyalgia Syndrome[30] - (Full text)
- 2019, Current Directions in the Auricular Vagus Nerve Stimulation I -A Physiological Perspective[31] - (Full text)
- 2019, Current directions in the auricular vagus nerve stimulation II–an engineering perspective[32] - (Full text)
- 2018, Transcutaneous auricular vagus nerve stimulation reduces pain and fatigue in patients with systemic lupus erythematosus: a randomised, double-blind, sham-controlled pilot trial[33] - (Abstract)
- Both pain and fatigue were significantly reduced.
- 2015, Noninvasive vagus nerve stimulation for acute treatment of high-frequency and chronic migraine: an open-label study[34] - (Full text)
See also[edit | edit source]
Learn more[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 "Vagus Nerve Stimulation (VNS)". Epilepsy Foundation. Retrieved February 25, 2020.
- ↑ Lanska, DJ (February 2002). "J.L. Corning and vagal nerve stimulation for seizures in the 1880s". Neurology. 58 (3): 452–9.
- ↑ 3.0 3.1 Pisapia, Jared; Baltuch, Gordon (January 22, 2016). "Vagus nerve stimulation: Introduction and technical aspects". In Hamani, Clement; Holtzheimer, Paul; Lozano, Andres; Mayberg, Helen (eds.). Neuromodulation in Psychiatry. Chicester, UK: Wiley-Blackwell. doi:10.1002/9781118801086.ch17/. ISBN 978-1118801048.
- ↑ 4.0 4.1 4.2 "Vagus nerve stimulation". Mayo Clinic. Retrieved February 25, 2020.
- ↑ 5.0 5.1 Rodriguez, Lucie S. T.; Pou, Christian; Lakshmikanth, Tadepally; Zhang, Jingdian; Mugabo, Constantin Habimana; Wang, Jun; Mikes, Jaromir; Olin, Axel; Chen, Yang (February 28, 2020). "Achieving symptom relief in patients with Myalgic encephalomyelitis by targeting the neuro-immune interface and inducing disease tolerance". bioRxiv: 2020.02.20.958249. doi:10.1101/2020.02.20.958249.
- ↑ "Breathing Exercises: Three To Try | 4-7-8 Breath | Andrew Weil, M.D." DrWeil.com. October 28, 2016. Retrieved April 7, 2021.
- ↑ Kharrazian, Datis (2013). Why isn't my brain working? : a revolutionary understanding of brain decline and effective strategies to recover your brain's health. Carlsbad, CA. ISBN 978-0-9856904-3-4. OCLC 853272721.
- ↑ Rosenberg, Stanley (2017). Accessing the healing power of the vagus nerve : self-help exercises for anxiety, depression, trauma, and autism. Berkeley, California. ISBN 978-1-62317-024-0. OCLC 918969766.
- ↑ Godek, Devon; Freeman, Andrew M. (2020). Physiology, Diving Reflex. Treasure Island (FL): StatPearls Publishing. PMID 30855833.
- ↑ Fanselow, Michael S. (June 1, 2013). "Fear and anxiety take a double hit from vagal nerve stimulation". Biological Psychiatry. 73 (11): 1043–1044. doi:10.1016/j.biopsych.2013.03.025. ISSN 1873-2402. PMID 23647735.
- ↑ Stavrakis, Stavros; Humphrey, Mary Beth; Scherlag, Benjamin J.; Hu, Yanqing; Jackman, Warren M.; Nakagawa, Hiroshi; Lockwood, Deborah; Lazzara, Ralph; Po, Sunny S. (March 10, 2015). "Low-level transcutaneous electrical vagus nerve stimulation suppresses atrial fibrillation". Journal of the American College of Cardiology. 65 (9): 867–875. doi:10.1016/j.jacc.2014.12.026. ISSN 1558-3597. PMID 25744003.
- ↑ Chakravarthy, Krishnan; Chaudhry, Hira; Williams, Kayode; Christo, Paul J. (December 2015). "Review of the Uses of Vagal Nerve Stimulation in Chronic Pain Management". Current Pain and Headache Reports. 19 (12): 54. doi:10.1007/s11916-015-0528-6. ISSN 1534-3081. PMID 26493698.
- ↑ Bonaz, B.; Sinniger, V.; Hoffmann, D.; Clarençon, D.; Mathieu, N.; Dantzer, C.; Vercueil, L.; Picq, C.; Trocmé, C.; Faure, P.; Cracowski, J.-L.; Pellissier, S. (June 2016). "Chronic vagus nerve stimulation in Crohn's disease: a 6-month follow-up pilot study". Neurogastroenterology and Motility: The Official Journal of the European Gastrointestinal Motility Society. 28 (6): 948–953. doi:10.1111/nmo.12792. ISSN 1365-2982. PMID 26920654.
