Dysautonomia
Dysautonomia describes several different medical disorders of the autonomic nervous system that cause disturbances in all or some autonomic functions.[1] Dysautonomia can be caused by other disease (e.g., diabetes), or by injury or poisoning/toxins, by genetics, or may not have a known cause.[1][2] People with dysautonomia can have problems regulating autonomic functions, including heart rate, blood pressure, body temperature, and digestion. Thus, dysautonomia can present with various symptoms, such as lightheadedness, fainting, unstable blood pressure, and orthostatic intolerance.[2]
Types of dysautonomia[edit | edit source]
More than 70 million people have dysautonomia. There are various types of dysautonomia, each presenting with different underlying mechanisms as well as some overlapping mechanisms. Forms of dysautonomia include:
- Postural orthostatic tachycardia syndrome (POTS), a form of orthostatic intolerance that can cause lightheadedness, fainting, tachycardia, chest pains, exercise intolerance, temperature sensitivity, and more.
- Neurocardiogenic syncope is the most common form of dysautonomia, with many individuals having a mild case (fainting once or twice in their lifetime). Severe cases can result in fainting several times per day.
- Multiple system atrophy (MSA), a fatal and rare form of dysautonomia, affects 350,000 people worldwide. It is a neurodegenerative disorder occurring in adults over the age of 40. MSA progresses rapidly; patients usually become bedridden within 2 years of diagnosis.
- Familial dysautonomia (FD) is a rare genetic disorder in persons of Ashkenazi Jewish descent. It is a very serious condition, consisting of abnormal development, progressive degeneration of the sensory and autonomic nervous systems, and is inevitably fatal. FD is caused by a point mutation in the IKBAP gene, resulting in the severe reduction of the IKAP protein, which is involved in many intracellular processes.[3]
- Autonomic dysreflexia (AD) is a form of dysautonomia associated with spinal cord injuries, affecting the communication of the autonomic nervous system.
- Baroreflex failure; the baroreflex is the body’s homeostatic mechanism for maintaining blood pressure. If the baroreceptor or its system fails, patients experience inappropriate blood pressure.
- Cerebral salt wasting syndrome is a condition in response to physical injury or the presence of tumors in the brain, presenting as hyponatremia (excessive sodium secretion from the kidney) and dehydration.
- Diabetic autonomic neuropathy is a very common form of dysautonomia, affecting 69 million people worldwide (20% of diabetics). It is a serious complication of diabetes, associated with an increased risk of cardiovascular mortality.
- Panayiotopoulos syndrome, also known as autonomic epilepsy is a childhood-specific seizure disorder consisting of seizures with predominantly autonomic symptoms (without convulsing).[4]
- Reflex sympathetic dystrophy is a an extremely painful neurological condition that is sometimes considered a form of dysautonomia.
Dysautonomia can occur independently or secondary to other medical conditions, such as diabetes, MS, rheumatoid arthritis, and lupus.[2]
Comorbidities/causes of dysautonomia[edit | edit source]
Comorbidities and causes of dysautonomia include:[2]
- Amyloidosis
- A group of rare disorders caused by the accumulation of amyloid protein in various tissues throughout the body. If the amyloid accumulation occurs in the heart or on peripheral nerves, it can cause dysautonomia.
- Celiac disease
- Charcot-Marie-Tooth disease
- Chiari malformation
- Chronic inflammatory demyelinating polyneuropathy
- Inflammatory bowel disease (such as Crohn’s and ulcerative colitis)[5][6]
- Deconditioning
- The physical change in the way the body functions due to a decrease in activity. The most common cause of deconditioning is bed rest. Due to debilitating symptoms, patients with various chronic illnesses may experience deconditioning, which can exacerbate symptoms. It is important to take steps to prevent and/or reverse deconditioning. [7]
- Diabetes[8]
- Ehlers-Danlos syndrome[9]
- Mast cell disorders
- Mitochondrial diseases[10]
- Paraneoplastic syndrome[11]
- Parkinson's disease[12]
- Sarcoidosis[13]
- Sjögren's syndrome[14]
- Physical trauma or surgery[15][16]
- Vitamin deficiencies
- Patients have also reported dysautonomia caused by viruses
Treatment[edit | edit source]
There are currently no cures for dysautonomia, as it is an umbrella term that covers many conditions related to the dysfunction of the autonomic system. Therefore, there are treatments that are used to improve quality of life by treating specific symptoms, or treating the underlying disease that is causing the dysautonomia. Further treatments are used to improve quality of life.[2]
Myalgic Encephalomyelitis[edit | edit source]
Many people with myalgic encephalomyelitis (ME) experience autonomic dysfunction. Symptoms of autonomic dysfunction in ME include altered blood pressure, heart rate, digestion, body temperature, exercise intolerance, and neurological correlates with autonomic nervous system (ANS) dysfunction (for a complete list, see our Autonomic Nervous System page).
