Epstein-Barr virus
The Epstein-Barr virus or EBV or Human Herpesvirus 4 or HHV-4 is a herpesvirus.[1] It is the most common cause of infectious mononucleosis or "glandular fever," and infects 90% of adults worldwide.[2] It has been implicated in numerous immune diseases and chronic illnesses, including chronic fatigue syndrome, multiple sclerosis, myasthenia gravis, and systemic lupus erythematosus. It is known to turn on "risk genes" for autoimmune disease in the cells it infects.[3][4]
Initial infection[edit | edit source]
Symptoms of EBV infection include:
Age of infection[edit | edit source]
Most people acquire EBV before the age of ten. Typically, young children who acquire EBV are either not symptomatic or have mild symptoms that are hard to distinguish from a cold or other other mild, childhood illnesses.[5]
In adolescents and young adults, EBV can cause infectious mononucleosis (IM), also known as glandular fever.[1] IM is characterized by fever, sore throat, swollen lymph nodes, body aches, and fatigue. It generally resolves with rest and only rarely causes serious complications. It typically occurs in people who have not been exposed to EBV in early childhood, and in comparison, is more severe than infection in childhood (i.e., it can last for months).
Following initial infection, EBV can reactivate and has been shown to have many connections with various chronic illnesses. Relative to initial infections, reactivated EBV is much more severe.
Transmission[edit | edit source]
EBV is transmitted through bodily fluids, most commonly through saliva. The first time a person is infected with EBV, the person is contagious for weeks (even when not displaying symptoms). The virus then transitions to the latent or inactive form, and stays in the body. If the virus reactivates, the person will be contagious again.[1]
Diagnosis[edit | edit source]
EBV infection is confirmed with blood tests that detect presence of antibodies. Nine out of ten adults have these antibodies, indicating that they have a current or past EBV infection.[1]
Anti-VCA (Viral capsid antigen) IgG and EBV nuclear antigen (EBNA) IgG antibodies persist throughout a person's life. Thus, positive results merely indicate a current or past infection. A current EBV infection is diagnosed based on the presence of Anti-VCA IgM and Anti-EA (Early Antigen) IgG. VCA IgM appears early in EBV infection and usually disappears within four to six weeks. Positive VCA IgM suggests current active acute EBV infection. EA IgG appears in the acute phase of illness and generally falls to undetectable levels after three to six months. Positive EA IgG can suggest current active EBV infection or EBV re-activation. [6]
Latency[edit | edit source]
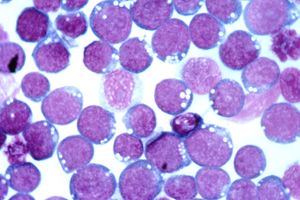
In healthy adults, the virus remains latent for life in memory B cells. It is estimated that one in every one hundred thousand to one million circulating B cells carry EBV.[7] In healthy hosts, EBV populations are kept in check by CD4+ and CD8+ T-cell responses.
The equilibrium can be disrupted in individuals with compromised immune systems such as patients with AIDS or transplant patients taking immune system suppressing drugs.[8] It has been observed that these patients are more susceptible to EBV-related cancers, such as certain lymphomas and carcinomas.[9] In immunocompromised patients, EBV can induce lymphoproliferation, lymphoma, and hemophagocytic lymphohistiocytosis (HLH).[10]
Natural killer T cells[edit | edit source]
It is thought that natural killer T cells (NKT) play a pivotal role in the control of EBV-infected B cells through their recognition of CD1d expressing cells.[8]
Neuronal infection[edit | edit source]
A 2015 study[11] demonstrated that human neuronal cells could be directly and actively infected with EBV and another herpesvirus, Kaposi's sarcoma-associated herpesvirus (KSHV).
Neuronal cells were infected with EBV or KSHV viruses which had been combined with a fluorescent protein so that the infection could be observed. The infection was seen to produce new virus cells (productive) and spread efficiently. Significantly, it not only infected surrounding neuronal cells but also nearby peripheral blood mononuclear cells.
EBV is known to be linked to many neuronal diseases[12] but this is the first evidence of how this may occur. The researchers note that this research supports the presence of EBV in neuronal diseases, but does not indicate why this is so.
