Craniocervical instability
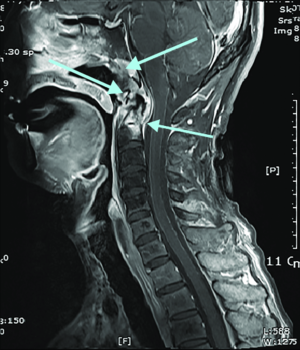
MRI of a patient's cervical spine, showing C1 and C2 radiation necrosis with C1-2 instability, cancer in the nasopharynx, and narrowing of the central canal at C1.
Source: Choi, Y., Woo, S. W., & Lee, J.H. (2018). Awake fiberoptic orotracheal intubation using a modified Guedel airway in a patient with craniocervical instability and an anticipated difficult airway: A case report. Anesthesia and Pain Medicine, 13(4), 383-387. Fig 1.[1] License: CC BY-NC-4.0
Craniocervical instability (CCI) is a pathological condition of increased mobility at the craniocervical junction, the area where the skull meets the spine. In CCI the ligamentous connections of the craniocervical junction can be stretched, weakened or ruptured.[2] This can lead to stretching and/or compression of the brainstem, upper spinal cord, or cerebellum and result in myelopathy, neck pain and a range of other symptoms.[3]
CCI can develop as a result of physical trauma such as a car accident, an inflammatory disease such as rheumatoid arthritis, a congenital disorder such as Down's syndrome[4], or infection[5][6][7][8]. More recently, physicians have reported an increased prevalence of CCI in patients with hereditary disorders of connective tissue such as Ehlers Danlos Syndromes (EDS).[9] There have also been anecdotal reports of patients with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) who were later diagnosed with CCI (as well as tethered cord syndrome),[10][11][12] although no scientific publication on this subject exists. It frequently co-occurs with atlantoaxial instability (AAI).[citation needed]
Symptoms[edit | edit source]
Symptoms of craniocervical instability include occipital headache, neck pain and neurological abnormalities such as numbness, motor weakness, dizziness, and gait instability.[13][14][15][16][17] Patients sometimes describe the feeling that their head is too heavy for their neck to support (“bobble-head”).[9] No particular symptom is mandatory for a diagnosis of CCI and each symptom listed might have a cause other than CCI.
Other symptoms reported in patients with CCI include:
- Muscle weakness,[18] numbness,[19][2] paralysis, paresthesias[18][20][21][22]
- Poor proprioception,[23] impaired coordination, gait changes[18][23]
- Dizziness, vertigo,[18][2][23][20][22][21] syncope,[18][19][2][23] nausea[19][2]
- Headache behind the eyes,[22] neck stiffness, torticollis,[23][24] posterior scalp irritation,[23] facial pain
- Apnea,[25][19][26] dyspnea (shortness of breath),[18][19] and dysphagia (difficulty swallowing)[19][2]
- Visual disturbances[20] downward nystagmus (irregular eye movements),[19][23] tinnitus[27][20]
- Fatigue,[18][28][29] Sleep dysfunction,[18][20] cognitive impairment,[20] and memory loss.
Risk factors and comorbidities[edit | edit source]
Established risk factors for CCI include physical trauma, infection, inflammatory disease, neoplasms and congenital disorders.[4][30]
More recently, physicians have reported an increased prevalence of CCI in patients with hereditary connective tissue disorders.[9] According to Brodbelt & Flint, however, an "increased range of joint movement, caused by ligamentous laxity, is not the same as spinal instability resulting from trauma or major inflammatory arthropathies such as (historically) rheumatoid arthritis."[31] Others have argued that "pathological instability at the cranio-cervical junction has not been clearly established in the literature for the joint hypermobility population."[9]
| Cause of instability | Example |
| Physical trauma[32] | Car accident[33][34], blow to the head.[35] |
| Infection & inflammatory disease | Upper respiratory infection[5][7], Rheumatoid arthritis[36], tuberculosis[8] |
| Neoplasms | Tumors[30] such as haemangioma, aneurysmal bone cyst |
| Congenital | Down’s syndrome[37], os odontoideum[38], dwarfism |
| Hereditary connective tissue disorder | Ehlers Danlos Syndromes[18][19] |
| Fluoroquinolones | Connective tissue weakening[39][40], tendon ruptures[41] |
It is not unusual for CCI to co-occur with other structural neurological abnormalities such as atlantoaxial instability (AAI) and chiari malformation (CM).[42][18]
Diagnosis[edit | edit source]
The diagnosis of CCI is based on symptom presentation, a supportive history, demonstrable neurological findings and abnormal imaging.
