Multiple sclerosis
Multiple Sclerosis (MS) is a chronic, inflammatory, demyelinating, autoimmune disease in which the insulating covers of nerve cells in the brain and spinal cord are damaged. This damage disrupts the ability of parts of the nervous system to communicate, resulting in a range of signs and symptoms, including physical, mental, and sometimes psychiatric problems. Specific symptoms can include double vision, blindness in one eye, muscle weakness, trouble with sensation, or trouble with coordination. MS takes several forms, with new symptoms either occurring in isolated attacks (relapsing forms) or building up over time (progressive forms). Between attacks, symptoms may disappear completely; however, permanent neurological problems often remain, especially as the disease advances.[1]
Epidemiology[edit | edit source]
Prevalence[edit | edit source]
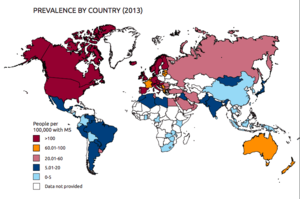
An estimated 2.3 million people worldwide have multiple sclerosis.
Risk factors[edit | edit source]
Latitude
Gender differences[edit | edit source]
Over the last decades, the ratio of women to men with MS has increased markedly, representing a true increase in MS among women but not men.[2]
Disease mechanisms[edit | edit source]
Immune system[edit | edit source]
In 1997, it was discovered that B cell therapy (eg Rituximab) which reduces the number of B cells, can bring immediate improvement in MS symptoms. This treatment is more effective for the relapsing-remitting variant of MS, and less effective for the primary progressive variant.[3]
Microbiome[edit | edit source]
Specific changes in the gut microbiome might increase the risk of MS[4], and the risk might be reduced using probiotics, antibiotics, a combination, or a change of diet. An 'International Multiple Sclerosis Microbiome Study' commenced in 2015.[3]
Treatments[edit | edit source]
Standard of care[edit | edit source]
Experimental treatments[edit | edit source]
Another discovery was that a commonly available and inexpensive antihistamine, can be used to induce remyelination of the nerve cells.[3]
Dietary tryptophan can help reduce brain inflammation and 'cognitive fog'.[5]
Comparison of Multiple Sclerosis and ME/CFS[edit | edit source]
Multiple Sclerosis is often used as a control group in ME/CFS research.[6]
There are many similar features in Multiple Sclerosis and Chronic Fatigue Syndrome/Myalgic Encephalomyelitis, including: severe disabling fatigue that worsens after exercise; debilitating autonomic symptoms, including orthostatic intolerance; illness course may be relapsing-remitting or progressive; infections and psychosocial stress causing exacerbation; auto-immunity and auto-inflammatory processes; mitochondrial dysfunction; and decreased cerebral blood flow, atrophy of some brain structures.[7]
In the United States, the prevalence rate of CFS is 0.42% of the population versus MS which has a rate of 0.09%.[8] Approximately 14% of MS patients meet the Fukuda criteria for CFS.[9]
In 2017, a study examined whether network analysis of cytokine production differed between patients with CFS, multiple sclerosis, and healthy controls. The study's model, using a select cytokine profile, showed that immunologic activation in CFS was significantly different from that found in the control and multiple sclerosis groups.[10]
A 2015 study found a markedly disturbed immune signature in the cerebrospinal fluid that is consistent with immune activation in the central nervous system, and autoimmunity. The MS and ME/CFS groups had markedly different immune signatures, and the ME/CFS group had a greater degree of CNS immune activation than the MS group.[11]