In human disease[edit | edit source]
Epstein-Barr virus has been associated with a wide number of immune diseases including multiple sclerosis, rheumatoid arthritis, systemic lupus erythematosus,[13] chronic fatigue syndrome, and myasthenia gravis. EBV was recently discovered to turn on "risk genes" for autoimmune disease in the cells it infects. EBNA2, a protein produced by EBV-infected cells, and its related transcription factors activate half the human genes known to be associated with the risk for lupus as well as genes associated with several other autoimmune diseases including multiple sclerosis, rheumatoid arthritis, inflammatory bowel disease, type 1 diabetes, juvenile idiopathic arthritis and celiac disease. EBV activation can thus increase the risk of developing these diseases.[3][4]
Chronic fatigue syndrome[edit | edit source]
A prospective study of 250 primary care patients revealed a higher prevalence of chronic fatigue syndrome after infectious mononucleosis (glandular fever) when compared to an ordinary upper respiratory tract infection.[14] Anti-early antigen titers to EBV were elevated in CFS patients and associated with worse symptoms.[15] A 2006 Australian prospective study found that 12% of subjects infected by EBV met the criteria for chronic fatigue syndrome six months after their infection, and 9% still had CFS 12 months after infection.[16] (The same rate held true for Ross River virus and Q fever.) In another study sample, 110 of 178 patients with increased antibodies against EBV had a diagnosis of CFS.[17]
Long COVID[edit | edit source]
Long COVID may be associated herpesvirus reactivation such as EBV.[18][19]
Multiple sclerosis[edit | edit source]
Infection later in life, high serum titers against EBV, and mononucleosis have all been associated with an increased risk of multiple sclerosis. MS relapses are correlated with EBV reactivation.[20]
Several studies by Alberto Ascherio, MD, DrPH, and his team at the Harvard School of Public Health have suggested that EBV is involved in multiple sclerosis, specifically in people with a certain immune-related gene and high levels of antibodies to EBV in their blood.[21]
Systemic lupus erythematosus[edit | edit source]
In a study of young patients with lupus, 99% had EBV as compared to 70% of healthy controls.[22] Another study found that patients with systemic lupus erythematosus had a roughly 40-fold increase in EBV viral loads compared with controls, likely stemming from altered t cell responses against EBV.[23]
Myasthenia gravis[edit | edit source]
Myasthenia gravis is an autoimmune disease which has been associated with a large number of different viruses, particularly EBV, HPV, and polioviruses. In several studies EBV infection of the thymus has been found in myasthenia gravis patients, but not all studies have found this.[24] B cells from myasthenia gravis patients stimulated in vitro by Epstein-Barr virus produced acetylcholine autoantibodies.[25] While EBV infection of the thymus has been posited as a causative agent for the production of acetylcholine receptor autoantibodies in myasthenia gravis.[26], there is only limited evidence supporting EBV or other viruses as a cause of myasthenia gravis.[24]
Gastrointestinal disease[edit | edit source]
One study of EBV in patients with gastritis, Crohn's disease, and ulcerative colitis and normal controls found essentially undetectable levels of EBV in normal gastric mucosa. However, EBV was detected in 46% of gastritis lesions, 44% of normal colonic mucosa, 55% of Crohn’s disease, and 64% of ulcerative colitis samples.[27]
Lyme disease[edit | edit source]
Several herpesviruses including Epstein-Barr virus may cause false positives on Lyme disease tests.[28]
XMEN disease[edit | edit source]
A 2014 study found chronic Epstein-Barr infection was linked to a magnesium transporter MAGT mutation.[29] Dysfunction in this transporter also resulted in decreased NK cell function, and neoplasia (sometimes-cancerous growths).[30]
This disorder, termed "XMEN" (for X-linked, EBV, and neoplasia) was identified as a recessive, X-linked disorder that would therefore be many times more common in men.
Since chronic EBV infection has been associated with chronic fatigue syndrome, this error in magnesium transport may be worth considering in male patients, especially with slow onset and history of childhood infection.[30][31] However, in this disorder, EBV would be seen as an indicator of the illness rather than the cause.
