Primer for journalists: Difference between revisions
(→Disease onset and lifelong illness: Pediatric) |
Notjusttired (talk | contribs) m (fix ref →Blood donation and organ transplant) |
||
| (666 intermediate revisions by 49 users not shown) | |||
| Line 1: | Line 1: | ||
[[Myalgic | {{mbox|text= Editors: Edits to this Primer may require the same edits to the other [[:Category:Primers|Primers]].}} | ||
[[myalgic encephalomyelitis|Myalgic encephalomyelitis]] (ME), [[chronic fatigue syndrome]] (CFS), and [[chronic fatigue]] (CF) are widely misunderstood. In this '''Primer for journalists''', we provide evidence-based statements (with links to further reading & sources) to support journalists writing about the disease. '''Chronic Fatigue Syndrome''' must never be shortened to ''Chronic Fatigue'' in the body of an article or its headline. This has caused much confusion for readers who do not understand CFS is a debilitating lifelong illness and it is not the same as [[chronic fatigue]] (CF); CF is a symptom of many different illnesses. Although the [[Fukuda criteria|Fukuda]]<ref name="fukuda1994">{{Cite journal | last = Fukuda | first = K. | authorlink = Keiji Fukuda | last2 = Straus | first2 = S.E. | authorlink2 = Stephen Straus | last3 = Hickie | first3 = I. | authorlink3 = Ian Hickie | last4 = Sharpe | first4 = M.C. | authorlink4 = Michael Sharpe | last5 = Dobbins | first5 = J.G. | authorlink5 = James Dobbins | last6 = Komaroff | first6 = A. | authorlink6 = Anthony Komaroff | date = 1994-12-15 | title = The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group | url = https://www.researchgate.net/profile/Michael_Sharpe2/publication/247808895_The_Chronic_Fatigue_Syndrome_A_Comprehensive_Approach_to_Its_Definition_and_Study/links/0c96053201643bfc4b000000/The-Chronic-Fatigue-Syndrome-A-Comprehensive-Approach-to-Its-Definition-and-Study.pdf|journal=Annals of Internal Medicine|volume=121|issue=12 | pages = 953–959 |issn=0003-4819|pmid=7978722|via=|doi=10.7326/0003-4819-121-12-199412150-00009|publisher=American College of Physicians}}</ref> and the [[Oxford criteria|Oxford Criteria]]<ref name="PMC1293107">{{Cite journal | title = A report--chronic fatigue syndrome: guidelines for research. | url = https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1293107/|journal=Journal of the Royal Society of Medicine | date = Feb 1991|issn=0141-0768|pmc=1293107|pmid=1999813 | pages = 118–121 |volume=84|issue=2 | first = MC | last = Sharpe | first2 = LC | last2 = Archard | first3 = JE | last3 = Banatvala | first4 = LK | last4 = Borysiewicz | first5 = AW | last5 = Clare | first6 = A | last6 = David | first7 = RH | last7 = Edwards | first8 = KE | last8 = Hawton | first9 = HP | last9 = Lambert}}</ref> are used for diagnosing CFS, they are both overly broad and there is criticism that patients are being [[misdiagnosis of myalgic encephalomyelitis and chronic fatigue syndrome|misdiagnosed]] in both clinical and research settings as having CFS when in fact they are suffering from the symptom CF or another fatiguing diagnosis.<ref name="Vink2019">{{Cite journal | last = Vink | last2 = Vink-Niese | date = 2019-09-20 | title = Work Rehabilitation and Medical Retirement for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. A Review and Appraisal of Diagnostic Strategies | url = https://www.mdpi.com/2075-4418/9/4/124|journal=Diagnostics|language=en|volume=9|issue=4|page=124|doi=10.3390/diagnostics9040124|issn=2075-4418 | first = Mark | first2 = Alexandra|pmc=|pmid=|quote= | author-link = Mark Vink | authorlink2 = Alexandra Vink-Niese|access-date=|via=}}</ref><ref name="Carruthers, 2003" /><ref name="ICC2011primer" /></div><ref>{{Cite web | title = What Does a True ME Definition Look Like? | url = https://www.meadvocacy.org/what_does_a_true_me_definition_look_like|website=MEadvocacy.org|access-date=2019-01-25 | first = | last = }}</ref><ref name="fukuda1994"/><ref>[http://theargusreport.com/us-nih-report-calls-uk-definition-mecfs-scrapped/ US NIH Report Calls for UK Definition of ME/CFS to be Scrapped - The Argus Report By: Penny Swift]</ref><ref>{{Cite web | url = http://occupyme.net/2016/08/16/ahrq-evidence-review-changes-its-conclusions/|website=occupyme.net|access-date=2019-01-25 | title = AHRQ Evidence Review Changes Its Conclusions | date = Aug 16, 2016 | last = Spotila | first=Jennie | authorlink=Jennie Spotila | last2 = Dimmock | first2 = Mary | authorlink2 = Mary Dimmock|archive-url=|archive-date=}}</ref> | |||
= | There have been media reports of athletes diagnosed with ME or CFS who have recovered in a relatively short period of time after rest, supplementation, and diet changes;<ref name="Inews2018">{{Cite news |url = https://inews.co.uk/news/health/marathon-runner-quit-work-me-cfs-diet-change/ | title = Marathon runner forced to quit work after developing ME claims diet change gave him his life back | first = Claudia | last = Tanner|publisher =iNews | date = 2018}}</ref><ref name="Times2017">{{Cite news | url = https://www.thetimes.co.uk/article/muslim-fighter-with-me-who-left-an-arranged-marriage-to-win-world-title-svxhhzt57 | title = Muslim fighter with ME who left an arranged marriage to win world | last = Broadbent | first = Rick | date = 2017-12-02|work=The Times|access-date=2019-02-28|archive-url=|archive-date=|language=en|issn=0140-0460|quote=}}</ref><ref name="ABC2018">{{Cite news |url = http://www.abc.net.au/7.30/committee-reviews-potentially-harmful-and-old/10010408 |at=6mins 18s| title = Committee reviews 'potentially harmful and old fashioned' chronic fatigue treatments|publisher =ABC News | first =Andy|last = Park | first2 = Clare | last2 = O'Halloran}}</ref><ref name="London2019">{{Cite news | url = https://www.thetimes.co.uk/article/nathan-douglas-london-2012-was-the-darkest-period-of-my-life-vxt5gftcx | title = Nathan Douglas: London 2012 was the darkest period of my life | last = Broadbent | first = Rick | date = 2019-02-27|work=The Times|access-date=2019-02-28|archive-url=|archive-date=|language=en|issn=0140-0460|quote=}}</ref> these athletes may have had [[overtraining syndrome]] (which has the symptom of [[chronic fatigue]]) and not ME or CFS,<ref name="spence"/> while people with adrenal failure, [[idiopathic chronic fatigue]] or other fatiguing illnesses may be erroneously diagnosed with CFS.<ref name="recovery"/><ref name="Anoop2012"/><ref name="ICC" /> ME and CFS in professional athletes is normally a career-ending diagnosis.<ref name="Squash" /><ref name="Annadale"/><ref name="Shattered"/><ref name="Olympian"/><ref name="FIFA"/><ref name="olaf"/><ref name="LA"/> | ||