Imaging[edit | edit source]
CCI is typically diagnosed via a cervical MRI, whether supine or upright. If supine, a 3 Tesla MRI is preferred over a 1.5 Tesla. Most neurosurgeons prefer upright MRI with flexion and extension.[citation needed][43] According to Henderson FC, “ventral brainstem compression may exist in flexion of the cervical spine, but appear normal on routine imaging.”[9]
| Imaging | Sensitive for |
|---|---|
| Upright MRI with flexion/extension | Horizontal instability |
| CT scan with rotation | Rotational instability |
| Invasive cervical traction (ICT) with fluoroscopy | Vertical instability |
Measurements[edit | edit source]
More than twenty radiological measurements have been proposed or used in the diagnosis of CCI. However, three measurements are most commonly used: the Grabb-Oakes line, which measures ventral brainstem compression; the Clivo-Axial Angle (CXA), which measures brainstem deformity by the odontoid process; and the Basion Dens Interval, which measures vertical instability (cranial settling). According to a 2013 consensus statement on the assessment of CCI, a CXA of 135 degrees or less should be considered as "potentially pathological."[44] as it is reported to be uncommon in the healthy population.[45][46][47] Others have argued that these radiological measurements are "not accepted internationally as indicating instability."[31]
| Measurement | Units | Description | Normal Range | Borderline Range | Pathological Range | Alternate Ranges | Instability Measured | Pathology Measured | Refs |
|---|---|---|---|---|---|---|---|---|---|
| Clivo-axial angle (CXA) | Degrees | Angle between clivus line and the posterior axial line | 170 -150 | 149 -136 | ≤ 135 | More sensitive for horizontal | Brainstem deformity | [48] | |
| Grabb-Oakes | mm | Distance from the dura to the line drawn from the basion to the posterior inferior edge of the C2 vertebra | < 6 | ≥ 6 and < 9 | ≥ 9 | Some use pathological ≥ 8 | More sensitive for horizontal | Brainstem compression | [49][9] |
| Basion-Axial Interval (BAI) | mm | Distance from tip of basion to posterior axial line | < 12 | ≥ 12 | [50] | ||||
| Basion-Dens interval (BDI) | mm | Vertical distance between the basion and the dens | < 12 | ≥ 12 | Some use pathological ≥ 10 | Vertical | Cranial settling | [50][9] | |
| Translational BAI | mm | Change in BAI between flexion and extension positions of the head | < 1 | ≥ 1 and ≤ 2 | > 2 | For surgery > 4 needed | Horizontal | Skull sliding over spine | [51][18] |
| Translational BDI | mm | Change in BDI between flexion and extension positions of the head | |||||||
| Dynamic BDI | mm | Change in BDI value when the head is pulled upward with traction force of typically up to 35 lbs | Vertical | Cranial settling | |||||
| Dens Over Chamberlain | mm | How far tip of the dens extends above Chamberlain's line | < 2 | ≥ 2 and ≤ 3 | ≥ 3 | Vertical | Basilar invagination | date = 2022)) |
Some of the measurement ranges in the above table are also to be found in the 2nd International CSF Dynamics Symposium Consensus Statement (2013).[44]
Traction[edit | edit source]
Manual traction, halo and invasive cervical traction may be used to aid in the diagnosis of CCI. Symptomatic improvement with traction can help determine whether a patient with abnormal measurements will benefit from craniocervical fusion surgery.
Treatment[edit | edit source]
Conservative treatment[edit | edit source]
Traditional “conservative” treatments for CCI include rest, pain management, upper cervical chiropractic treatment, and bracing with a cervical collar.[53] Although, in most cases these offer little relief. Physical therapy specific to CCI and individual symptoms can also help in cases where life-threatening symptoms aren’t a risk.
Other experimental treatments for CCI include prolotherapy, platelet rich plasma, and stem cell therapy.
Surgery[edit | edit source]
If non-invasive treatments for CCI fail to work, occipito-cervical fusion (OCF) can be considered.[18] OCF is a surgery that aims at a biomechanical stabilization of the craniocervical junction. Patients with objective radiological findings, a clinical picture supportive of the diagnosis, a positive response to traction, and who are significantly impaired may be candidates for this surgery. A common method involves internal fixation of the upper spine to the skull by mechanical rods and screws. (However, rod-wire, rigid rod-screws, occipital hooks and cervical claws are all methods currently in use.[54]) During surgery, titanium hardware is used to fixate the occiput, axis and atlas (i.e., C0 to C2) while rib graft, cadaver bone graft or synthetic bone is used to help the bones fuse together. Wire methods are less biomechanically stable than rod methods and have high rates of dural laceration.[54] Screw and rod fixation methods have lower complication rates and higher rates of successful fusion.[55] Fusion rates across all hardware methods range from 89 to 100%.[54] When cervical instability is present below C2, additional vertebrae may also be fused.