Vitamin D[edit | edit source]
Some recent research is finding links between EBV and Vitamin D.
An EBV protein, EBNA-3, has an affinity for the vitamin D receptor (VDR) and may actually block the activation of VDR-dependent genes by Vitamin D.[32]
Vitamin D receptor may be required for the normal development of natural killer T cells that react to cells expressing CD1d, as in cells infected by EBV.[33] VDR is expressed on B cells infected with EBV, and bioactive Vitamin D3 alters T cells to be less detrimental to the immune response.[20]
As low Vitamin D is also a risk factor for MS, some studies have attempt to find a link between low Vitamin D status, EBV, and MS. One study of healthy individuals found no link between EBV load and Vitamin D status. However, over half the subjects were Vitamin D deficient and none had optimal levels[34] (i.e., above 100 nmol/l).
Treatment[edit | edit source]
There is no specific treatment for EBV, only treatment of symptoms, such as taking over-the-counter medications for pain and fever.[1] EBV is thought to persistent harmlessly in immunocompetent individuals, but in those with compromised immune systems it has been associated with certain cancers and possibly autoimmune disease.
Antivirals[edit | edit source]
Several antivirals are active against EBV including valganciclovir, valacyclovir[35], acyclovir[36], and spironolactone.[37]
Acyclovir, an antiviral drug which inhibits (but does not destroy) herpesviruses, was shown to also inhibit the virus production. This suggests that EBV replicates via lytic replication.
A theoretical immunotherapy treatment proposes that inducing CD1d expression on EBV-infected B cells could prompt effective immune suppression of EBV by natural killer T cells.[8]
Rituximab[edit | edit source]
Rituximab may be effective in completely eliminating EBV infection from the peripheral blood.[38] A study of seventeen patients with low-grade B cell lymphoma found that after three cycles of rituximab, the virus had been completely eliminated from the peripheral blood in all but one patient.
Herbs and nutraceuticals[edit | edit source]
Though not tested in clinical trials, licorice derivatives quercetin and isoliquiritigenin inhibit EBV in cell cultures.[39] Vitamin C[17] and Vitamin D3[40] might also decrease duration and severity of the symptoms of EBV infection.
Vaccine[edit | edit source]
A vaccine for the prevention of Epstein-Barr virus is being explored.[41]
Notable studies[edit | edit source]
- 1996, MMPI profiles of patients with chronic fatigue syndrome[15] - (Abstract)
- 1998, Incidence, risk and prognosis of acute and chronic fatigue syndromes and psychiatric disorders after glandular fever[14] - (Abstract)
- 2006, Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study[16] - (Full text)
- 2019, EBV-requisitioning physicians' guess on fatigue state 6 months after acute EBV infection[42] - (Abstract)
- 2019, Predictors of chronic fatigue in adolescents six months after acute Epstein-Barr virus infection: A prospective cohort study[43] - (Abstract)
- 2019, Lifestyle factors during acute Epstein-Barr virus infection in adolescents predict physical activity six months later[44] - (Abstract)
- 2019, Epstein-Barr Virus dUTPase Induces Neuroinflammatory Mediators: Implications for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[45] - (Full text)
- 2019, Review article - Epstein-Barr virus induced gene-2 upregulation identifies a particular subtype of Chronic Fatigue Syndrome / Myalgic Encephalomyelitis[46] - (Full text)
- 2019, Epstein-Barr virus (EBV) reactivation and therapeutic inhibitors[47] - (Abstract)
- 2020, Cytomegalovirus, Epstein-Barr Virus, and Human herpesvirus-6 Infections in Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome[48] - (Abstract)
- 2021, Epstein-Barr Virus and the Origin of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome[49] - (Full text)
- 2021, Lasting Immunological Imprint of Primary Epstein-Barr Virus Infection With Associations to Chronic Low-Grade Inflammation and Fatigue[50] - (Full text)
- 2021, Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation[19] (Full text)
- 2021, Risks for Developing Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in College Students Following Infectious Mononucleosis: A Prospective Cohort Study[51] - (Full text)
- 2022, EBV/HHV-6A dUTPases contribute to myalgic encephalomyelitis/chronic fatigue syndrome pathophysiology by enhancing TFH cell differentiation and extrafollicular activities[52] - (Full text)
See also[edit | edit source]
- List of herpesvirus infection studies
- Abortive infection theory of ME/CFS (Dr. Lerner's theory that abortive herpesviruses cause ME/CFS)
Learn more[edit | edit source]
- Antiviral agents for infectious mononucleosis (glandular fever) (2016) - Cochrane review
- Study Provides Strongest Evidence Yet for the Role of Epstein-Barr Virus in Triggering Multiple Sclerosis (2022) - Multiple Sclerosis Society
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 "Epstein-barr | Mononucleosis | About Virus | Mono". Centers for Disease Control and Prevention. May 10, 2018. Retrieved November 14, 2018.