In December 2016, Ohanian, et al, published a study identifying two key immune symptoms that physicians could use to differentiate Myalgic Encephalomyelitis and Chronic Fatigue Syndrome from Multiple Sclerosis: flu-like symptoms and tender lymph nodes. Subjects included 106 people with MS and 354 people with ME or CFS who completed the DePaul Symptom Questionnaire. The data was analyzed using data mining techniques and machine learning that resulted in correctly categorizing MS and ME or CFS 81.2% of the time. The authors conclude that "because ME or CFS and MS have similar presentations recognizing the importance of immune dysfunction for ME or CFS might be important for healthcare providers."[12]
Notable studies comparing ME/CFS and multiple sclerosis[edit | edit source]
- 2018, Functional Status and Well-Being in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Compared with People with Multiple Sclerosis and Healthy Controls[13] (Full Text)
- 2017, Differentiating Multiple Sclerosis from Myalgic Encephalomyelitis and Chronic Fatigue Syndrome[14] (Full Text)
- 2017, Dysregulation of cytokine pathways in chronic fatigue syndrome and multiple sclerosis[10] (Abstract)
- 2017, Endogenous Pain Facilitation Rather Than Inhibition Differs Between People with Chronic Fatigue Syndrome, Multiple Sclerosis, and Controls: An Observational Study[15] (Full Text)
- 2016, Identifying Key Symptoms Differentiating Myalgic Encephalomyelitis and Chronic Fatigue Syndrome from Multiple Sclerosis[12] (Full Text)
- 2016, Pilot Study of Natural Killer Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis[16] (Abstract)
- 2016, Regulatory T, natural killer T and γδ T cells in multiple sclerosis and chronic fatigue syndrome/myalgic encephalomyelitis: a comparison[17] (Full Text)
- 2016, Cytokine network analysis of cerebrospinal fluid in myalgic encephalomyelitis/chronic fatigue syndrome[11] (Abstract)
- 2015, A Preliminary Comparative Assessment of the Role of CD8+ T Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis[18] (Full Text)
- 2015, A Comparison of Cytokine Profiles of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis Patients[19] (Full Text)
- 2013, Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics[7] (Full Text)
- 2012, Differences in metabolite-detecting, adrenergic, and immune gene expression after moderate exercise in patients with chronic fatigue syndrome, patients with multiple sclerosis, and healthy controls.[20] (Full Text)
Learn more[edit | edit source]
See also[edit | edit source]
References[edit | edit source]
- ↑ "Multiple Sclerosis", Wikipedia
- ↑ Harbo, Hanne (July 2013). "Sex and gender issues in multiple sclerosis". Ther Adv Neurol Disord.
- ↑ 3.0 3.1 3.2 Conway, Claire (April 25, 2016), "Wrapping Up Multiple Sclerosis", UCFS News Center
- ↑ "Gut bacteria regulate nerve fibre insulation", The Guardian - Science, April 5, 2016
- ↑ Rothhammer, Veit; Mascanfroni, Ivan D; Bunse, Lukas; et al. (May 9, 2016), "Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor", Nature Medicine, advance online publication, doi:10.1038/nm.4106, ISSN 1078-8956, lay summary
- ↑ reference needed
- ↑ 7.0 7.1 Morris, Gerwyn; Maes, Michael (2013), "Myalgic encephalomyelitis/chronic fatigue syndrome and encephalomyelitis disseminata/multiple sclerosis show remarkable levels of similarity in phenomenology and neuroimmune characteristics", BMC Medicine, 11: 205, doi:10.1186/1741-7015-11-205, ISSN 1741-7015
- ↑ Jason LA, Paavola E, Porter N, Morello M (2010) Frequency and content analysis of CFS in medical textbooks. Aust J Prim Health 16:174-178.
- ↑ Gaber TAZK, Oo WW, Ringrose H (2014) Multiple sclerosis/chronic fatigue syndrome overlap: When two common disorders collide. Neuro Rehabil 35: 529–534.