Outcomes, risks & complications[edit | edit source]
Little research on outcomes exists. In a small case study of 20 patients, the five-year outcome of OCF was generally favorable with most patients experiencing symptom relief post-surgery.[18] In this study, following 20 EDS patients five years free O-2 fusion, most reported they were satisfied with the surgery and experienced significant improvements in symptoms such as vertigo, headaches, imbalance, dysarthria, dizziness, and frequent daytime urination. There was, however, only a small increase in objective outcomes such as work resumption, with 60% of patients remaining unable to work or go to school. Participants attributed this to other EDS comorbidities such as POTS, Mast Cell Activation Syndrome, and additional spinal problems.[18]
The complications of OCF can be serious[56] and occur in an estimated 7% to 33% of patients.[4][55][3][57][54] Common complications include screw failure, wound infection, dural tear and cerebrospinal fluid leakage[3] In some cases revision surgery is needed to treat infection or to remove hardware. Severe complications can include meningitis and accidental injury of the vertebral artery by misplaced screws.[58]
A meta-study of 2274 procedures across 22 studies[54] found the following complication rates:
| Complication type | Prevalence rate |
|---|---|
| Hardware failure after fusion non-union | 7% |
| Wound infection | 3.8%-11% |
| Vertebral artery damage | 1.3%-4.1% |
| Dural tears | 0% to 4.2% |
Meta-studies place the rate of death from fusion surgery at 0-0.6%.[54][55]
Side effects[edit | edit source]
OCF causes a substantial reduction in the neck’s range of motion, estimated at approximately 40% of total cervical flexion–extension.[59]
Cost[edit | edit source]
OCF is estimated to cost tens of thousands of dollars, although some insurance schemes fully cover the cost of surgery depending on the country located and neurosurgeons involved.
Experimental treatments[edit | edit source]
- Stem cell therapy: Some clinics offer stem cell therapy in order to regenerate the area, ligaments, connective and other tissues that may be damaged in the area. The Centeno-Schultz Clinic offers bone marrow concentrate directed toward the problematic ligaments or structures using imaging guidance. This treatment contains the patient's own stem cells.[60]
- Platelet-Rich Plasma therapy (PRP therapy): Some clinics offer PRP therapy in order to help the body regenerate the area, e.g. Regenexx clinic.[61][62]
- Percutaneous implantation of the CCJ ligaments (PICL): A non-surgical treatment involving injecting your own bone marrow concentrate using dual c-arm guidance, endoscopy, and a 3-D printed mouthpiece to strengthen the alar/transverse and other internal ligaments.[63]
Dysautonomia and CCI in EDS[edit | edit source]
As CCI can lead to a compression of the brainstem, a number of experts believe it contributes to autonomic symptoms such as orthostatic tachycardia, dizziness and pre-/syncope that are frequently seen in patients with Ehlers Danlos Syndromes (EDS). In a 2007 influential paper Milhorat et al. followed-up on patients with Chiari malformation who did not improve with treatment and surgery. The authors discovered that many of these patients suffered from EDS and had other structural abnormalities at the upper spine such as CCI and cranial settling. Milhorat et al. speculated that the resulting compression of the brainstem might be the cause of the autonomic and other symptoms these patients were suffering from.[64] Neurosurgeons and other EDS specialists have expounded on the connection between CCI and forms of dysautonomia such as postural orthostatic tachycardia syndrome (POTS) in a number of conference presentations. [65][66][44]
Mechanical basis theory[edit | edit source]
This theory was developed and proposed by Jeffrey Wood in 2018. The central idea is that mechanical deformation of the brainstem, due to CCI or other underlying structural conditions, can account for the dysfunction seen in ME/CFS: Dysautonomia, immune system dysregulation, viral persistence, post-exertional malaise, and others. Research into this concept is in development. A sizable number of ME/CFS patients diagnosed with CCI (some also had EDS) reported to have experienced remarkable improvements and even remission of their ME/CFS symptoms following OCF-surgery.[67][68] Some have raised concerns about CCI surgery in patients with ME/CFS given the lack of research on OCF in this patient population.[69]
Synonyms[edit | edit source]
- Syndrome of Occipitoatlantialaxial Hypermobility[19]
- Hypermobility of the Craniocervical Junction[70]
- Craniocervical Junction Syndrome
See also[edit | edit source]
- Atlantoaxial instability (AAI)
- Neural strain
- Chiari malformation
- Ehlers-Danlos syndrome
- Intracranial hypertension
- Tethered cord syndrome
Learn more[edit | edit source]
- Could Craniocervical Instability Be Causing ME/CFS, Fibromyalgia & POTS? Pt I – The Spinal Series - from Health Rising
- Jennifer Brea’s Amazing ME/CFS Recovering Story: the Spinal Series – Pt. II - From Health Rising
- ME/CFS and Fibromyalgia Craniocervical Instability Surgery Effectiveness Poll - From Health Rising
References[edit | edit source]
- ↑ Choi, Yongjoon; Woo, Sung-won; Lee, Ji Heui (October 31, 2018). "Awake fiberoptic orotracheal intubation using a modified Guedel airway in a patient with craniocervical instability and an anticipated difficult airway - A case report -". Anesthesia and Pain Medicine. 13 (4): 383–387. doi:10.17085/apm.2018.13.4.383. ISSN 2383-7977.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Henderson, Fraser C.; Austin, Claudiu; Benzel, Edward; Bolognese, Paolo; Ellenbogen, Richard; Francomano, Clair A.; Ireton, Candace; Klinge, Petra; Koby, Myles (2017). "Neurological and spinal manifestations of the Ehlers–Danlos syndromes". American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 175 (1): 195–211. doi:10.1002/ajmg.c.31549. ISSN 1552-4876.