- ↑ Saha, Abhik; Robertson, Erle S (May 15, 2011). "Epstein-Barr Virus–Associated B-cell Lymphomas: Pathogenesis and Clinical Outcomes". Clinical Cancer Research. 17 (10): 3056–3063. doi:10.1158/1078-0432.CCR-10-2578. ISSN 1557-3265. PMID 21372216.
- ↑ 3.0 3.1 Harley, John B.; Chen, Xiaoting; Pujato, Mario; Miller, Daniel; Maddox, Avery; Forney, Carmy; Magnusen, Albert F.; Lynch, Arthur; Chetal, Kashish; Yukawa, Masashi; Barski, Artem (2018). "Transcription factors operate across disease loci, with EBNA2 implicated in autoimmunity". Nature Genetics. 50 (5): 699–707. doi:10.1038/s41588-018-0102-3. ISSN 1546-1718.
- ↑ 4.0 4.1 "Epstein-Barr virus protein can "switch on" risk genes for autoimmune diseases". National Institutes of Health. April 16, 2018.
- ↑ Rickinson, AB; Kieff, E (2001). "Epstein-Barr virus". In Knipe, DM; Howley, PM (eds.). Fields Virology. Philadelphia, PA: Lippincott Williams & Wilkins. pp. 2575–2627.
- ↑ "Epstein-barr | Mononucleosis | Laboratory Testing | Mono". Centers for Disease Control and Prevention. January 28, 2019. Retrieved October 8, 2020.
- ↑ Hsu, J.L.; Glaser, S.L. (April 2000). "Epstein-barr virus-associated malignancies: epidemiologic patterns and etiologic implications". Critical Reviews in Oncology/Hematology. 34 (1): 27–53. ISSN 1040-8428. PMID 10781747.
- ↑ 8.0 8.1 8.2 Priatel, John J; Chung, Brian K; Tsai, Kevin; Tan, Rusung (April 9, 2014). "Natural killer T cell strategies to combat Epstein–Barr virus infection". Oncoimmunology. 3: e28329. doi:10.4161/onci.28329. ISSN 2162-4011. PMC 4063158. PMID 25050206.
- ↑ Pattle, Samuel B.; Farrell, Paul J. (November 2006). "The role of Epstein-Barr virus in cancer". Expert Opinion on Biological Therapy. 6 (11): 1193–1205. doi:10.1517/14712598.6.11.1193. ISSN 1744-7682. PMID 17049016.
- ↑ Tangye, Stuart G.; Palendira, Umaimainthan; Edwards, Emily S.J. (January 20, 2017). "Human immunity against EBV—lessons from the clinic". Journal of Experimental Medicine. 214 (2): 269–283. doi:10.1084/jem.20161846. ISSN 0022-1007.
- ↑ Jha, HC; Mehta, D; Lu, J; El-Naccache, D; Shukla, SK; Kovacsics, C; Kolson, D; Robertson, ES (December 1, 2016). "Gammaherpesvirus Infection of Human Neuronal Cells". mBio. 6 (6): e01844-15. doi:10.1128/mBio.01844-15. PMID 26628726.