ME | |||
<embedvideo service="youtube" dimensions="400" alignment="right" container="frame" description="''What is ME/CFS'' By Open Medicine Foundation - OMF. Linda Tannenbaum, Founder & CEO/President, talks about ME/CFS and how OMF is leading research and delivering hope (2018)">https://www.youtube.com/watch?v=pqDubEeIBtA</embedvideo> | |||
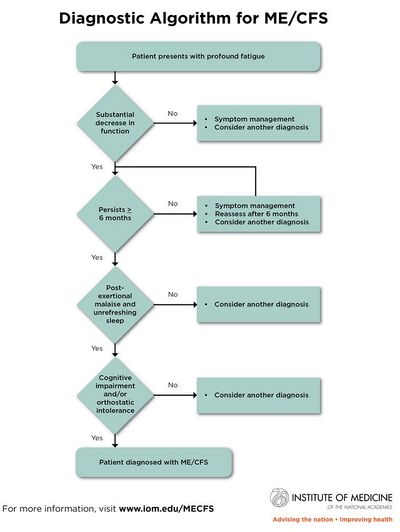
The core [[List of symptoms in ME CFS|ME/CFS symptoms]] are: [[chronic fatigue]] (CF); [[post-exertional malaise]] (PEM); [[unrefreshing sleep]]/[[Sleep dysfunction|sleep problems]]; and [[Cognitive dysfunction|cognitive impairment]]/[[brain fog]] and/or [[orthostatic intolerance]] (OI).<ref name="symptoms"/><ref name="clinicians">{{Cite web | url = https://www.nap.edu/resource/19012/MECFScliniciansguide.pdf | title = Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome - Redefining an Illness {{!}} Clinicians Guide | last = | first = | date = 2015 | publisher=Nation Academies Press|archive-url=|archive-date=|access-date= | authorlink = }}</ref>{{Rp|9-10}} A patient can have many more symptoms<ref name="what-is">{{Cite web | url = https://www.omf.ngo/what-is-mecfs/ | title = What is ME/CFS? | last = | first = | date = |archive-url=|archive-date=|access-date= | authorlink = |website=[[Open Medicine Foundation]]}}</ref> and meet different criteria. [[Systemic Exertion Intolerance Disease]] (SEID), an ME/CFS criterion, allows for a patient to be [[Systemic Exertion Intolerance Disease#Diagnostic criteria|diagnosed with the minimum core symptoms]]<ref name="DiagnosticAlgorithm">{{Cite web | url = https://www.nap.edu/resource/19012/MECFS_DiagnosticAlgorithm.jpg | title = Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness - Diagnostic Algorithm | last = | first = | author-link =| date = 2015 | website = nap.edu|archive-url=https://web.archive.org/web/20190528223706/https://www.nap.edu/resource/19012/MECFS_DiagnosticAlgorithm.jpg|archive-date=2019-05-28|access-date=}}</ref> and the patient may have other symptoms.<ref name="clinicians"/<ref name="IOM2015">{{Cite web | url = https://www.nap.edu/resource/19012/MECFScliniciansguide.pdf | title = Beyond Myalgid Encephalomyelitis/Chronic Fatigue Syndrome - Redefining an Illness - Clinician's Guide | date = 2015 | access-date=|website=nap.edu | last = | first = | authorlink = |archive-url=|archive-date= | page = 9}}</ref> The [[Canadian Consensus Criteria]] (CCC) requires the core symptoms and [[Nervous system|neurological]], [[Autonomic nervous system|autonomic]], [[Neuroendocrine system|neuroendocrine]], [[immune system]], and [[myalgia]] symptoms to meet [[Canadian Consensus Criteria#Definition|its ME/CFS diagnostic criteria]].<ref name="Carruthers, 2003">{{Cite journal | last1 = Carruthers | first1 = Bruce M. | authorlink1 = Bruce Carruthers | last2 = Jain | first2 = Anil Kumar | authorlink2 = Anil Kumar Jain | last3 = De Meirleir | first3 = Kenny L. | authorlink3 = Kenny De Meirleir | last4 = Peterson | first4 = Daniel L. | authorlink4 = Daniel Peterson | last5 = Klimas | first5 = Nancy G. | authorlink5 = Nancy Klimas | last6 = Lerner | first6 = A. Martin | authorlink6 = Martin Lerner | last7 = Bested | first7 = Alison C. | authorlink7 = Alison Bested | last8 = Flor-Henry | first8 = Pierre | authorlink8 = Pierre Flor-Henry | last9 =Joshi | first9 = Pradip | authorlink9 = Pradip Joshi | last10 = Powles | first10 = AC Peter | authorlink10 = A C Peter Powles | last11 = Sherkey | first11 = Jeffrey A. | authorlink11 = Jeffrey Sherkey | last12 = van de Sande | first12 = Marjorie I. | authorlink12 = Marjorie van de Sande | title = Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols | journal = Journal of Chronic Fatigue Syndrome | volume = 11 | issue = 2 | pages = 7-115 | date = 2003 | pmid = | doi = 10.1300/J092v11n01_02 | |||
| url = http://phoenixrising.me/wp-content/uploads/Canadian-definition.pdf }}</ref> The [[International Consensus Criteria]] (ICC) is used to diagnose [[myalgic encephalomyelitis]] (ME) which requires the core symptoms and neurological, immune/[[Gastrointestinal system|gastrointestinal]]/genitourinary impairment, and [[portal:Energy metabolism|energy metabolism]]/[[Ion transportation|ion transport]] impairment [[International Consensus Criteria#Criteria|symptoms for a diagnosis]].<ref name="ICC">{{Cite journal | last = Carruthers | first=Bruce M. | author-link = Bruce Carruthers | last2 = van de Sande | first2 = Marjorie I. | authorlink2 = Marjorie van de Sande | last3 = De Meirleir | first3 = Kenny L. | authorlink3 = Kenny De Meirleir | last4 = Klimas | first4 = Nancy G. | author-link4 = Nancy Klimas | last5 = Broderick | first5 = Gordon | author-link5 = Gordon Broderick | last6 = Mitchell | first6 = Terry | authorlink6 = Terry Mitchell | last7 = Staines | first7 = Donald | author-link7 = Donald Staines | last8 = Powles | first8 = A.C. Peter | authorlink8 = A C Peter Powles | last9 = Speight | first9 = Nigel | authorlink9 = Nigel Speight | last10 = Vallings | first10 = Rosamund | authorlink10 = Rosamund Vallings | last11 = Bateman | first11 = Lucinda | authorlink11 = Lucinda Bateman | last12 = Baumgarten-Austrheim | first12 = Barbara | author-link12 = Barbara Baumgarten-Austrheim | last13 = Bell | first13 = David | author-link13 = David Bell | last14 = Carlo-Stella | first14 = Nicoletta | author-link14 = Nicoletta Carlo-Stella | last15 = Chia | first15 = John | author-link15 = John Chia | last16 = Darragh | first16 = Austin | author-link16 = Austin Darragh | last17 = Jo | first17 = Daehyun | author-link17 = Daehyun Jo | last18 = Lewis | first18 = Donald | author-link18 = Donald Lewis | last19 = Light | first19 = Alan | author-link19 = Alan Light | last20 = Marshall-Gradisnik | first20 = Sonya | author-link20 = Sonya Marshall-Gradisnik | last21 = Mena | first21 = Ismael | author-link21 = Ismael Mena | last22 = Mikovits | first22 = Judy | author-link22 = Judy Mikovits | last23 = Miwa | first23 = Kunihisa | author-link23 = Kunihisa Miwa | last24 = Murovska | first24 = Modra | author-link24 = Modra Murovska | last25 = Pall | first25 = Martin | author-link25 = Martin Pall | last26 = Stevens | first26 = Staci | author-link26 = Staci Stevens | date = 2011-08-22 | title=Myalgic encephalomyelitis: International Consensus Criteria | url = https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2796.2011.02428.x|journal=Journal of Internal Medicine|language=en|volume=270|issue=4|pages=327–338|doi=10.1111/j.1365-2796.2011.02428.x|issn=0954-6820|pmc=3427890|pmid=21777306|via=}}</ref> | |||
