Thyroid hormone
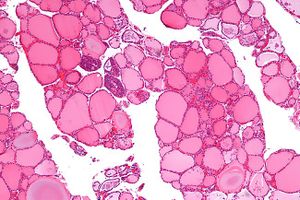
Source: Mizukami et al. (1994). "Solid cell nests of the thyroid. A histologic and immunohistochemical study". American Journal of Clinical Pathology. 101 (2): 186–191. doi:10.1093/ajcp/101.2.186.[1], enlarged and cropped.
Thyroid hormones are a group of hormones produced and released by the thyroid gland, namely triiodothyronine (T3) and thyroxine (T4). They are primarily responsible for regulation of metabolism, and thus act on nearly every cell in the body.
Thyroid hormone production is regulated by the pituitary gland, which releases thyroid stimulating hormone (TSH).
Over production of thyroid hormones (hyperthyroidism) can accelerate your body's metabolism causing sudden weight loss, a rapid or irregular heartbeat, sweating, nervousness or irritability, and other symptoms.[2] Under production of thyroid hormones (hypothyroidism) can lower your body's metabolism causing obesity, fatigue, muscle weakness, thinning hair, slowed heart rate, depression and other symptoms.[2]
Types of thyroid hormones[edit | edit source]
Thyroxine (T4) (90%)[edit | edit source]
Thyroxine (abbreviated as T4) accounts for 90% of the hormone produced by the thyroid gland. It is physiological inactive and must be converted to T3 in the liver and kidneys.
Triiodothyronine (T3) (9%)[edit | edit source]
Triiodothyronine (abbreviated as T3) is the active form of the hormone. Only 9% of the thyroid hormone produced by the thyroid glad is T3. The rest of the physiologically required T3 is converted from T4 within liver and kidney cells by deiodinases, which are selenium-dependent enzymes. Selenium sufficiency is therefore important for the proper conversion of T4 to T3. Genetic differences can deiodinase production and therefore conversion ability.
Reverse T3 (rT3) (0.9%)[edit | edit source]
Reverse T3 is an isomer of T3, that is it has the same chemical formula but a different shape and is physiologically inactive. It is also made from T4 and plays a role in euthyroid sick syndrome, where rT3 levels are elevated in presence of normal T4 and TSH levels.
Diiodothyronine (T2)[edit | edit source]
The physiological functions of diiodothyronine (T2), including 3,5-diiodo-L-thyronine, are less well-understood.
Production[edit | edit source]
Central[edit | edit source]
Peripheral[edit | edit source]
T4 is a prohormone and a reservoir for the biologically active T3. T4 is converted to T3 by deiodinase enzymes.
There are three types of deiodinase enzymes:
- Type 1 (D1) deiodinates T4 to the biologically active T3 as well as the hormonally inactive and possibly inhibitory rT3. Breaks down rT3 into T2. Encoded by DIO1 gene. In humans, it is found in liver, kidney, thyroid, and pituitary.[3]
- Type 2 (D2) converts T4 into T3, and breaks down rT3 into T2. Encoded by DIO2 gene. In humans, it is found in skeletal muscle, central nervous system, pituitary, thyroid, heart, and brown adipose tissue.[3]
- Type 3 (D3) produces rT3 from T4, and breaks down T3 into T2. Encoded by DIO3 gene. In humans, it has been found in the central nervous system and placenta in adults and in many additional tissues in the fetus.[3]
Genetic factors[edit | edit source]
It is estimated that 40–65% of the inter-individual variation in serum TSH and FT4 levels is determined by genetic factors.[3] Genetic factors may influence individual variation in the ability to convert T4 to T3. Several SNPs of the DIO1 gene, which encodes for the D1 enzyme, and DIO2 gene, which encodes for the D2 enzyme, have been studied.