- ↑ Kleines, M; Schiefer, J; Stienen, A; Blaum, M; Ritter, K; Häusler, M (May 15, 2011), "Expanding the spectrum of neurological disease associated with Epstein-Barr virus activity", European Journal of Clinical Microbiology & Infectious Diseases, 30 (12): 1561–1569, doi:10.1007/s10096-011-1261-7, ISSN 1435-4373
- ↑ Lossius, Andreas; Johansen, Jorunn N.; Torkildsen, Øivind; Vartdal, Frode; Holmøy, Trygve (December 2012). "Epstein-Barr Virus in Systemic Lupus Erythematosus, Rheumatoid Arthritis and Multiple Sclerosis—Association and Causation". Viruses. 4 (12): 3701–3730. doi:10.3390/v4123701. ISSN 1999-4915. PMC 3528287.
- ↑ 14.0 14.1 White, P.D.; Thomas, J.M.; Amess, J.; Crawford, D.H.; Grover, S.A.; Kangro, H.O.; Clare, A.W. (December 1998). "Incidence, risk and prognosis of acute and chronic fatigue syndromes and psychiatric disorders after glandular fever". The British Journal of Psychiatry: The Journal of Mental Science. 173: 475–481. ISSN 0007-1250. PMID 9926075.
- ↑ 15.0 15.1 Schmaling, K.B.; Jones, J.F. (January 1996). "MMPI profiles of patients with chronic fatigue syndrome". Journal of Psychosomatic Research. 40 (1): 67–74. ISSN 0022-3999. PMID 8730646.
- ↑ 16.0 16.1 Hickie, Ian; Davenport, Tracey; Wakefield, Denis; Vollmer-Conna, Ute; Cameron, Barbara; Vernon, Suzanne D; Reeves, William C; Lloyd, Andrew (September 16, 2006). "Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study". BMJ : British Medical Journal. 333 (7568): 575. doi:10.1136/bmj.38933.585764.AE. ISSN 0959-8138. PMC 1569956. PMID 16950834.
- ↑ 17.0 17.1 Mikirova, Nina; Hunninghake, Ronald (May 3, 2014). "Effect of high dose vitamin C on Epstein-Barr viral infection". Medical Science Monitor: International Medical Journal of Experimental and Clinical Research. 20: 725–732. doi:10.12659/MSM.890423. ISSN 1643-3750. PMC 4015650. PMID 24793092.
- ↑ Proal, Amy D.; VanElzakker, Michael B. (2021). "Long COVID or Post-acute Sequelae of COVID-19 (PASC): An Overview of Biological Factors That May Contribute to Persistent Symptoms". Frontiers in Microbiology. 12: 698169. doi:10.3389/fmicb.2021.698169. ISSN 1664-302X.
- ↑ 19.0 19.1 Gold, Jeffrey E.; Okyay, Ramazan A.; Licht, Warren E.; Hurley, David J. (June 2021). "Investigation of Long COVID Prevalence and Its Relationship to Epstein-Barr Virus Reactivation". Pathogens. 10 (6): 763. doi:10.3390/pathogens10060763. ISSN 2076-0817.
- ↑ 20.0 20.1 Holmøy, Trygve (January 1, 2008). "Vitamin D status modulates the immune response to Epstein Barr virus: Synergistic effect of risk factors in multiple sclerosis". Medical Hypotheses. 70 (1): 66–69. doi:10.1016/j.mehy.2007.04.030. ISSN 0306-9877.
- ↑ "Viruses". National Multiple Sclerosis Society. Retrieved November 14, 2018.
- ↑ James, J.A.; Kaufman, K.M.; Farris, A.D.; Taylor-Albert, E.; Lehman, T.J.; Harley, J.B. (December 15, 1997). "An increased prevalence of Epstein-Barr virus infection in young patients suggests a possible etiology for systemic lupus erythematosus". The Journal of Clinical Investigation. 100 (12): 3019–3026. doi:10.1172/JCI119856. ISSN 0021-9738. PMID 9399948.
- ↑ Kang, Insoo; Quan, Timothy; Nolasco, Helena; Park, Sung-Hwan; Hong, Myung Sun; Crouch, Jill; Pamer, Eric G.; Howe, John Greg; Craft, Joe (January 15, 2004). "Defective Control of Latent Epstein-Barr Virus Infection in Systemic Lupus Erythematosus". The Journal of Immunology. 172 (2): 1287–1294. doi:10.4049/jimmunol.172.2.1287. ISSN 0022-1767. PMID 14707107.