- ↑ 3.0 3.1 3.2 Choi, Sung Ho; Lee, Sang Gu; Park, Chan Woo; Kim, Woo Kyung; Yoo, Chan Jong; Son, Seong (April 2013). "Surgical Outcomes and Complications after Occipito-Cervical Fusion Using the Screw-Rod System in Craniocervical Instability". Journal of Korean Neurosurgical Society. 53 (4): 223–227. doi:10.3340/jkns.2013.53.4.223. ISSN 2005-3711. PMC 3698232. PMID 23826478.
- ↑ 4.0 4.1 4.2 Ashafai, Nabeel S.; Visocchi, Massimiliano; Wąsik, Norbert (2019). "Occipitocervical Fusion: An Updated Review". Acta Neurochirurgica. Supplement. 125: 247–252. doi:10.1007/978-3-319-62515-7_35. ISSN 0065-1419. PMID 30610329.
- ↑ 5.0 5.1 Hettiaratchy, Shehan; Ning, Chou; Sabin, Ian (July 1, 1998). "Nontraumatic Atlanto-occipital and Atlantoaxial Rotatory Subluxation: Case Report". Neurosurgery. 43 (1): 162–164. doi:10.1097/00006123-199807000-00110. ISSN 0148-396X.
- ↑ "Atlantoaxial Instability: Practice Essentials, Pathophysiology, Etiology". July 17, 2023. Cite journal requires
|journal=(help) - ↑ 7.0 7.1 Washington, Eleby R. (March 1959). "Non-Traumatic Atlanto-Occipital and Atlanto-Axial Dislocation: A Case Report". JBJS. 41 (2): 341–344. ISSN 0021-9355.
- ↑ 8.0 8.1 Chaudhary, Kshitij; Potdar, Prabodhan; Bapat, Mihir; Rathod, Ashok; Laheri, Vinod (June 15, 2012). "Structural odontoid lesions in craniovertebral tuberculosis: a review of 15 cases". Spine. 37 (14): E836–843. doi:10.1097/BRS.0b013e31824a4c8f. ISSN 1528-1159. PMID 22261632.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Henderson, Fraser C. (2016). "Cranio-cervical Instability in Patients with Hypermobility Connective Disorders". Journal of Spine. 05 (02). doi:10.4172/2165-7939.1000299. ISSN 2165-7939.
- ↑ "Have you ruled out Chiari as a cause of your CFS". Phoenix Rising.
- ↑ Brea, Jennifer (June 6, 2019). "CCI + Tethered cord series". Medium. Retrieved June 6, 2019.
- ↑ "Craniocervical instability, Atlantoaxial Instability, Myalgic Encephalomyelitis, ME, CFS". MEchanical Basis. Retrieved June 6, 2019.
- ↑ Bobinski, Lukas; Levivier, Marc; Duff, John M. (February 2015). "Occipitoaxial spinal interarticular stabilization with vertebral artery preservation for atlantal lateral mass failure". Journal of Neurosurgery Spine. 22 (2): 134–138. doi:10.3171/2014.10.SPINE14131. ISSN 1547-5646. PMID 25415481.
- ↑ O'Brien, Michael F.; Casey, Adrian T.H.; Crockard, Alan; Pringle, Jean; Stevens, John M. (October 15, 2002). "Histology of the craniocervical junction in chronic rheumatoid arthritis: a clinicopathologic analysis of 33 operative cases". Spine. 27 (20): 2245–2254. doi:10.1097/01.BRS.0000029252.98053.43. ISSN 1528-1159. PMID 12394902.