D1O1[edit | edit source]
rs2235544: The homozygous mutant allele (A;A) is associated decreased deiodinase function, resulting in a lower FT3/FT4 ratio, lower T3 and high T4 compared to wild type.[3][4]
D2O2[edit | edit source]
rs225014: Also known as Thr92Ala, represents a variant in the deiodinase, iodothyronine, type II DIO2 gene on chromosome 14. A study of 102 patients pre- and post- total thyroidectomy showed that after receiving T4-only hormone replacement, 34% of patients had lower reduced Free T3 levels (FT3) than they had pre-surgery. Those with mutant alleles of Thr92Ala had lower levels of Free T3 hormone than wild type (Thr/Thr) / (T;T) patients. The percentage of reduced post-surgery FT3 levels was directly correlated with the presence and severity of the polymorphism: 58.3% in homozygous (Ala/Ala) / (C;C) patients vs 36.5% in heterozygous (Thr/Ala) / (T;C) subjects.[5]
rs12885300: In a study of patients after thyroidectomy, patients with appeared to have an "have an altered set point of the hypothalamus-pituitary-thyroid axis" with a weaker negative feedback of FT4 on TSH in patients with homozygous mutant alleles (C;C).[6]
Transport[edit | edit source]
Thyroxine binding globulin is a transport protein responsible for carrying T4 and T3 in the bloodstream.
Function and metabolic effects[edit | edit source]
Thyroid hormones are essential for regulating a number of biological processes, including growth, neurodevelopment, carbohydrate metabolism, oxygen consumption and protein synthesis.
Mitochondrial function[edit | edit source]
T3 plays an important role in the regulation of mitochondrial function as well as in mitochondrial biogenesis[7]. T3 rapidly stimulates an increase in cellular respiration within minutes to hours after hormone treatment. One to several days after hormone treatment, changes in gene expression as well as direct binding of hormone to receptors induces mitochondrial biogenesis and changes to mitochondrial mass. T3 stimulates the expression of an inner membrane mitochondrial protein called uncoupling protein, resulting in increased inner membrane proton leak. It also induces changes in phospholipid turnover. ATP synthesis and turnover reactions are also affected.[8][9][10]
Uncoupling protein is responsible for thermogenesis, which is why hyperthyroidism results in excess heat while hypothyroidism results in cold intolerance.
Citric acid cycle[edit | edit source]
T3 increases oxygen[11][12][13], glucose and pyruvate[14][15][16] utilization, shifting metabolism from an anaerobic to more aerobic state.
T2 also plays a role in regulating energy metabolism, although its role is less studied. 3,5-diiodo-L-thyronine influences resting metabolic rate.[17]
Cholesterol[edit | edit source]
Triiodothyronine reduces cholesterol.
Testing[edit | edit source]
Standard commercial laboratory testing for thyroid hormones is via immunoassay. However, these tests are shown to be unreliable in the low-normal and high-normal range when compared to mass spectrometry.[18] In addition, most clinicians do not test for reverse T3.
Thyroid disease[edit | edit source]
Hypothyrodism[edit | edit source]
Hypothyrodism is when the thyroid produces excess levels of hormone. It can have a number of causes including:
Hyperthyrodism[edit | edit source]
Hyperthyroidism is when the thyroid produces excess levels of hormone. It can have a number of causes including:
- Graves' disease, an autoimmune disorder
Low T3 Syndrome[edit | edit source]
Also known as euthyroid sick syndrome, Low T3 syndrome is characterized by decreased serum T3 and/or thyroxin (T4) levels, increased reverse T3 (rT3), and no significant increase in TSH. Low T3 syndrome is often seen in cases of acute and chronic illness, including myocardial infarction, fasting, starvation and sepsis. There is no evidence that supplementation with T3 is of benefit.
Nutrition[edit | edit source]
Iodine, selenium and iron are crucial for normal thyroid hormone function. Thyroid hormones are partially comprised of iodine and a deficiency of iodine in the diet can lead to decreased production of these hormones. If left uncorrected the thyroid tissue can enlarge, resulting in a pronounced swelling in the neck, called a 'simple goitre.'[19][20] Selenium is required for the production of deiodinase enzymes, and thus the conversion of T4 to T3. Iron is needed for heme-dependent thyroid peroxidase.
Hormone replacement[edit | edit source]
Patients with hypothyroidism may need hormone replacement. The standard replacement therapy is Levothyroxine, a synthetic form of T4. However, some patients on Levothyroxine report continuing symptoms of hypothyroidism despite normal laboratory results, perhaps owing to poor conversion of T4 to T3. In these cases, patients may add a T3 replacement hormone drug such as Liothyronine sodium with brand names Cytomel (US, Canada) or Cynomel (Mexico), or a natural desiccated thyroid product such as Armour Thyroid (US), Erfa Thyroid (Canada), or Thyroid-S (Thailand), which is made from the thyroid gland of pigs.