ME/CFS | The acronym ME/CFS is widely used in research, by clinicians, patient organizations, and patients. | ||
"The most common overlapping condition with ME/CFS is [[fibromyalgia]]."<ref name="ICC2011primer">{{citation | last1 = Carruthers | first1 = BM | authorlink1 = Bruce Carruthers | last2 = van de Sande | first2 = MI | authorlink2 = Marjorie van de Sande | last3 = De Meirleir | first3 = KL | authorlink3 = Kenny de Meirleir | last4 = Klimas | first4 = NG | authorlink4 = Nancy Klimas | last5 = Broderick | first5 = G | authorlink5 = Gordon Broderick | last6 = Mitchell | first6 = T | authorlink6 = Terry Mitchell | last7 = Staines | first7 = D | authorlink7 = Donald Staines | last8 = Powles | first8 = ACP | authorlink8 = A C Peter Powles | last9 = Speight | first9 = N | authorlink9 = Nigel Speight | last10 = Vallings | first10 = R | authorlink10 = Rosamund Vallings | last11 = Bateman | first11 = L | authorlink11 = Lucinda Bateman | last12 = Bell | first12 = DS | authorlink12 = David Bell | last13 = Carlo-Stella | first13 = N | authorlink13 = Nicoletta Carlo-Stella | last14 = Chia | first14 = J | authorlink14 = John Chia | last15 = Darragh | first15 = A | authorlink15 = Austin Darragh | last16 = Gerken | first16 = A | authorlink16 = Anne Gerken | last17 = Jo | first17 = D | authorlink17 = Daehyun Jo | last18 = Lewis | first18 = DP | authorlink18 = Donald Lewis | last19 = Light | first19 = AR | authorlink19 = Alan Light | last20 = Light | first20 = KC | authorlink20 = Kathleen Light | last21 = Marshall-Gradisnik | first21 = S | authorlink21 = Sonya Marshall-Gradisnik | last22 = McLaren-Howard | first22 = J | authorlink22 = John McLaren-Howard | last23 = Mena | first23 = I | authorlink23 = Ismael Mena | last24 = Miwa | first24 = K | authorlink24 = Kunihisa Miwa | last25 = Murovska | first25 = M | authorlink25 = Modra Murovska | last26 = Stevens | first26 = SR | authorlink26 = Staci Stevens | title = Myalgic encephalomyelitis: Adult & Paediatric: International Consensus Primer for Medical Practitioners | date = 2012 | isbn = 978-0-9739335-3-6 | url = http://www.investinme.org/Documents/Guidelines/Myalgic%20Encephalomyelitis%20International%20Consensus%20Primer%20-2012-11-26.pdf}}</ref><ref name="Primer2014"/><ref name="Jason2001">{{Cite journal | last= Jason | first = Leonard | last2 = Taylor | first2 = R.R. | last3 = Kennedy | first3 = C.L. | last4 = Song | first4 = S | last5 = Johnson | first5 = D | last6 = Torres | first6 = S.R. | date = 2001-01-01 | title = Chronic fatigue syndrome: Comorbidity with fibromyalgia and psychiatric illness | url = https://www.researchgate.net/publication/285787383_Chronic_fatigue_syndrome_Comorbidity_with_fibromyalgia_and_psychiatric_illness|journal=Medicine and Psychiatry|volume=4 | pages = 29–34}}</ref> While some have posited ME/CFS and fibromyalgia are variants of the same illness, [[Benjamin Natelson]], MD summoned considerable amounts of data that suggest the two illnesses differ with different pathophysiologic processes leading to different treatments.<ref>{{Cite journal | last = Natelson | first = Benjamin H. | date = 2019-02-19 | title = Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Fibromyalgia: Definitions, Similarities, and Differences | url = https://www.clinicaltherapeutics.com/article/S0149-2918(19)30003-7/abstract|journal=Clinical Therapeutics|language=English|volume=41|issue=4 | page = 612|doi=10.1016/j.clinthera.2018.12.016|issn=0149-2918|pmid=30795933}}</ref> | |||
The | |||
Unfortunately, a [[Psychologization|psychiatric approach]] has been taken with ME/CFS, but this is changing. At this time there are no approved drug treatments. [[Graded exercise therapy]] (GET) and [[cognitive behavioral therapy]] (CBT) are used in the [[United Kingdom|UK]] inappropriately for treating ME/CFS. The [[Centers for Disease Control and Prevention]] (CDC) website states "ME/CFS is a '''biological illness''', not a psychologic disorder" and impacts multiple body systems.<ref name="etiology">{{Cite web | title = Etiology and Pathophysiology {{!}} Presentation and Clinical Course {{!}} Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/etiology-pathophysiology.html|website=[[Centers for Disease Control and Prevention]] | date = 2018-11-08| access-date = 2019-01-22 |language=en-us}}</ref> The CDC recognizes the hallmark symptom of PEM which is a worsening of symptoms after physical, mental or emotional exertion<ref name="symptoms">{{Cite web | title = Symptoms of ME/CFS {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/symptoms-diagnosis/symptoms.html|website=[[Centers for Disease Control and Prevention]] | date = 2019-01-18|access-date=2019-01-22|language=en-us}}</ref> and says [[ME/CFS]] is a "disabling and complex disease."<ref name="whatis">{{Cite web | url = https://www.cdc.gov/me-cfs/about/index.html | title = What is ME/CFS? {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | date = 2019-01-18 | website = [[Centers for Disease Control and Prevention]]|language=en-us|access-date=2019-04-12}}</ref> | |||
=== | [[File:SEID algorithm.JPG|400px|thumb|right|Diagnostic Algorithm for [[Systemic Exertion Intolerance Disease|SEID]]'s minimum [[List of symptoms in ME CFS#Systemic Exertion Intolerance Disease (SEID) symptom list|ME/CFS core symptoms]]]] | ||
==What do we know?== | |||
ME is a debilitating illness that has been recognized as a neurological disease by the [[World Health Organization]] (WHO) since 1969.<ref name="icd10">{{Cite book | url = https://apps.who.int/iris/bitstream/handle/10665/70934/ICD_10_1969_eng_v2a.pdf?sequence=3&isAllowed=y | title = International Classification of Diseases | last = World Health Organization | first = |publisher=WHO| year = 1969|isbn=|editor-link=|edition=Eighth revision|volume=2|location=Geneva|pages=173|chapter=|quote=Encephalomyelitis (chronic),<br>(myalgic, benign) 323|editor-last2=|editor-link2=}}</ref> | |||
It is a systemic [[Neuro-immune disease|neuroimmune]] disease characterized by [[post-exertional malaise]] (PEM) (a severe worsening of symptoms after even minimal [[exertion]]). It causes dysregulation of both the [[immune system]] and the [[nervous system]]. The effects of ME are devastating enough to leave [[Severe and very severe ME|25% of patients housebound or bedbound]]. For moderate to severe patients, the disability of living with ME is like living with late-stage cancer, advanced stage AIDS, or congestive heart failure for decades. | |||