- ↑ Young, Richard M.; Sherman, Jonathan H.; Wind, Joshua J.; Litvack, Zachary; O'Brien, Joseph (August 2014). "Treatment of craniocervical instability using a posterior-only approach: report of 3 cases". Journal of Neurosurgery. Spine. 21 (2): 239–248. doi:10.3171/2014.3.SPINE13684. ISSN 1547-5646. PMID 24785968.
- ↑ Botelho, Ricardo V.; Neto, Eliseu B.; Patriota, Gustavo C.; Daniel, Jefferson W.; Dumont, Paulo A.S.; Rotta, José M. (October 2007). "Basilar invagination: craniocervical instability treated with cervical traction and occipitocervical fixation. Case report". Journal of Neurosurgery. Spine. 7 (4): 444–449. doi:10.3171/SPI-07/10/444. ISSN 1547-5654. PMID 17933321.
- ↑ Henderson, Fraser C.; Henderson, Fraser C.; Wilson, William A.; Mark, Alexander S.; Koby, Myles (January 2018). "Utility of the clivo-axial angle in assessing brainstem deformity: pilot study and literature review". Neurosurgical Review. 41 (1): 149–163. doi:10.1007/s10143-017-0830-3. ISSN 1437-2320. PMC 5748419. PMID 28258417.
- ↑ 18.00 18.01 18.02 18.03 18.04 18.05 18.06 18.07 18.08 18.09 18.10 18.11 18.12 18.13 Henderson, Fraser C.; Francomano, C.A.; Koby, M.; Tuchman, K.; Adcock, J.; Patel, S. (January 9, 2019). "Cervical medullary syndrome secondary to craniocervical instability and ventral brainstem compression in hereditary hypermobility connective tissue disorders: 5-year follow-up after craniocervical reduction, fusion, and stabilization". Neurosurgical Review. 92: 915–936. doi:10.1007/s10143-018-01070-4. ISSN 1437-2320.
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 19.7 19.8 Francomano, Clair A.; McDonnell, Nazli B.; Nishikawa, Misao; Bolognese, Paolo A.; Milhorat, Thomas H. (December 1, 2007). "Syndrome of occipitoatlantoaxial hypermobility, cranial settling, and Chiari malformation Type I in patients with hereditary disorders of connective tissue". Journal of Neurosurgery: Spine. 7 (6): 601–609. doi:10.3171/SPI-07/12/601.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 "MRI video diagnosis and surgical therapy of soft tissue trauma to the craniocervical junction - ProQuest". search.proquest.com. Retrieved June 1, 2019.
- ↑ 21.0 21.1 Rebbeck, Trudy; Liebert, Ann (December 1, 2014). "Clinical management of cranio-vertebral instability after whiplash, when guidelines should be adapted: A case report". Manual Therapy. 19 (6): 618–621. doi:10.1016/j.math.2014.01.009. ISSN 1356-689X.
- ↑ 22.0 22.1 22.2 Mathers, K. Sean; Schneider, Michael; Timko, Michael (June 2011). "Occult Hypermobility of the Craniocervical Junction: A Case Report and Review". Journal of Orthopaedic & Sports Physical Therapy. 41 (6): 444–457. doi:10.2519/jospt.2011.3305. ISSN 0190-6011.
- ↑ 23.0 23.1 23.2 23.3 23.4 23.5 23.6 Bergholm, Ulla; Johansson, Bengt H.; Johansson, Hakan (January 1, 2004). "New Diagnostic Tools Can Contribute to Better Treatment of Patients with Chronic Whiplash Disorders". Journal of Whiplash & Related Disorders. 3 (2): 5–19. doi:10.3109/J180v03n02_02. ISSN 1533-2888.
- ↑ Ghanem, Ismat; El Hage, Samer; Rachkidi, Rami; Kharrat, Khalil; Dagher, Fernand; Kreichati, Gabi (March 1, 2008). "Pediatric cervical spine instability". Journal of Children's Orthopaedics. 2 (2): 71–84. doi:10.1007/s11832-008-0092-2. ISSN 1863-2521. PMC 2656787. PMID 19308585.
- ↑ Janjua, M. Burhan; Hwang, Steven W.; Samdani, Amer F.; Pahys, Joshua M.; Baaj, Ali A.; Härtl, Roger; Greenfield, Jeffrey P. (January 1, 2019). "Instrumented arthrodesis for non-traumatic craniocervical instability in very young children". Child's Nervous System. 35 (1): 97–106. doi:10.1007/s00381-018-3876-9. ISSN 1433-0350.