Some researchers suggest that dysautonomia is central to the pathophysiology of ME.[18] Various studies have investigated the efficacy of treating ME patients by targeting autonomic symptoms without significant success.[19]
Studies on Dysautonomia and ME[edit | edit source]
One study (Orjatsalo et al. 2018) has looked at autonomic cardiac function in different sleep stages of people with chronic fatigue syndrome (CFS). They found that people with CFS had higher nocturnal systolic and mean BP and lower heart rate than controls, suggesting a nocturnal dysfunction of the cardiac ANS in CFS. This means that patients have a lower parasympathetic tone and higher sympathetic tone during sleep.[20]
Another study (Miwa 2016) investigated POTS in patients with both ME and orthostatic intolerance. They hypothesized that the characteristics of sympathetic activation may differ between these patients’ “good days” and “bad days”. Patients were characterized with an active standing test and an echocardiography. Their results indicated that ME patients may experience exaggerated activation of the sympathetic nervous system. They suggest that sympathetic activation in ME is impaired and is associated with preload failure.[21][22]
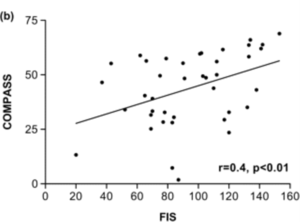
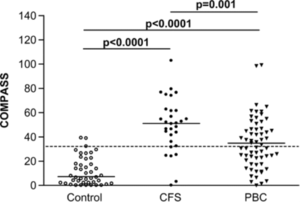
Newton et al. aimed to determine the prevalence of autonomic dysfunction in CFS using the Composite Autonomic Symptom Scale (COMPASS) and the Fatigue Impact Scale (FIS). The study included a healthy control group and a control group of patients with primary biliary cirrhosis (PBC; where 60% of patients experience significant fatigue and some experience autonomic dysfunction). Their results indicated that symptoms of autonomic dysfunction were strongly associated with the presence of CFS or PBC (in some but not all patients), and that symptoms correlated with severity of fatigue. COMPASS scores were significantly higher for the CFS group than for the PBC group and healthy control group.[17]
Ehlers-Danlos Syndrome[edit | edit source]
A study of 39 female Hypermobile EDS patients showed increased sympathetic activity at rest and reduced sympathetic reactivity to stimuli. It also showed an increased rate of orthostatic intolerance (74% in hEDS v. 34% in controls).[23] A study of hEDS patients found that 74.4% had Orthostatic Intolerance.[22] A study of 48 patients meeting the 1998 Brighton criteria found that 78% had orthostatic intolerance versus 10% of controls.[24]
Fibromyalgia[edit | edit source]
A symptom survey study comparing patients with EDS and fibromyalgia found that fibromyalgia patients had a much higher autonomic symptom burdens than controls, but similar to patients with EDS.[25]
See also[edit | edit source]
- Autonomic nervous system
- Dizziness
- Hypotension
- Neurally mediated hypotension
- Orthostatic intolerance
- Postural orthostatic tachycardia syndrome
References[edit | edit source]
- ↑ 1.0 1.1 "Definition of DYSAUTONOMIA". Merrian-Webster Medical Dictionary. Retrieved February 20, 2021.
- ↑ 2.0 2.1 2.2 2.3 2.4 "What is dysautonomia International". Dysautonomia International. Retrieved December 12, 2018.
- ↑ Dragatsis, Ioannis; Dietrich, Paula; Dragatsis, Ioannis; Dietrich, Paula (December 2016). "Familial Dysautonomia: Mechanisms and Models". Genetics and Molecular Biology. 39 (4): 497–514. doi:10.1590/1678-4685-gmb-2015-0335. ISSN 1415-4757.
- ↑ Covanis, Athanasios (October 1, 2006). "Panayiotopoulos Syndrome: A Benign Childhood Autonomic Epilepsy Frequently Imitating Encephalitis, Syncope, Migraine, Sleep Disorder, or Gastroenteritis". Pediatrics. 118 (4): e1237–e1243. doi:10.1542/peds.2006-0623. ISSN 1098-4275. PMID 16950946.