In many parts of the world, it is commonly called chronic fatigue syndrome. | |||
[[ME/CFS]] costs the US economy up to $24 billion per year in direct medical costs, and lost production.<ref name="IOM2015MECFS" /> Despite this, funding for research is not commensurate with the level of disease burden. In the 2015 financial year, the [[National Institutes of Health]] (NIH) provided only $5 million in research funding for ME/CFS, which is less funding than hayfever. This is in stark contrast to funding levels for other similarly disabling illnesses, like [[multiple sclerosis]] ($105 million) and HIV/AIDS ($3 billion).{{Citation needed|reason=Reference needed for NIH funding levels | date = 4 November 2019}} The [[Institute of Medicine]], a special advisory committee of the [[U.S. Department of Health and Human Services]] (HHS) (ref: [[Chronic Fatigue Syndrome Advisory Committee|CFSAC]] recommendations) and [[NIH]] expert advisory panel agree that it is imperative to increase research funding into ME/CFS.<ref name="NIHP2PFIN" /> | |||
== Disease onset and course of illness== | |||
[[Onset of ME/CFS|ME/CFS can begin]] from many acute/sudden<ref name="Chu2019">{{Cite journal | last = Chu | first = Lily | authorlink = Lily Chu | last2 = Valencia | first2 = Ian J. | authorlink2 = Ian Valencia | last3 = Garvert | first3 = Donn W. | authorlink3 = | last4 = Montoya | first4 = Jose G. | authorlink4 = Jose Montoya | authorlink5 = | date = Jan 14, 2019 | title = Onset patterns and course of myalgic encephalomyelitis/chronic fatigue syndrome | url = https://www.frontiersin.org/articles/10.3389/fped.2019.00012/abstract|journal=Frontiers in Pediatrics|volume=|issue=|pages=|doi=10.3389/fped.2019.00012|quote=|via=}}</ref> events: usually [[Viral onset hypothesis|viral]] or [[Bacterial disease onset|bacterial]] infections, but also [[trauma]], surgery or childbirth, [[anaphylaxis|allergic reaction]], and [[stress]].<ref>{{Cite web | url = https://www.cdc.gov/grand-rounds/pp/2016/20160216-presentation-chronic-fatigue-H.pdf | title = CDC Public Health Grand Rounds - Chronic Fatigue Syndrome - Advancing Research and Clinical Education | last = | first = | author-link =| date = |website=[[Centers for Disease Control and Prevention]] | page = 6|archive-url=|archive-date=|access-date=}}</ref> There is also a gradual onset in some people,<ref name="Chu2019" /><ref name="clinical">{{Cite web | url = https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/index.html | title = Presentation and Clinical Course of ME/CFS {{!}} Information for Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome ME/CFS | date = 2018-12-12 | website = [[Centers for Disease Control and Prevention]]|language=en-us|access-date=2019-02-07}}</ref> that is not attributed to any one event. Occasionally, ME/CFS has been triggered by [[Environmentally acquired illness|environmental toxins]] or the receipt of an [[Vaccine|immunizing injection]].<ref>[https://www.masscfids.org/images/pdf/Primer_2014.pdf Chronic Fatigue Syndrome Myalgic Encephalomyelitis - Primer for Clinical Practitioners - 2014 Edition - Massachusettes CFIDS/FM Assoc]</ref> Some say that the disease [[Myalgic encephalomyelitis|ME]] always has an acute/sudden [[Infection|infectious]] onset.<ref name="Evans2018">{{Cite journal | last = Evans | first = Meredyth | authorlink = Meredyth Evans | authorlink2 = Leonard Jason | date = 2018 | title = Onset patterns of chronic fatigue syndrome and myalgic encephalomyelitis | url = https://www.openaccessjournals.com/articles/Onset%20patterns%20of%20chronic%20fatigue%20syndrome%20and%20myalgic%20encephalomyelitis.pdf|journal=Research on Chronic Diseases|volume=|issue=|pages=2|quote=|via= | last2 = Jason | first2 = Leonard}}</ref> | |||
The disease [[ME/CFS]] is often diagnosed when a person does not recover from a [[flu-like illness]], [[mononucleosis]] or another [[HHV|herpesvirus]], [[Q fever]], an unidentified [[virus]], or [[:Category:Infectious agents|other infection]], and meets one or more [[Definitions of myalgic encephalomyelitis and chronic fatigue syndrome|diagnostic criteria for either ME, CFS, or ME/CFS]].<ref name="IOM2015"/>{{Rp|157-158}}<ref>[http://www.cortjohnson.org/blog/2014/01/09/lipkin-study-vagus-nerve-hhv-6-loomis-hhv-6-foundation/ The Lipkin Study, The Vagus Nerve Infection Hypothesis and HHV-6: Kristin Loomis of the HHV-6 Foundation Talks – Pt. I - Health Rising - By: Cort Johnson - June 2014]</ref> Patients experience [[List of symptoms in ME CFS|numerous symptoms]] and disease severity which fluctuate from day to day, week to week, month to month, year to year, and even decade to decade. Furthermore, symptoms and disease severity vary among patients.<ref name="Primer2014"/><ref name="WebMD">[http://www.webmd.com/chronic-fatigue-syndrome/chronic-fatigue-syndrome-symptoms Chronic Fatigue Syndrome - Symptoms - Web MD]</ref> | |||
The CDC recognizes that there can be different causes and it is possible that two or more things could cause the illness. Areas of research include infections, [[immune system]] changes, physical or psychological [[stress]] affecting body chemistry, changes in [[Metabolic|energy production]], and a possible [[Genetics of chronic fatigue syndrome|genetic link]].<ref name="causes">{{Cite web | title = Possible Causes {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/about/possible-causes.html|website=[[Centers for Disease Control and Prevention]] | date = 2019-01-18|access-date=2019-01-27|language=en-us}}</ref><ref name="etiology" /> The CDC notes there are abnormalities with the immune system, [[Metabolic|cellular metabolism]], neuroendocrine disturbances, and [[blood pressure]] or heart rate regulation.<ref name="etiology" /> | |||
===Not a mental health disorder=== | |||
In the past, CFS was believed to be a mental health disorder. This is why the CDC now states: "ME/CFS is a biological illness, not a psychologic disorder. Patients with ME/CFS are neither malingering nor seeking secondary gain. These patients have multiple pathophysiological changes that affect multiple systems."<ref name="etiology" /> | |||
===No clear evidence that ME/CFS is contagious=== | |||