- ↑ Henderson, Fraser C.; Austin, Claudiu; Benzel, Edward; Bolognese, Paolo; Ellenbogen, Richard; Francomano, Clair A.; Ireton, Candace; Klinge, Petra; Koby, Myles (2017). "Neurological and spinal manifestations of the Ehlers–Danlos syndromes". American Journal of Medical Genetics Part C: Seminars in Medical Genetics. 175 (1): 195–211. doi:10.1002/ajmg.c.31549. ISSN 1552-4876.
- ↑ Montazem, Abbas (2000). "Secondary tinnitus as a symptom of instability in the upper cervical spine: Operative management" (PDF). International Tinnitus Journal. 6 (2): 130–3. PMID 14689631.
- ↑ Henderson, Fraser C.; Henderson, Fraser C.; Wilson, William A.; Mark, Alexander S.; Koby, Myles (January 1, 2018). "Utility of the clivo-axial angle in assessing brainstem deformity: pilot study and literature review". Neurosurgical Review. 41 (1): 149–163. doi:10.1007/s10143-017-0830-3. ISSN 1437-2320. PMC 5748419. PMID 28258417.
- ↑ Henderson, Fraser C.; Wilson, William A.; Mott, Stephen; Mark, Alexander; Schmidt, Kristi; Berry, Joel K.; Vaccaro, Alexander; Benzel, Edward (July 16, 2010). "Deformative stress associated with an abnormal clivo-axial angle: A finite element analysis". Surgical Neurology International. 1. doi:10.4103/2152-7806.66461. ISSN 2152-7806. PMC 2940090. PMID 20847911.
- ↑ 30.0 30.1 Sapkas, George; Papadakis, Stamatios A; Segkos, Dimitrios; Kateros, Konstantinos; Tsakotos, George; Katonis, Pavlos (June 2, 2011). "Posterior Instrumentation for Occipitocervical Fusion". The Open Orthopaedics Journal. 5: 209–218. doi:10.2174/1874325001105010209. ISSN 1874-3250. PMC 3139273. PMID 21772931.
- ↑ 31.0 31.1 Brodbelt, Andrew R.; Flint, Graham (August 2017). "Ehlers Danlos, complex Chiari and cranio-cervical fixation: how best should we treat patients with hypermobility?". British Journal of Neurosurgery. 31 (4): 397–398. doi:10.1080/02688697.2017.1386282. ISSN 1360-046X. PMID 28961036.
- ↑ Ghatan, Saadi; Newell, David W.; Grady, M. Sean; Mirza, Sohail K.; Chapman, Jens R.; Mann, Frederick A.; Ellenbogen, Richard G. (August 2004). "Severe posttraumatic craniocervical instability in the very young patient. Report of three cases". Journal of Neurosurgery. 101 (1 Suppl): 102–107. doi:10.3171/ped.2004.101.2.0102. ISSN 0022-3085. PMID 16206980.
- ↑ Uribe, Juan S.; Ramos, Edwin; Baaj, Ali; Youssef, A. Samy; Vale, Fernando L. (December 2009). "Occipital cervical stabilization using occipital condyles for cranial fixation: technical case report". Neurosurgery. 65 (6): E1216–1217, discussion E1217. doi:10.1227/01.NEU.0000349207.98394.FA. ISSN 1524-4040. PMID 19934947.
- ↑ Volle, E.; Montazem, A. (January 2001). "MRI video diagnosis and surgical therapy of soft tissue trauma to the craniocervical junction". Ear, Nose, & Throat Journal. 80 (1): 41–44, 46–48. ISSN 0145-5613. PMID 11209518.
- ↑ Mathers, K. Sean; Schneider, Michael; Timko, Michael (June 2011). "Occult hypermobility of the craniocervical junction: a case report and review". The Journal of Orthopaedic and Sports Physical Therapy. 41 (6): 444–457. doi:10.2519/jospt.2011.3305. ISSN 1938-1344. PMID 21628827.
- ↑ O'Brien, Michael F.; Casey, Adrian T.H.; Crockard, Alan; Pringle, Jean; Stevens, John M. (October 15, 2002). "Histology of the craniocervical junction in chronic rheumatoid arthritis: a clinicopathologic analysis of 33 operative cases". Spine. 27 (20): 2245–2254. doi:10.1097/01.BRS.0000029252.98053.43. ISSN 1528-1159. PMID 12394902.
- ↑ Hankinson, Todd C.; Anderson, Richard C.E. (March 2010). "Craniovertebral junction abnormalities in Down syndrome". Neurosurgery. 66 (3 Suppl): 32–38. doi:10.1227/01.NEU.0000365803.22786.F0. ISSN 1524-4040. PMID 20173525.