- ↑ Lindgren, S.; Lilja, B.; Rosén, I.; Sundkvist, G. (April 1991). "Disturbed autonomic nerve function in patients with Crohn's disease". Scandinavian Journal of Gastroenterology. 26 (4): 361–366. ISSN 0036-5521. PMID 2034989.
- ↑ Lindgren, S.; Stewenius, J.; Sjölund, K.; Lilja, B.; Sundkvist, G. (July 1993). "Autonomic vagal nerve dysfunction in patients with ulcerative colitis". Scandinavian Journal of Gastroenterology. 28 (7): 638–642. ISSN 0036-5521. PMID 8362220.
- ↑ Dyckman, Damian J.; Sauder, Charity L.; Ray, Chester A. (January 1, 2012). "Effects of short-term and prolonged bed rest on the vestibulosympathetic reflex". American Journal of Physiology. Heart and Circulatory Physiology. 302 (1): H368–374. doi:10.1152/ajpheart.00193.2011. ISSN 1522-1539. PMC 3334249. PMID 22021328.
- ↑ Vinik, Aaron I; Erbas, Tomris; Casellini, Carolina M (January 29, 2013). "Diabetic cardiac autonomic neuropathy, inflammation and cardiovascular disease". Journal of Diabetes Investigation. 4 (1): 4–18. doi:10.1111/jdi.12042. ISSN 2040-1116. PMC 3580884. PMID 23550085.
- ↑ Rowe, Peter C.; Barron, Diana F.; Calkins, Hugh; Maumenee, Irene H.; Tong, Patrick Y.; Geraghty, Michael T. (October 1, 1999). "Orthostatic intolerance and chronic fatigue syndrome associated with Ehlers-Danlos syndrome". The Journal of Pediatrics. 135 (4): 494–499. doi:10.1016/S0022-3476(99)70173-3. ISSN 0022-3476.
- ↑ Kanjwal, Khalil; Karabin, Beverly; Kanjwal, Yousuf; Saeed, Bilal; Grubb, Blair P. (October 2010). "Autonomic dysfunction presenting as orthostatic intolerance in patients suffering from mitochondrial cytopathy". Clinical Cardiology. 33 (10): 626–629. doi:10.1002/clc.20805. ISSN 1932-8737. PMID 20960537.
- ↑ Koike, Haruki; Tanaka, Fumiaki; Sobue, Gen (October 2011). "Paraneoplastic neuropathy: wide-ranging clinicopathological manifestations". Current Opinion in Neurology. 24 (5): 504–510. doi:10.1097/WCO.0b013e32834a87b7. ISSN 1473-6551. PMID 21799410.
- ↑ Goldstein, David S (April 2014). "Dysautonomia in Parkinson's disease: neurocardiological abnormalities". Comprehensive Physiology. 4 (2): 805–826. doi:10.1002/cphy.c130026. ISSN 2040-4603. PMC 4222515. PMID 24715569.
- ↑ Bakkers, M.; Faber, C.G.; Drent, M.; Hermans, M.C.E.; van Nes, S.I.; Lauria, G.; De Baets, M.; Merkies, I. S.J. (December 2010). "Pain and autonomic dysfunction in patients with sarcoidosis and small fibre neuropathy". Journal of Neurology. 257 (12): 2086–2090. doi:10.1007/s00415-010-5664-7. ISSN 0340-5354. PMC 2993892. PMID 20644950.
- ↑ Ng, W.-F.; Stangroom, A.J.; Davidson, A.; Wilton, K.; Mitchell, S.; Newton, J.L. (December 2012). "Primary Sjogrens syndrome is associated with impaired autonomic response to orthostasis and sympathetic failure". QJM: monthly journal of the Association of Physicians. 105 (12): 1191–1199. doi:10.1093/qjmed/hcs172. ISSN 1460-2393. PMC 3508582. PMID 22976617.
- ↑ Kanjwal, Khalil; Karabin, Beverly; Kanjwal, Yousuf; Grubb, Blair P. (2010). "Autonomic dysfunction presenting as postural tachycardia syndrome following traumatic brain injury". Cardiology Journal. 17 (5): 482–487. ISSN 1897-5593. PMID 20865679.