[[:Category:Infectious agents|Infectious episodes]] have led to [[List of myalgic encephalomyelitis and chronic fatigue syndrome outbreaks|outbreaks]] over the years and 72% of ME/CFS patients report an [[Onset of ME/CFS|onset]] of a viral or bacterial infection.<ref>{{Cite web | url = https://www.cdc.gov/grand-rounds/pp/2016/20160216-presentation-chronic-fatigue-H.pdf | title = CDC Public Health Grand Rounds - Chronic Fatigue Syndrome - Advancing Research and Clinical Education | last = | first = | author-link =| date = |website=cdc.gov | page = 6|archive-url=|archive-date=|access-date=}}</ref> Nowadays, the vast majority of ME/CFS cases are sporadic rather than epidemic - although some outbreaks have been caused by known viruses such as the [[2003 Hong Kong outbreak|SARS pandemic]] and [[2019 Coronavirus pandemic outbreak|COVID-19]] - there is no clear evidence that sporadic ME/CFS cases are contagious.<ref name="pediatricprimer">{{Cite journal | last = Rowe | first = Katherine S. | last2 = Vallings | first2 = Rosamund | last3 = Stewart | first3 = Julian M. | last4 = Speight | first4 = Nigel | last5 = Schwartz | first5 = Malcolm S. | last6 = Medow | first6 = Marvin S. | last7 = Gurwitt | first7 = Alan | last8 = Friedman | first8 = Kenneth J. | last9 = Underhill | first9 = Rosemary A. | date = 2017 | title = Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer |url = https://www.frontiersin.org/articles/10.3389/fped.2017.00121/full|journal=Frontiers in Pediatrics|language=English|volume=5|doi=10.3389/fped.2017.00121|issn=2296-2360}}</ref> | |||
Families, partners, and friends do not report contracting ME/CFS from someone with the disease nor do patients report passing it on to others.<ref>{{Cite web | url = http://forums.prohealth.com/forums/index.php?threads/is-cfs-contagious.189664/ | title = Is CFS contagious? |website = ProHealth Forums|access-date=2019-02-13}}</ref> However, [[Rosemary Underhill|Underhill]] and O'Gorman (2006) researched 219 patients with ME/CFS, and concluded that close household contact and genetics were both risk factors for CFS, finding 3.2% of spouses/partners of those with CFS also had the illness.<ref name="UnderhillInfectious">{{Cite journal | last = Underhill | first = Rosemary A. | last2 = O'Gorman | first2 = Ruth | date = 2006-01-01 | title = Prevalence of Chronic Fatigue Syndrome and Chronic Fatigue Within Families of CFS Patients | url = https://doi.org/10.1300/J092v13n01_02|journal=Journal of Chronic Fatigue Syndrome|volume=13|issue=1|pages=3–13|doi=10.1300/J092v13n01_02|issn=1057-3321}}</ref> This was a higher prevalence than all genetic relatives except children of patients. Because ME/CFS can run in families, a [[Genetics of chronic fatigue syndrome|genetic link]] is a line of research recommended by the CDC.<ref name="causes" /><br /> | |||
[[Michael Sikora]] and collaborators at the [[Open Medicine Foundation]] hope that their research on the role of [[T cell]]s and immune-related [[Genetics of chronic fatigue syndrome|genes]] will help address "whether ME/CFS is an autoimmune or infectious disease, or simply an activation of the immune system".<ref name="omf-funded">{{Cite web | url = https://www.omf.ngo/2018/06/04/omf-funded-research/ | title = OMF funded research | date = Jun 4, 2018 | website = [[Open Medicine Foundation]]}}</ref> | |||
====Blood donation and organ transplant==== | |||
A [[Blood donation|tissue and blood donation]] ban is in force for ME/CFS in the [[United Kingdom]] (even if recovered),<ref name="BloodUK">{{Cite web | url = https://my.blood.co.uk/KnowledgeBase | title = Knowledgebase|website=My Donor Record - Health, Eligibility & Travel | last = | first = | authorlink = |archive-url=|archive-date=|url-status=|access-date=2021-10-08}}</ref> [[Australia]],<ref name="donate">{{Cite web|url = https://www.donateblood.com.au/faq/chronic-fatigue-syndrome |title=Chronic fatigue syndrome – I have/had chronic fatigue syndrome. Can I donate?|access-date=2022-05-25|website = Australian Red Cross}}</ref> [[New Zealand]],<ref name="NZBlood">{{Cite web |url = https://www.nzblood.co.nz/become-a-donor/am-i-eligible/detailed-eligibility-criteria/ | title = Detailed Eligibility Criteria|access-date=2022-05-25 | date = |website=NZ Blood|quote=}}</ref> most of [[Canada]],<ref name="Wilson2014">{{Cite journal | title = The Use of Preliminary Scientific Evidence in Public Health: A Case Study of XMRV | date = 2014-04-08 | url = https://journals.plos.org/plosmedicine/article?id=10.1371/journal.pmed.1001623|journal=PLOS Medicine|volume=11|issue=4| pages = e1001623 | last = Wilson | first = Kumanan | last2 = Atkinson | first2 = Katherine | last3 = Keelan | first3 = Jennifer|language=en|doi=10.1371/journal.pmed.1001623|pmc=PMC3979645|pmid=24714396|issn=1549-1676}}</ref> and for a time also in the [[United States]],<ref name="post">{{Cite web | url = http://voices.washingtonpost.com/checkup/2010/12/red_cross_bars_chronic_fatique.html | title = Red Cross bars chronic fatigue patients from donating blood | last = Stein | first = Rob | authorlink = | date = Dec 3, 2010 | website = Washington Post|archive-url=|archive-date=|access-date=2022-05-25}}</ref> initially due to the research on [[Xenotropic murine leukemia virus-related virus|XMRV]] as being the likely infectious trigger of CFS<ref>{{Cite web | url = https://www.meassociation.org.uk/2010/04/xmrv-testing-in-the-uk/ | title = XMRV testing in the UK | last = | first = | author-link =| date = 2010 | website = [[ME Association]]|language=en-US|archive-url=|archive-date=|access-date=2019-02-13}}</ref> and showing that patients carried the virus.<ref name="post" /> Two papers on XMRV were retracted as the result was caused by laboratory contamination,<ref name="Redaction2012">{{Cite journal | date = Dec 2012 | title = Redaction, retraction and reaction | url = https://www.nature.com/articles/nrmicro2928|journal=Nature Reviews Microbiology|language=en|volume=10|issue=12 | pages = 799|doi=10.1038/nrmicro2928|issn=1740-1534}}</ref><ref name="transfusion">{{Cite web | url = https://transfusionnews.com/2012/10/05/multicenter-study-finds-no-correlation-between-chronic-fatigue-syndrome-and-xmrv/ | title = Multicenter Study Finds No Correlation between Chronic Fatigue Syndrome and XMRV|website=transfusionnews.com|access-date=2019-02-13}}</ref> but many blood donation bans remain.<ref name="Wilson2014"/> | |||