- ↑ 24.0 24.1 Leopardi, Victoria; Chang, Yu-Mei; Pham, Andrew; Luo, Jie; Garden, Oliver A. (2021). "A Systematic Review of the Potential Implication of Infectious Agents in Myasthenia Gravis". Frontiers in Neurology. 12. doi:10.3389/fneur.2021.618021/full. ISSN 1664-2295.
- ↑ Brenner, T.; Timore, Y.; Wirguin, I.; Abramsky, O.; Steinitz, M. (October 1989). "In vitro synthesis of antibodies to acetylcholine receptor by Epstein-Barr virus-stimulated B-lymphocytes derived from patients with myasthenia gravis". Journal of Neuroimmunology. 24 (3): 217–222. ISSN 0165-5728. PMID 2553772.
- ↑ Kaminski, Henry J; Minarovits, Janos (2010). "Epstein-barr virus: Trigger for autoimmunity?". Annals of Neurology. 67 (6): 697–698. ISSN 0364-5134.
- ↑ Ryan, Julie L.; Shen, You-Jun; Morgan, Douglas R.; Thorne, Leigh B.; Kenney, Shannon C.; Dominguez, Ricardo L.; Gulley, Margaret L. (July 1, 2012). "Epstein-Barr Virus Infection Is Common in Inflamed Gastrointestinal Mucosa". Digestive Diseases and Sciences. 57 (7): 1887–1898. doi:10.1007/s10620-012-2116-5. ISSN 1573-2568. PMC 3535492. PMID 22410851.
- ↑ Goossens, HA; Nohlmans, MK; van den Bogaard, AE (May–June 1999). "Epstein-Barr virus and cytomegalovirus infections cause false-positive results in IgM two-test protocol for early Lyme borreliosis". Infection. 27 (3): 231. doi:10.1007/BF02561539. PMID 10378140.
- ↑ "MAGT1 magnesium transporter 1 [Homo sapiens (human)]". NCBI. Retrieved May 21, 2022.
- ↑ 30.0 30.1 Li, F.-Y.; Chaigne-Delalande, B; Su, H; Matthews, H; Lenardo, M.J. (2014). "XMEN disease: a new primary immunodeficiency affecting Mg2+ regulation of immunity against Epstein-Barr virus". Blood. 123 (14): 2148–2152. doi:10.1182/blood-2013-11-538686.
- ↑ Ravell, Juan; Chaigne-Delalande, Benjamin; Lenardo, Michael (December 2014). "X-linked immunodeficiency with magnesium defect, Epstein–Barr virus infection, and neoplasia disease: a combined immune deficiency with magnesium defect". Current Opinion in Pediatrics. 26 (6): 713–719. doi:10.1097/MOP.0000000000000156. ISSN 1040-8703. PMC 4306042. PMID 25313976.
- ↑ Yenamandra, Surya Pavan; Hellman, Ulf; Kempkes, Bettina; Darekar, Suhas Deoram; Petermann, Sabine; Sculley, Tom; Klein, George; Kashuba, Elena (December 2010). "Epstein-Barr virus encoded EBNA-3 binds to vitamin D receptor and blocks activation of its target genes". Cellular and molecular life sciences: CMLS. 67 (24): 4249–4256. doi:10.1007/s00018-010-0441-4. ISSN 1420-9071. PMID 20593215.
- ↑ Yu, Sanhong; Cantorna, Margherita T. (April 1, 2008). "The vitamin D receptor is required for iNKT cell development". Proceedings of the National Academy of Sciences. 105 (13): 5207–5212. doi:10.1073/pnas.0711558105. ISSN 0027-8424. PMID 18364394.
- ↑ Ramien, Caren; Pachnio, Annette; Sisay, Sofia; Begum, Jusnara; Leese, Alison; Disanto, Giulio; Kuhle, Jens; Giovannoni, Gavin; Rickinson, Alan (May 2014). "Hypovitaminosis-D and EBV: no interdependence between two MS risk factors in a healthy young UK autumn cohort". Multiple Sclerosis (Houndmills, Basingstoke, England). 20 (6): 751–753. doi:10.1177/1352458513509507. ISSN 1477-0970. PMID 24192216.