- ↑ Billakanty, Sreedhar R.; Kligman, MarkD.; Kanjwal, Yousuf M.; Kosinski, Daniel J.; Maly, George T.; Karabin, Beverly; Grubb, Blair P. (July 2008). "New-onset orthostatic intolerance following bariatric surgery". Pacing and clinical electrophysiology: PACE. 31 (7): 884–888. doi:10.1111/j.1540-8159.2008.01103.x. ISSN 1540-8159. PMID 18684286.
- ↑ 17.0 17.1 17.2 Jones, D. E.J.; Shin, J.; Seth, A.; Sutcliffe, K.; Okonkwo, O.; Newton, J.L. (August 1, 2007). "Symptoms of autonomic dysfunction in chronic fatigue syndrome". QJM: An International Journal of Medicine. 100 (8): 519–526. doi:10.1093/qjmed/hcm057. ISSN 1460-2725.
- ↑ Naschitz, Jochanan E; Yeshurun, Daniel; Rosner, Itzhak (February 2004). "Dysautonomia in chronic fatigue syndrome: facts, hypotheses, implications". Medical Hypotheses. 62 (2): 203–206. doi:10.1016/S0306-9877(03)00331-1. ISSN 0306-9877.
- ↑ Straus, Stephen E.; Wolff, Mark; Lucas, Katherine E.; Snader, Sally; Hohman, Patricia; Soto, Norberto; Cuccherini, Brenda A.; Sharma, Geetika; Anand, Ravinder (January 3, 2001). "Fludrocortisone Acetate to Treat Neurally Mediated Hypotension in Chronic Fatigue Syndrome: A Randomized Controlled Trial". JAMA. 285 (1): 52–59. doi:10.1001/jama.285.1.52. ISSN 0098-7484.
- ↑ Orjatsalo, Maija; Alakuijala, Anniina; Partinen, Markku (February 15, 2018). "Autonomic Nervous System Functioning Related to Nocturnal Sleep in Patients With Chronic Fatigue Syndrome Compared to Tired Controls". Journal of clinical sleep medicine: JCSM: official publication of the American Academy of Sleep Medicine. 14 (2): 163–171. doi:10.5664/jcsm.6924. ISSN 1550-9397. PMC 5786834. PMID 29246267.
- ↑ Miwa, Kunihisa (September 2016). "Variability of postural orthostatic tachycardia in patients with myalgic encephalomyelitis and orthostatic intolerance". Heart and Vessels. 31 (9): 1522–1528. doi:10.1007/s00380-015-0744-3. ISSN 1615-2573. PMID 26374335.
- ↑ 22.0 22.1 Malfait, Fransiska; Calders, Patrick; De Paepe, Anne; De Mits, Sophie; Da Silva, Hellen; Peersman, Wim; De Backer, Tine; Rombaut, Lies; De Wandele, Inge (August 1, 2016). "Orthostatic intolerance and fatigue in the hypermobility type of Ehlers-Danlos Syndrome". Rheumatology. 55 (8): 1412–1420. doi:10.1093/rheumatology/kew032. ISSN 1462-0324.
- ↑ De Wandele, Inge; Rombaut, Lies; Leybaert, Luc; Van de Borne, Philippe; De Backer, Tine; Malfait, Fransiska; De Paepe, Anne; Calders, Patrick (August 1, 2014). "Dysautonomia and its underlying mechanisms in the hypermobility type of Ehlers–Danlos syndrome". Seminars in Arthritis and Rheumatism. 44 (1): 93–100. doi:10.1016/j.semarthrit.2013.12.006. ISSN 0049-0172.
- ↑ Gazit, Yael; Nahir, A. Menahem; Grahame, Rodney; Jacob, Giris (July 1, 2003). "Dysautonomia in the joint hypermobility syndrome". The American Journal of Medicine. 115 (1): 33–40. doi:10.1016/S0002-9343(03)00235-3. ISSN 0002-9343.
- ↑ De Wandele, Inge; Calders, Patrick; Peersman, Wim; Rimbaut, Steven; De Backer, Tine; Malfait, Fransiska; De Paepe, Anne; Rombaut, Lies (December 1, 2014). "Autonomic symptom burden in the hypermobility type of Ehlers–Danlos syndrome: A comparative study with two other EDS types, fibromyalgia, and healthy controls". Seminars in Arthritis and Rheumatism. 44 (3): 353–361. doi:10.1016/j.semarthrit.2014.05.013. ISSN 0049-0172.