The US American Red Cross no longer has statements barring transfusions or transplants for CFS,<ref name="redcross">{{Cite web | url = https://www.redcrossblood.org/faq.html#eligibility-health|access-date=2019-02-13 | title = Frequently Asked Questions | date = | last = | first = | authorlink = |archive-url=|archive-date=|website=American Red Cross|quote=Your search for "Chronic fatigue syndrome" returned no results.}}</ref> but patients are expected to be in "good health" which would exclude most.<ref name="redcross"/> The American Association of Blood Banks advises to either accept or defer ME/CFS donors based on "clinical judgment of the donor's health status".<ref name="AABBOct2012">{{Cite web | last = American Association of Blood Banks | url = https://www.aabb.org/docs/default-source/default-document-library/regulatory/eid/xmrvfactsheet.pdf?sfvrsn=cd162fa3_2 | date = October 2012 | title = Xenotropic Murine Leukemia Virus-Related Virus (XMRV) and other Polytropic Murine Leukemia Viruses (pMLV)|pages = 3 |quote=An updated AABB Association Bulletin #12-05 (November 2012) states that individual collectors of blood and cellular therapy products should accept or defer donors with a history of CFS based on their clinical judgment of the donor's health status.|access-date=2022-05-25}}</ref> Patient charities discourage ME/CFS patients from donating blood,<ref name="MassBlood2015">{{Cite web | url = https://www.massmecfs.org/research/recent-research/19-xmrv/237-aabbs-recommendation-on-cfidsme-and-blood-donation | title = AABB's recommendation on ME/CFS and blood donation | date = Nov 25, 2015 |website=[[Massachusetts ME/CFS & FM Association]]|access-date=2022-05-25}}</ref> | |||
== Mini-Docs == | |||
<embedvideo service="youtube" dimensions="400" alignment="right" container="frame" description="By Jen Brea/TED (2016)">https://www.youtube.com/watch?v=Fb3yp4uJhq0</embedvideo> | |||
[[What happens when you have a disease doctors can't diagnose - TED Talk (2016)|''What happens when you have a disease doctors can't diagnose'']] By [[Jennifer Brea|Jen Brea]]/TED | |||
Five years ago, TED Fellow Jen Brea became progressively ill with myalgic encephalomyelitis, commonly known as chronic fatigue syndrome, a debilitating illness that severely impairs normal activities and on bad days makes even the rustling of bed sheets unbearable. In this poignant talk, Brea describes the obstacles she's encountered in seeking treatment for her illness, whose root causes and physical effects we don't fully understand, as well as her mission to document through film the lives of patients that medicine struggles to treat.<ref>{{Cite web | url = https://www.youtube.com/watch?v=Fb3yp4uJhq0 | title = What happens when you have a disease doctors can't diagnose | date = Jan 17, 2017|access-date=|website=YouTube | last = Brea | first=Jennifer | authorlink=Jennifer Brea|archive-url=|archive-date=|publisher=TED}}</ref><ref>{{Cite web | url = https://www.ted.com/talks/jen_brea_what_happens_when_you_have_a_disease_doctors_can_t_diagnose | title = What happens when you have a disease doctors can't diagnose | date = Jun 2016|access-date=|website=TED | last = Brea | first=Jennifer | authorlink=Jennifer Brea|archive-url=|archive-date=}}</ref> | |||
<embedvideo service="youtube" dimensions="400" alignment="right" container="frame" description="By Veronica Weber/Palo Alto Online (2015)">https://www.youtube.com/watch?v=9_HwOUiImvw</embedvideo> | |||
[[Invisible Illness - Stories of Chronic Fatigue Syndrome|''Invisible Illness - Stories of Chronic Fatigue Syndrome'']] By Veronica Weber/Palo Alto Online | |||
This mini documentary reveals 3 stories of people who have been impacted by [[Chronic Fatigue Syndrome]] - a little known disease that affects roughly 836,000-2.5 million people in the U.S. and receives little research funding. They share emotions of treating loved ones with the disease, their frustrations of being ignored by members of society and the healthcare industry and express hopes of treatment and research. Video by Veronica Weber/Palo Alto Online<ref>{{Cite web | url = https://www.youtube.com/watch?v=9_HwOUiImvw | title = Invisible Illness - Stories of Chronic Fatigue Syndrome | date = Jul 10, 2015 |access-date=|website=YouTube | last = Weber | first = Veronica | authorlink=|archive-url=|archive-date=|publisher=Palo Alto Online}}</ref> | |||
<embedvideo service="youtube" dimensions="400" alignment="right" container="frame" description="By Dr. David Kaufman/Unrest (2018)">https://www.youtube.com/watch?v=RC9TjgE_PlU</embedvideo> | |||
''Diagnosis and Management of Myalgic Encephalomyelitis and Chronic Fatigue Syndrome'' By Dr. [[David Kaufman]]/[[Unrest|''Unrest'']] | |||
This video on the diagnosis and management of myalgic encephalomyelitis and chronic fatigue syndrome is '''part of the Unrest Continuing Education module''', made available through the American Medical Women’s Association and Indiana University School of Medicine, and in partnership with #MEAction. US medical providers can visit: https://www.unrest.film/cme to register to watch [[Unrest]] online for free and receive Continuing Education credit.<ref>{{Cite web | url = https://www.youtube.com/watch?v=RC9TjgE_PlU | title = Diagnosis and Management of Myalgic Encephalomyelitis and Chronic Fatigue Syndrome | date = Oct 16, 2018|access-date=|website=YouTube | last = | first = | authorlink = David Kaufman|archive-url=|archive-date=|publisher=Unrest Film}}</ref> | |||
==Epidemiology == | |||
In the [[United States]], 836,000 - 2.5 million people suffer from ME/CFS. "The total economic costs of ME/CFS are estimated at $17 to $24 billion annually."<ref name="clinicians" /> Some CFS patients can work with [https://www.dol.gov/general/topic/disability/jobaccommodations job accommodations] but 1/3 to 1/2 become unemployed and [[Disability|many rely on SSDI/SSI]].<ref>[https://www.masscfids.org/job-accommodations Job Accommodations - MASS CFIDS]</ref> | |||
*[[Epidemiology of myalgic encephalomyelitis and chronic fatigue syndrome|Epidemiology]] | |||
:All races and cultures are afflicted with ME/CFS.<ref>[http://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-9-91 Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-sectional study in primary care - July 2011]</ref><ref name="epidemiology">{{Cite web | title = Epidemiology {{!}} Presentation and Clinical Course {{!}} Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/epidemiology.html|website=[[Centers for Disease Control and Prevention]] | date = 2018-11-08|access-date=2019-01-29|language=en-us}}</ref> Children and adolescents are also diagnosed.<ref>{{Cite web | title = ME/CFS in Children {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/me-cfs-children/index.html|website=[[Centers for Disease Control and Prevention]] | date = 2019-01-18|access-date=2019-01-29|language=en-us}}</ref><ref>{{Cite web | title = Pediatric ME/CFS Home Page | url = https://www.massmecfs.org/pediatric-me-cfs-home-page|website=massmecfs.org|access-date=2019-01-29}}</ref> | |||