- ↑ 10.0 10.1 Sorenson, Matthew; Furst, Jacob; Mathews, Herbert; Jason, Leonard A. (2017), "Dysregulation of cytokine pathways in chronic fatigue syndrome and multiple sclerosis", Fatigue: Biomedicine, Health & Behavior, 5 (3): 145-158, doi:10.1080/21641846.2017.1335237
- ↑ 11.0 11.1 Hornig, M; Gottschalk, CG; Peterson, DL; et al. (February 2016), "Cytokine network analysis of cerebrospinal fluid in myalgic encephalomyelitis/chronic fatigue syndrome", Molecular Psychiatry, 21 (2): 261–269, doi:10.1038/mp.2015.29, ISSN 1359-4184, lay summary
- ↑ 12.0 12.1 Ohanian, Diana; Brown, Abigail; Sunnquist, Madison; Furst, Jacob; Nicholson, Laura; Klebek, Lauren; Jason, Leonard (2016), "Identifying Key Symptoms Differentiating Myalgic Encephalomyelitis and Chronic Fatigue Syndrome from Multiple Sclerosis", EC Neurology, 4.1 (2): 41-45, PMID 28066845
- ↑ Kingdon, CC; Bowman, EW; Curran, H; Nacul, L; Lacerda, EM (2018), "Functional Status and Well-Being in People with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Compared with People with Multiple Sclerosis and Healthy Controls", PharmacoEconomics - Open, doi:10.1007/s41669-018-0071-6, PMID 29536371
- ↑ Jason, LA; Ohanian, D; Brown, A; Sunnquist, M; McManimen, S; Klebek, L; Fox, P; Sorenson, M (2017), "Differentiating Multiple Sclerosis from Myalgic Encephalomyelitis and Chronic Fatigue Syndrome", Insights in Biomedicine, 2 (2), doi:10.21767/2572-5610.100011
- ↑ Polli, Andrea; Willekens, Barbara; Meeus, Mira; Nijs, Jo; Collin, Simon M.; Ickmans, Kelly (2017), "Endogenous Pain Facilitation Rather Than Inhibition Differs Between People with Chronic Fatigue Syndrome, Multiple Sclerosis, and Controls: An Observational Study Observational Study", Pain Physician, 20 (4): E489-E497, PMID 28535557
- ↑ Huth, TK; Brenu, EW; Ramos, S; Nguyen, T; Broadley, S; Staines, D; Marshall-Gradisnik, S (January 2016), "Pilot Study of Natural Killer Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis", Scand J Immunol, 83(1): 44-51, doi:10.1111/sji.12388, PMID 26381393
- ↑ Ramos, S; Brenu, E; Broadley, S; Kwiatek, R; Ng, J; Nguyen, T; Freeman, S; Staines, D; Marshall-Gradisnik, S (March 20, 2016), "Regulatory T, natural killer T and γδ T cells in multiple sclerosis and chronic fatigue syndrome/myalgic encephalomyelitis: a comparison" (PDF), Asian Pac J Allergy Immunol, 2016 (34): 300-305, doi:10.12932/AP0733
- ↑ Brenu, EW; Broadley, S; Nguyen, T; Johnston, S; Ramos, S; Staines, D; Marshall-Gradisnik, S (2016), "A Preliminary Comparative Assessment of the Role of CD8+ T Cells in Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis" (PDF), Journal of Immunology Research, 2016, doi:10.1155/2016/9064529
- ↑ Wong, Naomi; Nguyen, Thao; Brenu, Ekua Weba; Broadley, Simon; Staines, Donald; Marshall-Gradisnik, Sonya (2015), "A Comparison of Cytokine Profiles of Chronic Fatigue Syndrome/Myalgic Encephalomyelitis and Multiple Sclerosis Patients", International Journal of Clinical Medicine, 6 (10): 769-783, doi:10.4236/ijcm.2015.610103
- ↑ White, AT; Light, AR; Hughen, RW; Vanhaitsma, TA; Light, KC (2012), "Differences in metabolite-detecting, adrenergic, and immune gene expression after moderate exercise in patients with chronic fatigue syndrome, patients with multiple sclerosis, and healthy controls", Psychosomatic Medicine, 74 (1): 46-54, doi:10.1097/PSY.0b013e31824152ed