Epigenetics
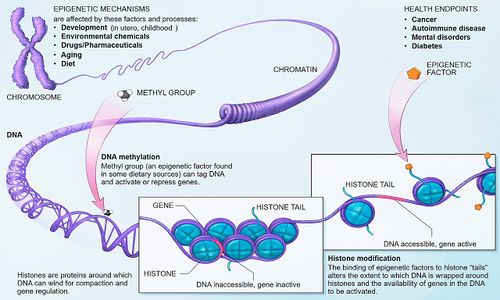
Epigenetics refers to how gene expression is influenced by our environment, e.g., everything we breathe, eat and put on our skin, along with physical and mental trauma. This environmental input affects which genes turn on and off, and when. External influences primarily work by triggering cellular processes such as methylation, acetylation, or phosphorylation. These simple chemical reactions affect the function of the gene.[1][2]
Epigenetic changes are thought to be a part of numerous diseases, such as cancer, asthma and heart disease,[3][4] as well as autoimmune disease.[5][6]
Gene on/off switch
- Aug 1, 2007, NOVA slideshow article by Nipam Patel, Gene Switches.
- Slide 9 of 9: Later in an animal's development, epigenetic switches take over. These epigenetic mechanisms act to maintain the fate of cells by doing what the Hox genes and other transcription factors did earlier, namely, controlling the "on" and "off" state of genes within each cell.
- Nov 10, 2016, Dr. Anthony Komaroff briefly discussed Epigenetics on November 10, 2016 on a Solve ME/CFS webinar. A gene can be normal and not mutated but it may not be turned on or off at the right time. Webinar with Dr. Anthony L. Komaroff @42:50
- Jul 19, 2018, Trans-NIH ME/CFS Working Group ME/CFS Advocacy Call. Recorded: @28.06 Dr. Anthony Komaroff with transcript.[7]
Now, let me turn to the exercise and orthostatic challenge studies that I mentioned. As Dr. Breen said earlier, there have been a variety of laboratory or biological abnormalities shown in patients with ME/CFS, including changes in the immune system, in metabolism in general, energy metabolism in particular, and epigenetic studies, epigenetic being shorthand for determining what genes are turned on and off and whether they're turned on and off appropriately.
So all of these different kinds of abnormalities have been demonstrated, but they’ve typically been demonstrated in people at rest. The question is, particularly in an illness like this one, where certain challenges like exercise or being upright for prolonged periods of time make the symptoms worse. It raises the question of whether those same challenges would make the laboratory abnormalities worse. Because all we can say now when we see a particular, let's say immune system abnormality, being abnormal in people with this illness at rest, we can say that it's there. But we can't really tell if it is cause or effect.
But if you show that when people do something like exercise, it makes them feel worse, that those certain metabolic abnormalities get worse along with the symptoms getting worse, it makes it more plausible that these laboratory abnormalities may actually be causal, may be actually contributing to the symptoms of the illness. And if that were true that would be good because they would represent targets for treatment interventions to try to prevent the symptoms from happening.
So that's the rationale for these studies. About 100 patients and healthy controls will be involved in four centers around the country, are involved already, and I think it has the potential to provide some important information.
Learn more
- Epigenetics - NOVA Science NOW Video 2007
- Investigator Report: Epigenetics of ME/CFS - Solve ME/CFS Initiative - Webinar August 21, 2014 "Think about our genetics, our heritiages as the hardware of our bodies... Epigenetics is like the software." "Epigenetics: Biological processes that control when, where and how our genes work." ~Patrick O. McGowan, Ph.D.
- Wikipedia
References
- ↑ Epigenetics Primer - PDF - The Scientist
- ↑ What is Epigenetics - Fundamentals
- ↑ 'Epigenetics' Means What We Eat, How We Live And Love, Alters How Our Genes Behave - Science Daily - Duke University Medical Cetner
- ↑ Epigenetic Influences and Disease - Scitable
- ↑ Harley, John (April 16, 2018). "Transcription factors operate across disease loci, with EBNA2 implicated in autoimmunity". Nature genetics.
- ↑ "Epstein-Barr virus protein can "switch on" risk genes for autoimmune diseases". National Institutes of Health. April 16, 2018.
- ↑ ME/CFS Advocacy Call - @28.06 and transcript. - July 19, 2018 - Dr. Anthony Komaroff - NIH - July 19, 2018