*[[Female predominant diseases]] | |||
:Like many [[Autoimmune disease|autoimmune]] and [[Neuro-immune disease|neuro-immune]] diseases where mostly women are afflicted,<ref>[http://www.rightdiagnosis.com/artic/fact_sheet_autoimmune_disease_in_women_nwhic.htm Fact Sheet Autoimmune Disease in Women: NWHIC - Right Diagnosis - Aug 2015]</ref> the ME/CFS female/male patient ratio per Capelli et al. is 6:1<ref>{{Cite journal | title = Chronic fatigue syndrome/myalgic encephalomyelitis: an update | url = https://www.ncbi.nlm.nih.gov/pubmed/21244747|journal=International Journal of Immunopathology and Pharmacology | date = Oct 2010|issn=0394-6320|pmid=21244747 | pages = 981–989|volume=23|issue=4|doi=10.1177/039463201002300402 | first = E. | last=Capelli | first2 = R. | last2 = Zola | first3 = L. | last3 = Lorusso | first4 = L. | last4 = Venturini | first5 = F. | last5 = Sardi | first6 = G. | last6 = Ricevuti}}</ref> while the CDC states 4:1.<ref name="epidemiology"/> | |||
*[[Pediatric myalgic encephalomyelitis and chronic fatigue syndrome|Pediatric]] | |||
:Pediatric ME/CFS is defined by the CDC<ref>{{Cite web | url = https://www.cdc.gov/me-cfs/me-cfs-children/factsheet-healthcare-professional.html | title = Pediatric ME/CFS: Fact Sheet for Healthcare Professionals {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | date = 2017-10-10 | website = [[Centers for Disease Control and Prevention]]|language=en-us|access-date=2018-10-13}}</ref> and the [[National Academy of Medicine]] (NAM)<ref name="IOM2015"/>{{Rp|181}} although it is usually diagnosed in adults.<ref name="whatis"/> "Children below the age of 8 or 9 do not have the symptom pattern of adolescents past puberty. If the onset of the disease occurs during adolescence, the most common time of onset, the pattern is similar to that of adults."<ref>{{Cite web | url = https://www.omf.ngo/2016/06/25/mecfs-in-children-by-dr-david-s-bell-2/ | title = ME/CFS in Children - by David S. Bell, MD | date = 2016-06-25|publisher=[[Open Medicine Foundation]]|access-date=2018-08-11|language=en-US | last = Bell | first = David | authorlink = David Bell}}</ref> The prognosis in adolescents is considered to be better than in adults.<ref name="prognosis">{{Cite web | url = https://www.cdc.gov/me-cfs/healthcare-providers/presentation-clinical-course/prognosis.html | title = Prognosis {{!}} Presentation and Clinical Course {{!}} Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | date = 2018-11-08 | website = [[Centers for Disease Control and Prevention]]|language=en-us|access-date=2019-01-31}}</ref><ref>{{Cite journal | last = Rowe | first = Peter C. | last2 = Underhill | first2 = Rosemary A. | last3 = Friedman | first3 = Kenneth J. | last4 = Gurwitt | first4 = Alan | last5 = Medow | first5 = Marvin S. | last6 = Schwartz | first6 = Malcolm S. | last7 = Speight | first7 = Nigel | last8 = Stewart | first8 = Julian M. | last9 = Vallings | first9 = Rosamund | date = 2017 | title=Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer |url = https://www.frontiersin.org/articles/10.3389/fped.2017.00121/full|journal=Frontiers in Pediatrics|language=English|volume=5|doi=10.3389/fped.2017.00121|issn=2296-2360}}</ref> Children are diagnosed with ME/CFS at three months of illness under SEID and CCC and ME is diagnosed immediately under ICC.<ref>{{Cite web | url = https://www.masscfids.org/pediatric-me-cfs-links | title = Pediatric ME/CFS links|website=[[Massachusetts ME/CFS & FM Association]]|language=en-GB|access-date=2018-08-11}}</ref><ref name="clinicians" /><ref name="Carruthers, 2003" /><ref name="ICC" /> | |||
*[[Prevalence of myalgic encephalomyelitis and chronic fatigue syndrome|Prevalence]] | |||
:"Worldwide, there may be as many as 17 – 24 million people with ME/CFS."<ref>{{Cite web | url = https://ammes.org/how-many-people-have-mecfs/ | title = How Many People Have ME/CFS?|website = [[American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society]]|language=en-US|access-date=2019-01-31}}</ref> 25% of ME/CFS patients are [[Severe and very severe ME|housebound or bedbound]] at some point in their illness.<ref name="keyfacts">{{Cite web | url = https://www.nap.edu/resource/19012/MECFS_KeyFacts.pdf | title = Myalgic Encelphalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Key Facts | last = | first = | author-link =| date = 2015 | website = nap.edu|archive-url=https://web.archive.org/web/20190327085836/https://www.nap.edu/resource/19012/MECFS_KeyFacts.pdf|archive-date=2019-03-27|url-status=dead|access-date=}}</ref><ref name="IOM2015"/>{{Rp|32}} 90% of patients are undiagnosed.<ref name="whatis"/> | |||
*[[Prognosis for myalgic encephalomyelitis and chronic fatigue syndrome|Prognosis]] | |||
:The prognosis for a patient diagnosed with ME/CFS is considered to be poor with only a minority (a median estimate of 5%) returning to pre-morbid levels of functioning.<ref name="Cairns2005">{{Cite journal | last = Cairns | first = R. | author-link = | last2 = Hotopf | first2 = M. | authorlink2 = Matthew Hotopf | date = Jan 2005 | title = A systematic review describing the prognosis of chronic fatigue syndrome | url = https://www.ncbi.nlm.nih.gov/pubmed/15699087|journal=Occupational Medicine (Oxford, England)|volume=55|issue=1|pages=20–31|doi=10.1093/occmed/kqi013|issn=0962-7480|pmid=15699087|quote=|via=}}</ref> The majority of patients remains significantly impaired. A substantial improvement however is noted in an estimated 40% of patients.<ref name="Cairns2005" /><ref name="Joyce1997">{{Cite journal | last= Joyce | first = J. | last2 = Hotopf | first2 = M. | last3 = Wessely | first3 = S. | date = Mar 1997 | title = The prognosis of chronic fatigue and chronic fatigue syndrome: a systematic review | url = https://www.ncbi.nlm.nih.gov/pubmed/9093600|journal=QJM: monthly journal of the Association of Physicians|volume=90|issue=3|pages=223–233|issn=1460-2725|pmid=9093600}}</ref> | |||
==ME vs CFS vs CF== | ==ME vs CFS vs CF== | ||