- ↑ Lange, Gudrun; Janal, Malvin N.; Maniker, Allen; Fitzgibbons, Jennifer; Fobler, Malusha; Cook, Dane; Natelson, Benjamin H. (September 2011). "Safety and efficacy of vagus nerve stimulation in fibromyalgia: a phase I/II proof of concept trial". Pain Medicine (Malden, Mass.). 12 (9): 1406–1413. doi:10.1111/j.1526-4637.2011.01203.x. ISSN 1526-4637. PMID 21812908.
- ↑ Hauptman, Paul J.; Schwartz, Peter J.; Gold, Michael R.; Borggrefe, Martin; Van Veldhuisen, Dirk J.; Starling, Randall C.; Mann, Douglas L. (June 2012). "Rationale and study design of the increase of vagal tone in heart failure study: INOVATE-HF". American Heart Journal. 163 (6): 954–962.e1. doi:10.1016/j.ahj.2012.03.021. ISSN 1097-6744. PMID 22709747.
- ↑ 16.0 16.1 Jiao, Yue; Guo, Xiao; Luo, Man; Li, Suxia; Liu, Aihua; Zhao, Yufeng; Zhao, Bin; Wang, Dequan; Li, Zaifang (August 7, 2020). "Effect of Transcutaneous Vagus Nerve Stimulation at Auricular Concha for Insomnia: A Randomized Clinical Trial". Evidence-Based Complementary and Alternative Medicine. 2020: 6049891. doi:10.1155/2020/6049891. PMC 7429019. PMID 32831871.
- ↑ Silberstein, Stephen D.; Calhoun, Anne H.; Lipton, Richard B.; Grosberg, Brian M.; Cady, Roger K.; Dorlas, Stefanie; Simmons, Kristy A.; Mullin, Chris; Liebler, Eric J.; Goadsby, Peter J.; Saper, Joel R.; EVENT Study Group (August 2, 2016). "Chronic migraine headache prevention with noninvasive vagus nerve stimulation: The EVENT study". Neurology. 87 (5): 529–538. doi:10.1212/WNL.0000000000002918. ISSN 1526-632X. PMID 27412146.
- ↑ 18.0 18.1 Verbanck, P; Clarinval AM, AM; Burton, F; Corazza, F; Nagant, C; Cheron, G (2021). "Transcutaneous Auricular Vagus Nerve Stimulation (tVNS) can Reverse the Manifestations of the Long-COVID Syndrome: A Pilot Study". Advances in Neurology and Neuroscience Research. p. 100011. doi:10.51956/ANNR.100011 (inactive April 7, 2022) Check
|doi=value (help). Archived from the original on February 13, 2022. Retrieved January 19, 2022.CS1 maint: DOI inactive as of April 2022 (link) - ↑ "Kevin J. Tracey, MD". feinstein.northwell.edu. Retrieved February 25, 2020.
- ↑ Lund, D. D.; Oda, R.P.; Pardini, B.J.; Schmid, P.G. (March 1986). "Vagus nerve stimulation alters regional acetylcholine turnover in rat heart". Circulation Research. 58 (3): 372–377. ISSN 0009-7330. PMID 3719926.
- ↑ Borovikova, Lyudmila V.; Ivanova, Svetlana; Zhang, Minghuang; Yang, Huan; Botchkina, Galina I.; Watkins, Linda R.; Wang, Haichao; Abumrad, Naji; Eaton, John W.; Tracey, Kevin J. (May 25, 2000). "Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin". Nature. 405 (6785): 458–462. doi:10.1038/35013070. ISSN 0028-0836. Retrieved December 12, 2016.
- ↑ Tracey, Kevin J. (February 1, 2007). "Physiology and immunology of the cholinergic antiinflammatory pathway". Journal of Clinical Investigation. 117 (2): 289–296. doi:10.1172/JCI30555. ISSN 0021-9738. PMID 17273548. Retrieved December 12, 2016.
- ↑ Knapton, Sarah (July 7, 2016). "Electronic implant in 'Spock' nerve could reverse rheumatoid arthritis". The Telegraph. London. Retrieved December 12, 2016.
- ↑ Johnson, Cort (January 11, 2016). "Vagus Nerve Stimulation, Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS)". HealthRising. Henderson, NV. Retrieved December 12, 2016.
- ↑ Behar, Michael (May 23, 2014). "Can the Nervous System Be Hacked?". The New York Times. Retrieved December 12, 2016.
- ↑ Molero-Chamizo, Andrés; Nitsche, Michael A.; Bolz, Armin; Andújar Barroso, Rafael Tomás; Alameda Bailén, José R.; García Palomeque, Jesús Carlos; Rivera-Urbina, Guadalupe Nathzidy (January 2022). "Non-Invasive Transcutaneous Vagus Nerve Stimulation for the Treatment of Fibromyalgia Symptoms: A Study Protocol". Brain Sciences. 12 (1): 95. doi:10.3390/brainsci12010095. ISSN 2076-3425.
