Cancer-related fatigue
Cancer-related fatigue or CRF may refer fatigue caused by cancer that begins before cancer treatment,[1] or fatigue that begins during cancer treatment, which is also known as Post-cancer Fatigue or PCF.
Cancer-related fatigue excludes the diagnosis of chronic fatigue syndrome when symptoms can be fully accounted for by cancer-related fatigue. People with pre-existing ME/CFS may experience a significant increase in fatigue after developing cancer.
Symptoms[edit | edit source]
Differences from ME/CFS[edit | edit source]
Disease process[edit | edit source]
Cancer-related fatigue and chronic fatigue syndrome have some similarities but are believed to have different underlying disease mechanisms, and affect the body differently. Fatigue can be one of several early symptoms of cancer, or may be triggered by cancer treatment.[2] Differences include different EEG findings, different hs-CRP levels and different heart rate variability.[2]
Symptoms[edit | edit source]
Post-exertional malaise (PEM) is increasingly regarded as the hallmark symptom in ME/CFS, but is only found in a minority of people with cancer-related fatigue.
Cancer-related fatigue was found to more closely linked to sleep quality, anxiety and depression compared to chronic fatigue syndrome.[2]
Diagnostic criteria[edit | edit source]
Cancer-related fatigue cannot be diagnosed without a clear test indicating that cancer is present. ME/CFS is not diagnosed if an alternative explanation is present for the symptoms, such as an untreated fatiguing illness, although this does depend on the diagnostic criteria used.
Risk factors[edit | edit source]
Triggers and risk factors differ significantly between ME/CFS and cancer-related fatigue.[3] ME/CFS is mostly commonly associated with a sudden rather than gradual onset, and often begins after an infection, particularly a virus, although many other events may trigger ME/CFS include accidents and injuries, and surgery.
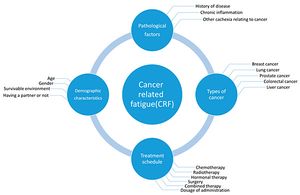
Cancer-related fatigue (CRF) is associated with different demographics, for example older patients and obesity is a significant risk factor, plus the type of cancer, the cancer treatment schedule, plus specific anti-cancer drugs and treatments.[3]
Treatment[edit | edit source]
Treatment for chronic fatigue syndrome differs significantly from the treatment of cancer-related fatigue. Exercise intolerance is a hallmark of ME/CFS and exercise therapy is linked to worsening symptoms in the vast majority of ME/CFS patients, but exercise often improves cancer-related fatigue.[2]
Notable studies[edit | edit source]
- 2022, Commonalities in the Features of Cancer and Chronic Fatigue Syndrome (CFS): Evidence for Stress-Induced Phenotype Instability?[4] - (Full text)
- 2020, Post-exertional Malaise in People With Chronic Cancer-Related Fatigue[5] - (Full text)
- A subset of people with chronic CRF (up to 33% in this sample) may experience PEM. Exercise specialists and health care professionals working with people with chronic CRF must be aware that PEM may be an issue. Symptom exacerbation after exercise should be monitored, and exercise should be tailored and adapted to limit the potential for harm.
- 2013, Differing Leukocyte Gene Expression Profiles Associated with Fatigue in Patients with Prostate Cancer versus Chronic Fatigue Syndrome[6] - (Full Text)
See also[edit | edit source]
Learn more[edit | edit source]
- Spotting the difference: Cancer related fatigue vs everyday fatigue - Leukaemia Care
References[edit | edit source]
- ↑ "Spotting the difference: Cancer related fatigue VS everyday fatigue". Leukaemia Care. Retrieved September 25, 2020.
- ↑ 2.0 2.1 2.2 2.3 Park, Hye Youn; Jeon, Hong Jun; Bang, Young Rong; Yoon, In-Young (January 2019). "Multidimensional Comparison of Cancer-Related Fatigue and Chronic Fatigue Syndrome: The Role of Psychophysiological Markers". Psychiatry Investigation. 16 (1): 71–79. doi:10.30773/pi.2018.10.26. ISSN 1738-3684. PMC 6354035. PMID 30605994.
- ↑ 3.0 3.1 Yang, Songwei; Chu, Shifeng; Gao, Yan; Ai, Qidi; Liu, Yingjiao; Li, Xun; Chen, Naihong (July 18, 2019). "A Narrative Review of Cancer-Related Fatigue (CRF) and Its Possible Pathogenesis". Cells. 8 (7): 738. doi:10.3390/cells8070738. ISSN 2073-4409. PMC 6679212. PMID 31323874.
- ↑ https://www.mdpi.com/1422-0067/23/2/691/htm
- ↑ https://doi.org/10.1016/j.jpainsymman.2020.02.012
- ↑ Light, Kathleen C.; Agarwal, Neeraj; Iacob, Eli; White, Andrea T.; Kinney, Anita Y.; VanHaitsma, Timothy A.; Aizad, Hannah; Hughen, Ronald W.; Bateman, Lucinda; Light, Alan R. (December 2013). "Differing Leukocyte Gene Expression Profiles Associated with Fatigue in Patients with Prostate Cancer versus Chronic Fatigue Syndrome". Psychoneuroendocrinology. 38 (12): 10.1016/j.psyneuen.2013.08.008. doi:10.1016/j.psyneuen.2013.08.008. ISSN 0306-4530. PMC 3848711. PMID 24054763.