- ↑ Zhao, Deng; Wang, Shenglin; Passias, Peter G.; Wang, Chao (May 2015). "Craniocervical instability in the setting of os odontoideum: assessment of cause, presentation, and surgical outcomes in a series of 279 cases". Neurosurgery. 76 (5): 514–521. doi:10.1227/NEU.0000000000000668. ISSN 1524-4040. PMID 25635883.
- ↑ Etminan, M.; Sodhi, M.; Ganjizadeh-Zavareh, S.; Carleton, B.; Kezouh, A.; Brophy, J.M. (September 17, 2019). "Oral Fluoroquinolones and Risk of Mitral and Aortic Regurgitation". Journal of the American College of Cardiology. 74 (11): 1444–1450. doi:10.1016/j.jacc.2019.07.035. ISSN 0735-1097.
- ↑ Demetrious, James S. (July 9, 2018). "Spontaneous cervical artery dissection: a fluoroquinolone induced connective tissue disorder?". Chiropractic & Manual Therapies. 26 (1): 22. doi:10.1186/s12998-018-0193-z. ISSN 2045-709X.
- ↑ Stephenson, Anne L.; Wu, Wei; Cortes, Daniel; Rochon, Paula A. (September 2013). "Tendon Injury and Fluoroquinolone Use: A Systematic Review". Drug Safety. 36 (9): 709–721. doi:10.1007/s40264-013-0089-8. ISSN 1179-1942. PMID 23888427.
- ↑ Camino Willhuber, Gaston O.; Bosio, Santiago T.; Puigdevall, Miguel H.; Halliburton, Carolina; Sola, Carlos A.; Maenza, Ruben A. (January 2017). "Craniocervical spinal instability after type 1 Arnold Chiari decompression: a case report". Journal of Pediatric Orthopedics. Part B. 26 (1): 80–85. doi:10.1097/BPB.0000000000000346. ISSN 1473-5865. PMID 27258364.
- ↑ "Craniocervical instability, Atlantoaxial Instability, Myalgic Encephalomyelitis, ME, CFS". MEchanical Basis. Retrieved June 2, 2019.
- ↑ 44.0 44.1 44.2 CSF, Bobby Jones |. "REVIEW OF THE 2013 CSF RESEARCH COLLOQUIUM & CONSENSUS ON CRANIOCERVICAL INSTABILITY – Bobby Jones CSF". Retrieved September 18, 2019.
- ↑ Batista, Ulysses C.; Joaquim, Andrei F.; Fernandes, Yvens B.; Mathias, Roger N.; Ghizoni, Enrico; Tedeschi, Helder (April 2015). "Computed tomography evaluation of the normal craniocervical junction craniometry in 100 asymptomatic patients". Neurosurgical Focus. 38 (4): E5. doi:10.3171/2015.1.FOCUS14642. ISSN 1092-0684. PMID 25828499.
- ↑ Botelho, Ricardo Vieira; Ferreira, Edson Dener Zandonadi (October 2013). "Angular craniometry in craniocervical junction malformation". Neurosurgical Review. 36 (4): 603–610, discussion 610. doi:10.1007/s10143-013-0471-0. ISSN 1437-2320. PMC 3910287. PMID 23640096.
- ↑ Bundschuh, C; Modic, Mt; Kearney, F; Morris, R; Deal, C (July 1, 1988). "Rheumatoid arthritis of the cervical spine: surface-coil MR imaging". American Journal of Roentgenology. 151 (1): 181–187. doi:10.2214/ajr.151.1.181. ISSN 0361-803X.
- ↑ Bolognese, Paolo (2014). "Videoed Presentation at: ASAP Chiari & Syringomyelia Conference Paolo Bolognese, MD "Complex Chiari. Timecode 14:28". YouTube.
- ↑ Bolognese, Paolo (April 12, 2018). "Videoed presentation at: EDS Awareness Educational Series. Timecodes: 49:30 and 53:47". YouTube.
- ↑ 50.0 50.1 Henderson, Fraser. "Videoed presentation at: Chiari & Syringomyelia Foundation, Patient Conference of Action, June 24, 2018. Timecode: 10:34".
- ↑ Henderson, Fraser C.; Francomano, C.A.; Koby, M.; Tuchman, K.; Adcock, J.; Patel, S. (January 9, 2019). "Cervical medullary syndrome secondary to craniocervical instability and ventral brainstem compression in hereditary hypermobility connective tissue disorders: 5-year follow-up after craniocervical reduction, fusion, and stabilization". Neurosurgical Review. doi:10.1007/s10143-018-01070-4. ISSN 1437-2320.
- ↑ Hain, Timothy C. "Basilar Invagination, Basilar Impression and Atlantoaxial Subluxation". dizziness-and-balance.com.