- ↑ Coppola, Gianluca; Magis, Delphine; Casillo, Francesco; Sebastianelli, Gabriele; Abagnale, Chiara; Cioffi, Ettore; Di Lenola, Davide; Di Lorenzo, Cherubino; Serrao, Mariano (February 7, 2022). "Neuromodulation for Chronic Daily Headache". Current Pain and Headache Reports. 26 (3): 267–278. doi:10.1007/s11916-022-01025-x. ISSN 1531-3433. PMC 8927000. PMID 35129825.
- ↑ Natelson, Benjamin H.; Stegner, Aaron J.; Lange, Gudrun; Khan, Sarah; Blate, Michelle; Sotolongo, Anays; DeLuca, Michelle; Van Doren, William W.; Helmer, Drew A. (October 1, 2021). "Vagal nerve stimulation as a possible non-invasive treatment for chronic widespread pain in Gulf Veterans with Gulf War Illness". Life Sciences. 282: 119805. doi:10.1016/j.lfs.2021.119805. ISSN 0024-3205.
- ↑ Traianos, E.; Dibnah, B.; Lendrem, D.; Clark, Y.; Macrae, V.; Slater, V.; Wood, K.; Storey, D.; Simon, B.; Blake, J.; Tarn, J. (June 1, 2021). "Ab0051 the Effects of Non-Invasive Vagus Nerve Stimulation on Immunological Responses and Patient Reported Outcome Measures of Fatigue in Patients with Chronic Fatigue Syndrome, Fibromyalgia, and Rheumatoid Arthritis". Annals of the Rheumatic Diseases. 80 (Suppl 1): 1057–1058. doi:10.1136/annrheumdis-2021-eular.1999. ISSN 0003-4967.
- ↑ Kutlu, Nazlı; Özden, Ali Veysel; Alptekin, Hasan Kerem; Alptekin, Jülide Öncü (March 2, 2020). "The Impact of Auricular Vagus Nerve Stimulation on Pain and Life Quality in Patients with Fibromyalgia Syndrome". BioMed Research International. 2020: e8656218. doi:10.1155/2020/8656218. ISSN 2314-6133.
- ↑ Kaniusas, Eugenijus; Kampusch, Stefan; Tittgemeyer, Marc; Panetsos, Fivos; Gines, Raquel Fernandez; Papa, Michele; Kiss, Attila; Podesser, Bruno; Cassara, Antonino Mario; Tanghe, Emmeric; Samoudi, Amine Mohammed (2019). "Current Directions in the Auricular Vagus Nerve Stimulation I – A Physiological Perspective". Frontiers in Neuroscience. 13: 854. doi:10.3389/fnins.2019.00854. ISSN 1662-453X. PMC 6697069. PMID 31447643.
- ↑ Kaniusas, Eugenijus; Kampusch, Stefan; Tittgemeyer, Marc; Panetsos, Fivos; Gines, Raquel Fernandez; Papa, Michele; Kiss, Attila; Podesser, Bruno; Cassara, Antonino Mario; Tanghe, Emmeric; Samoudi, Amine Mohammed (2019). "Current Directions in the Auricular Vagus Nerve Stimulation II – An Engineering Perspective". Frontiers in Neuroscience. 13. doi:10.3389/fnins.2019.00772/full. ISSN 1662-453X.
- ↑ Aranow, Cynthia; Atisha-Fregoso, Yemil; Lesser, Martin; Mackay, Meggan; Anderson, Erik; Chavan, Sangeeta; Zanos, Theodoros P.; Datta-Chaudhuri, Timir; Bouton, Chad; Tracey, Kevin J.; Diamond, Betty (February 1, 2021). "Transcutaneous auricular vagus nerve stimulation reduces pain and fatigue in patients with systemic lupus erythematosus: a randomised, double-blind, sham-controlled pilot trial". Annals of the Rheumatic Diseases. 80 (2): 203–208. doi:10.1136/annrheumdis-2020-217872. ISSN 0003-4967. PMID 33144299.
- ↑ Lange, Gudrun; Janal, Malvin N.; Maniker, Allen; FitzGibbons, Jennifer; Fobler, Malusha; Cook, Dane; Natelson, Benjamin H. (September 1, 2011). "Safety and Efficacy of Vagus Nerve Stimulation in Fibromyalgia: A Phase I/II Proof of Concept Trial". Pain Medicine. 12 (9): 1406–1413. doi:10.1111/j.1526-4637.2011.01203.x. ISSN 1526-2375. PMC 3173600. PMID 21812908.