- ↑ Hoshino, Yo; Katano, Harutaka; Zou, Ping; Hohman, Patricia; Marques, Adriana; Tyring, Stephen K.; Follmann, Dean; Cohen, Jeffrey I. (November 2009). "Long-term administration of valacyclovir reduces the number of Epstein-Barr virus (EBV)-infected B cells but not the number of EBV DNA copies per B cell in healthy volunteers". Journal of Virology. 83 (22): 11857–11861. doi:10.1128/JVI.01005-09. ISSN 1098-5514. PMC 2772668. PMID 19740997.
- ↑ Rafailidis, Petros I.; Mavros, Michael N.; Kapaskelis, Anastasios; Falagas, Matthew E. (November 2010). "Antiviral treatment for severe EBV infections in apparently immunocompetent patients". Journal of Clinical Virology: The Official Publication of the Pan American Society for Clinical Virology. 49 (3): 151–157. doi:10.1016/j.jcv.2010.07.008. ISSN 1873-5967. PMID 20739216.
- ↑ Verma, Dinesh; Thompson, Jacob; Swaminathan, Sankar (March 29, 2016). "Spironolactone blocks Epstein–Barr virus production by inhibiting EBV SM protein function". Proceedings of the National Academy of Sciences. 113 (13): 3609–3614. doi:10.1073/pnas.1523686113. ISSN 1091-6490. PMID 26976570.
- ↑ Diamantopoulos, Panagiotis T.; Polonyfi, Katerina; Sofotasiou, Maria; Papadopoulou, Vasiliki; Kalala, Fani; Iliakis, Theodoros; Zervakis, Kostantinos; Tsilimidos, Gerassimos; Kouzis, Panagiotis (December 2013). "Rituximab in the treatment of EBV-positive low grade B-cell lymphoma". Anticancer Research. 33 (12): 5693–5698. ISSN 1791-7530. PMID 24324119.
- ↑ Lee, Minjung; Son, Myoungki; Ryu, Eunhyun; Shin, Yu Su; Kim, Jong Gwang; Kang, Byung Woog; Cho, Hyosun; Kang, Hyojeung (May 20, 2015). "Quercetin-induced apoptosis prevents EBV infection". Oncotarget. 6 (14): 12603–12624. doi:10.18632/oncotarget.3687. ISSN 1949-2553. PMC 4494961. PMID 26059439.
- ↑ Rolf, Linda; Muris, Anne-Hilde; Mathias, Amandine; Du Pasquier, Renaud; Koneczny, Inga; Disanto, Giulio; Kuhle, Jens; Ramagopalan, Sreeram; Damoiseaux, Jan; Smolders, Joost; Hupperts, Raymond (September 2018). "Exploring the effect of vitamin D3 supplementation on the anti-EBV antibody response in relapsing-remitting multiple sclerosis". Multiple Sclerosis (Houndmills, Basingstoke, England). 24 (10): 1280–1287. doi:10.1177/1352458517722646. ISSN 1477-0970. PMC 6108041. PMID 28731372.
- ↑ "NIH researchers make progress toward Epstein-Barr virus vaccine". National Institutes of Health (NIH). April 9, 2019. Retrieved April 10, 2019.
- ↑ Asprusten, Tarjei Tørre; Pedersen, Maria; Skovlund, Eva; Wyller, Vegard Bruun (2019). "EBV-requisitioning physicians' guess on fatigue state 6 months after acute EBV infection". BMJ paediatrics open. 3 (1): e000390. doi:10.1136/bmjpo-2018-000390. ISSN 2399-9772. PMID 30957026.
- ↑ Pedersen, Maria; Asprusten, Tarjei Tørre; Godang, Kristin; Leegaard, Truls Michael; Osnes, Liv Toril; Skovlund, Eva; Tjade, Trygve; Øie, Merete Glenne; Wyller, Vegard Bruun Bratholm (January 2019). "Predictors of chronic fatigue in adolescents six months after acute Epstein-Barr virus infection: A prospective cohort study". Brain, Behavior, and Immunity. 75: 94–100. doi:10.1016/j.bbi.2018.09.023. ISSN 1090-2139. PMID 30261303.