- ↑ Mathers, K. Sean; Schneider, Michael; Timko, Michael (June 2011). "Occult hypermobility of the craniocervical junction: a case report and review". The Journal of Orthopaedic and Sports Physical Therapy. 41 (6): 444–457. doi:10.2519/jospt.2011.3305. ISSN 1938-1344. PMID 21628827.
- ↑ 54.0 54.1 54.2 54.3 54.4 54.5 Resnick, Daniel K.; Patel, Nirav J.; Lall, Rishi (November 1, 2010). "A Review of Complications Associated With Craniocervical Fusion Surgery". Neurosurgery. 67 (5): 1396–1403. doi:10.1227/NEU.0b013e3181f1ec73. ISSN 0148-396X.
- ↑ 55.0 55.1 55.2 Winegar, Corbett D.; Lawrence, James P.; Friel, Brian C.; Fernandez, Carmella; Hong, Joseph; Maltenfort, Mitchell; Anderson, Paul A.; Vaccaro, Alexander R. (July 2010). "A systematic review of occipital cervical fusion: techniques and outcomes". Journal of Neurosurgery. Spine. 13 (1): 5–16. doi:10.3171/2010.3.SPINE08143. ISSN 1547-5646. PMID 20594011.
- ↑ Garrido, Ben J.; Sasso, Rick C. (January 2012). "Occipitocervical fusion". The Orthopedic Clinics of North America. 43 (1): 1–9, vii. doi:10.1016/j.ocl.2011.08.009. ISSN 1558-1373. PMID 22082624.
- ↑ Ando, Kei; Imagama, Shiro; Ito, Zenya; Kobayashi, Kazuyoshi; Yagi, Hideki; Shinjo, Ryuichi; Hida, Tetsuro; Ito, Kenyu; Ishikawa, Yoshimoto (June 2017). "Minimum 5-year Follow-up Results for Occipitocervical Fusion Using the Screw-Rod System in Craniocervical Instability". Clinical Spine Surgery. 30 (5): E628–E632. doi:10.1097/BSD.0000000000000199. ISSN 2380-0194. PMID 28525489.
- ↑ Nockels, Russ P.; Shaffrey, Christopher I.; Kanter, Adam S.; Azeem, Syed; York, Julie E. (August 2007). "Occipitocervical fusion with rigid internal fixation: long-term follow-up data in 69 patients". Journal of Neurosurgery. Spine. 7 (2): 117–123. doi:10.3171/SPI-07/08/117. ISSN 1547-5654. PMID 17688049.
- ↑ Ashafai, Nabeel S.; Visocchi, Massimiliano; Wąsik, Norbert (2019). Visocchi, Massimiliano (ed.). Occipitocervical Fusion: An Updated Review. Acta Neurochirurgica Supplement. Cham: Springer International Publishing. pp. 247–252. doi:10.1007/978-3-319-62515-7_35. ISBN 9783319625157.
- ↑ https://centenoschultz.com/cervical-joint-degeneration/
- ↑ https://regenexx.com/blog/candidacy-for-ccj-instability-procedure/
- ↑ https://www.nwrestorativemedicine.com/pain-solutions/neck-pain/
- ↑ https://centenoschultz.com/craniocervical-instability-cci/
- ↑ Milhorat, Thomas H.; Bolognese, Paolo A.; Nishikawa, Misao; McDonnell, Nazli B.; Francomano, Clair A. (December 2007). "Syndrome of occipitoatlantoaxial hypermobility, cranial settling, and chiari malformation type I in patients with hereditary disorders of connective tissue". Journal of Neurosurgery. Spine. 7 (6): 601–609. doi:10.3171/SPI-07/12/601. ISSN 1547-5654. PMID 18074684.
- ↑ Craniocervical Instability (Dr Henderson the 2012 EDNF Confrence). Minute 12.10.
- ↑ Dr Milhorat from The Chiari Institute at the 2005 ASAP.
- ↑ "Craniocervical instability, Atlantoaxial Instability, Myalgic Encephalomyelitis, ME, CFS". MEchanical Basis. Retrieved June 6, 2019.
- ↑ Brea, Jennifer (May 20, 2019). "Health update #3: My ME is in remission". Medium. Retrieved June 3, 2019.
- ↑ "Concerns about craniocervical instability surgery in ME/CFS". Science for ME. Retrieved June 3, 2019.
- ↑ Mathers, K. Sean; Schneider, Michael; Timko, Michael (June 2011). "Occult hypermobility of the craniocervical junction: a case report and review". The Journal of Orthopaedic and Sports Physical Therapy. 41 (6): 444–457. doi:10.2519/jospt.2011.3305. ISSN 1938-1344. PMID 21628827.