Role in other human disease[edit | edit source]
ME/CFS[edit | edit source]
A study of 99 patients with a diagnosis of chronic fatigue syndrome found similar levels of TSH to healthy controls but lower free triiodothyronine (FT3), total thyroxine (TT4), total triiodothyronine (TT3), %TT3 (4.7%), deiodinase activity, secretory capacity of the thyroid gland, lower 24-h urinary iodine (27.6%), and higher % reverse T3 (rT3). "Low circulating T3 and the apparent shift from T3 to rT3 may reflect more severely depressed tissue T3 levels. The present findings might be in line with recent metabolomic studies pointing at a hypometabolic state."[21]
Fibromyalgia[edit | edit source]
A series of small N trials found significant improvement in fibromyalgia symptoms in euthyroid patients given T3.[22][23][24][25]
Small intestinal bacterial overgrowth[edit | edit source]
In one study, 54% of patients with hypothyroidism tested positive for small intestinal bacterial overgrowth (SIBO) as compared to 5% of controls.[26] SIBO is also associated with Levothyroxine usage,[27] possibly owing to the secondary hypothyroidism seen in patients who are poor converters.
Notable studies[edit | edit source]
- 2018, Higher Prevalence of “Low T3 Syndrome” in Patients With Chronic Fatigue Syndrome: A Case–Control Study[21] Full Text)
Learn more[edit | edit source]
See also[edit | edit source]
References[edit | edit source]
- ↑ Mizukami, Y.; Nonomura, A.; Michigishi, T.; Noguchi, M.; Hashimoto, T.; Nakamura, S.; Ishizaki, T. (February 1994). "Solid cell nests of the thyroid. A histologic and immunohistochemical study". American Journal of Clinical Pathology. 101 (2): 186–191. doi:10.1093/ajcp/101.2.186. ISSN 0002-9173. PMID 7509563.
- ↑ 2.0 2.1 "Hyperthyroidism - Symptoms and causes". Mayo Clinic. Retrieved July 31, 2018.
- ↑ 3.0 3.1 3.2 3.3 3.4 Medici, Marco (March 2017). "Genetics of thyroid function". Best Practice & Research Clinical Endocrinology & Metabolism. 31: 129–142.
- ↑ Panicker, V (August 2008). "A common variation in deiodinase 1 gene DIO1 is associated with the relative levels of free thyroxine and triiodothyronine". Journal of Clinical Endocrinology Metabolism. 93: 3075–81.
- ↑ Castagna, Maria (May 2017). "DIO2 Thr92Ala Reduces Deiodinase-2 Activity and Serum-T3 Levels in Thyroid-Deficient Patients". The Journal of Clinical Endocrinology & Metabolism. 102: 1623–1630.
- ↑ Hoftijzer, HC (September 2011). "The type 2 deiodinase ORFa-Gly3Asp polymorphism (rs12885300) influences the set point of the hypothalamus-pituitary-thyroid axis in patients treated for differentiated thyroid carcinoma". Journal of Clinical Endocrinology and Metabolism. 96: 1527–33.
- ↑ Weitzel, Joachim (May 4, 2004). "Regulation of Mitochondrial Biogenesis by Thyroid Hormone". Experimental Physiology.
- ↑ Harper, ME; Seifert, EL (February 2008). "Thyroid hormone effects on mitochondrial energetics". Thyroid.
- ↑ Wrutniak-Cabello, C (February 2001). "Thyroid Hormone action in mitochondria". Journal of Molecular Endocrinology.
- ↑ Cioffi, Frederica (October 15, 2013). "Thyroid hormones and mitochondria: With a brief look at derivatives and analogues". Molecular and Cellular Endocrinology. 379: 51–61.
- ↑ Bray, G.A. (August 1, 1969). "Effect of diet and triiodothyronine on the activity of sn-glycerol-3-phosphate dehydrogenase and on the metabolism of glucose and pyruvate by adipose tissue of obese patients". The Journal of Clinical Investigation.