- ↑ Pedersen, Maria; Asprusten, Tarjei Tørre; Godang, Kristin; Leegaard, Truls Michael; Osnes, Liv Toril; Skovlund, Eva; Tjade, Trygve; Øie, Merete Glenne; Wyller, Vegard Bruun Bratholm (January 27, 2019). "Lifestyle factors during acute Epstein-Barr virus infection in adolescents predict physical activity six months later". Acta Paediatrica (Oslo, Norway: 1992). 108 (8): 1521–1526. doi:10.1111/apa.14728. ISSN 1651-2227. PMID 30685875.
- ↑ Williams, Marshall V.; Cox, Brandon; Lafuse, William P.; Ariza, Maria Eugenia (May 2019). "Epstein-Barr Virus dUTPase Induces Neuroinflammatory Mediators: Implications for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Clinical Therapeutics. 41 (5): 848–863. doi:10.1016/j.clinthera.2019.04.009. PMC 6525645. PMID 31040055.
- ↑ Kerr, Jonathan R. (February 2019). "Epstein-Barr virus induced gene-2 upregulation identifies a particular subtype of Chronic Fatigue Syndrome / Myalgic Encephalomyelitis". Frontiers in Pediatrics. 72 (10): 651–8. doi:10.3389/fped.2019.00059.
- ↑ Kerr, Jonathan R (July 17, 2019). "Epstein-Barr virus (EBV) reactivation and therapeutic inhibitors". Journal of Clinical Pathology: jclinpath–2019–205822. doi:10.1136/jclinpath-2019-205822. ISSN 0021-9746.
- ↑ Shikova, Evelina; Reshkova, Valentina; Kumanova, Аntoniya; Raleva, Sevdalina; Alexandrova, Dora; Capo, Natasa; Murovska, Modra (2020). "Cytomegalovirus, Epstein-Barr virus, and human herpesvirus-6 infections in patients with myalgic еncephalomyelitis/chronic fatigue syndrome". Journal of Medical Virology. doi:10.1002/jmv.25744. ISSN 1096-9071.
- ↑ Ruiz-Pablos, Manuel; Paiva, Bruno; Monter-Mateo, Rosario; Garcia, Nicolas; Zabaleta, Aintzane (November 15, 2021). "Epstein-Barr Virus and the Origin of Myalgic Encephalomyelitis or Chronic Fatigue Syndrome". Frontiers in Immunology. 12: 656797. doi:10.3389/fimmu.2021.656797. PMID 34867935. Retrieved June 10, 2022.
- ↑ Fevang, Børre; Wyller, Vegard Bruun Bratholm; Mollnes, Tom Eirik; Pedersen, Maria; Asprusten, Tarjei Tørre; Michelsen, Annika; Ueland, Thor; Otterdal, Kari (2021). "Lasting Immunological Imprint of Primary Epstein-Barr Virus Infection With Associations to Chronic Low-Grade Inflammation and Fatigue". Frontiers in Immunology. 12: 715102. doi:10.3389/fimmu.2021.715102. ISSN 1664-3224. PMC 8721200. PMID 34987499.
- ↑ Jason, Leonard A; Cotler, Joseph; Islam, Mohammed F; Sunnquist, Madison; Katz, Ben Z (December 25, 2020). "Risks for Developing Myalgic Encephalomyelitis/Chronic Fatigue Syndrome in College Students Following Infectious Mononucleosis: A Prospective Cohort Study". Clinical Infectious Diseases. 73 (11): e3740–e3746. doi:10.1093/cid/ciaa1886. ISSN 1058-4838. PMC 8664491. PMID 33367564.
- ↑ Cox, Brandon S.; Alharshawi, Khaled; Mena-Palomo, Irene; Lafuse, William P.; Ariza, Maria Eugenia (June 8, 2022). "EBV/HHV-6A dUTPases contribute to myalgic encephalomyelitis/chronic fatigue syndrome pathophysiology by enhancing TFH cell differentiation and extrafollicular activities". JCI Insight. 7 (11). doi:10.1172/jci.insight.158193. ISSN 0021-9738.