- ↑ Bray, G.A. (August 1971). "Effects of Triiodothyronine, Growth Hormone and Anabolic Steroids on Nitrogen Excretion and Oxygen Consumption of Obese Patients". The Journal of Clinical Endocrinology & Metabolism. 33: 293–300.
- ↑ Oh, Soomee (December 1, 1994). "Early Treatment of Obese (ob/ob) Mice with Triiodothyronine Increases Oxygen Consumption and Temperature and Decreases Body Fat Content". Experimental Biology and Medicine. 207: 260–267.
- ↑ Paradise, Giuseppe (August 17, 1988). "Effect of hyperthyroidism on the transport of pyruvate in rat-heart mitochondria". Biochimica et Biophysica Acta (BBA) - Bioenergetics. 935: 79–86.
- ↑ Leary, DC (October 1996). "Direct Effects of 3, 5, 3′-Triiodothyronine and 3, 5-Diiodothyronine on Mitochondrial Metabolism in the GoldfishCarassius auratus". General and Comparative Endocrinology.
- ↑ Novitsky, D (January 1988). "Change from aerobic to anaerobic metabolism after brain death, and reversal following triiodothyronine therapy". Transplantation. 45: 32–36.
- ↑ Goglia, Fernando (June 1999). "Action of thyroid hormones at the cellular level: the mitochondrial target". FEBS Letters. 452: 115–120.
- ↑ "Steve Soldin & NIH team develop UltraHigh Sensitivity Method for FT3/FT4 Hormones with IONICS 3Q 320". January 9, 2015.
- ↑ "Thyroid Goiter". UCLA Health. Retrieved October 31, 2020.
- ↑ "Simple goiter". MedlinePlus Medical Encyclopedia. Retrieved October 31, 2020.
- ↑ 21.0 21.1 Ruiz-Núñez, Begoña; Tarasse, Rabab; Vogelaar, Emar F.; Janneke Dijck-Brouwer, D.A.; Muskiet, Frits A. J. (2018), "Higher Prevalence of "Low T3 Syndrome" in Patients With Chronic Fatigue Syndrome: A Case–Control Study", Frontiers in Endocrinology, 9: 97, doi:10.3389/fendo.2018.00097, PMID 29615976
- ↑ Lowe, John C. (August 10, 1996). "Results of an Open Trial of T3Therapy with 77 Euthyroid Female Fibromyalgia Patients". Clinical Bulletin of Myofascial Therapy. 2 (1): 35–37. doi:10.1300/j425v02n01_04. ISSN 1089-4195.
- ↑ Lowe, John C.; Garrison, Richard L.; Reichman, Alan; Yellin, Jackie (August 15, 1997). "Triiodothyronine (T3) Treatment of Euthyroid Fibromyalgia". Clinical Bulletin of Myofascial Therapy. 2 (4): 71–88. doi:10.1300/j425v02n04_05. ISSN 1089-4195.
- ↑ Lowe, John C.; Garrison, Richard L.; Reichman, Alan J.; Yellin, Jackie; Thompson, Mervianna; Kaufman, Daniel (October 8, 1996). "Effectiveness and Safety of T3(Triiodothyronine) Therapy for Euthyroid Fibromyalgia". Clinical Bulletin of Myofascial Therapy. 2 (2–3): 31–57. doi:10.1300/j425v02n02_04. ISSN 1089-4195.
- ↑ Lowe, Jhon C.; Reichman, Alan J.; Yellin, Jackie (October 8, 1996). "The Process of Change During T3Treatment for Euthyroid Fibromyalgia". Clinical Bulletin of Myofascial Therapy. 2 (2–3): 91–124. doi:10.1300/j425v02n02_07. ISSN 1089-4195.
- ↑ Lauritano, Ernesto Cristiano (November 1, 2007). "Association between Hypothyroidism and Small Intestinal Bacterial Overgrowth". The Journal of Clinical Endocrinology & Metabolism. 92: 4180–4184.
- ↑ Brechmann, Thorsten (February 2017). "Levothyroxine therapy and impaired clearance are the strongest contributors to small intestinal bacterial overgrowth: Results of a retrospective cohort study". World Journal of Gastroenterology. 23: 842–852.