The name | The name myalgic encephalomyelitis (ME) was coined following an [[Epidemic myalgic encephalomyelitis|outbreak]] of an illness at the [[1955 Royal Free Hospital outbreak|Royal Free Hospital]] in the UK, in 1955. The name chronic fatigue syndrome (CFS) was coined by the [[Centers for Disease Control and Prevention]] (CDC) following an [[List of myalgic encephalomyelitis and chronic fatigue syndrome outbreaks|outbreak]] of a [[flu-like illness]] at [[1984 Incline Village chronic fatigue syndrome outbreak|Incline Village]], at Lake Tahoe, in the 1980s. There is disagreement as to whether ME and CFS are the same disease, entirely separate illnesses, or whether ME constitutes a more severe subset of CFS. Adding to the confusion, the diagnostic name given to patients is more often dependent on the country in which they live, than differing characteristics of their illness, as some countries use CFS (eg: US, [[Australia]]), and other countries (particularly in Europe) use ME. At this point in time, there is no clear biological evidence to resolve whether the illnesses are the same or different, and there is unlikely to be a resolution until firm [[diagnostic biomarker|biomarkers]] have been identified. As such, many patients and researchers use the term ME/CFS.<ref name="Klimas20140621video" /> See: [[Definitions of ME and CFS]]. | ||
The name Chronic Fatigue Syndrome is itself controversial, as many consider it | The name Chronic Fatigue Syndrome is itself controversial, as many consider it [[stigma and discrimination|stigmatizing]]. In February 2016, Dr [[Anthony Komaroff]], who was part of the CDC group of clinicians who coined the name Chronic Fatigue Syndrome, said of it: | ||
<blockquote>"I think that was a big mistake because the name, in my opinion, and the opinion of a lot of people, it both trivializes and stigmatizes the illness. It makes it seem unimportant, maybe not even real"<ref name="Komaroff20160217video" /></blockquote> | |||
It is important to distinguish between ME/CFS and chronic fatigue (CF), which is a symptom of many different medical conditions (e.g.: anemia, [[hepatitis]], [[multiple sclerosis]], [[Thyroid disease|hypothyroidism]], [[depression]], ME/CFS). "Chronic fatigue" is not an illness in its own right and it is incorrect and misleading to refer to ME/CFS as "chronic fatigue". While [[fatigue]] is a component of ME/CFS, many consider [[post-exertional malaise]] (PEM) to be the cardinal feature of ME/CFS.<ref name="Carruthers, 2003" /><ref name="IOM2015MECFS" /> | |||
==Evidence of a disease== | |||
== | === Symptoms === | ||
[[List of symptoms in ME CFS|Symptom presentation varies enormously]] between individuals. Symptom presentation also varies within individuals, as individuals often report that symptoms change over time (increasing or decreasing) and new symptoms may appear while others disappear.<ref>{{Cite web | title = Symptoms and Diagnosis of ME/CFS {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/symptoms-diagnosis/index.html|website=[[Centers for Disease Control and Prevention]] | date = 2019-01-18|access-date=2019-02-01|language=en-us}}</ref> There are many symptoms which people with ME/CFS experience, though those listed below are the core symptoms found in all patients. | |||
=== | [[File:Cfs woman sketch.jpg|435x435px|thumb|[[Post-exertional malaise]] (PEM) is a [[List of symptoms in ME CFS|''worsening'' of ME/CFS symptoms]] after minimal [[Exertion#Exertion in ME.2FCFS|physical, mental or emotional exertion]]. Worsening symptoms may include [[chronic fatigue]]; [[flu-like symptoms]], [[brain fog]]/[[cognitive dysfunction]], and [[word-finding problems]], [[unrefreshing sleep]], [[headache]]s and [[migraine]]s, [[chronic pain]], [[Myalgia|muscle pain]] and [[muscle fatigability]], [[orthostatic intolerance]], [[neurally mediated hypotension]], or [[Postural orthostatic tachycardia syndrome|POTS]] and more. The [[Delayed onset of post-exertional symptoms|onset of PEM can be delayed 24-72 hours]] and depending on ME/CFS severity can last days, weeks, or even months]] | ||
*[[Post-exertional malaise]] (PEM) is the hallmark symptom of ME/CFS. After physical or | [[File:Rosa SEID.JPG|400px|thumb|left|Rosa age 25 in 1986 and mildly ill with [[Systemic Exertion Intolerance Disease#Diagnostic criteria|ME/CFS's core symptoms]]. In 2015 the [[SEID]] criteria were released. Rosa read about [[Post-exertional malaise|PEM]] and how it is delayed and makes [[List of symptoms in ME CFS|ME/CFS symptoms]] like [[Chronic fatigue|CF]], [[Orthostatic intolerance|OI]], and [[Cognitive dysfunction|cognition]] worse. Her life since [[Pediatric myalgic encephalomyelitis/chronic fatigue syndrome|age 17]] fell into place as she never connected her worsening symptoms with increased [[Exertion#Exertion in ME.2FCFS|physical or mental activity]] 24-72 hours prior. She believes not understanding PEM made her illness worsen over the years and is now disabled meeting the [[Canadian Consensus Criteria|CCC]] with PEM.]] | ||
[[File:Brian vastag.png|thumb|left|[[Brian Vastag]] is an American and award-winning journalist and an ME/CFS patient that won a disability case against Prudential, proving that PEM is a severe symptom that keeps him from gainful employment]] | |||
[[File:PEM1.JPG|300px|thumb|right|I think [https://twitter.com/hashtag/twofacesofme?f=tweets&vertical=default&src=hash #TwoFacesofME] is a really important hashtag. We’re only out and about at our best, and our (more frequent) worst often remains hidden. I’m convinced it’s why #[[ME/CFS|MEcfs]] research funding is so low - the problem isn’t visible enough. I’m seriously ill in both these photos.<ref>{{Cite web | url = https://twitter.com/JackCroxall/status/1085900441328803840 | title = I think #TwoFacesofME is a really important hashtag. We’re only out and about at our best, and our (more frequent) worst often remains hidden. I’m convinced it’s why #MEcfs research funding is so low - the problem isn’t visible enough. I’m seriously ill in both these photos.pic.twitter.com/hNjK5140kv | last = Croxall | first = Jack | date = 2019-01-17 | website = @JackCroxall|language=en|access-date=2019-01-17}}</ref>]] | |||
[[File:PEM4.JPG|300px|thumb|right|First photo, me in my [[Severe and very severe ME|wheelchair on a rare trip out]]. Second photo, the inevitable crash. Eye half closed, [[Speech difficulties|slurred speech]], [[Dizziness|dizzy]], weak, etc. #TwoFacesofME<ref>{{Cite web | url = https://twitter.com/hopeforMEyet/status/1085909800766980096 | title = First photo, me in my wheelchair on a rare trip out. Second photo, the inevitable crash. Eye half closed, slurred speech, dizzy, weak, etc. #TwoFacesofMEpic.twitter.com/P2OPnnpQvF | last = Karen | date = 2019-01-17 | website = @hopeforMEyet|language=en|access-date=2019-01-17}}</ref>]] | |||
[[File:PEM5.JPG|300px|thumb|right|#TwoFacesofME First photo from the morning, the other one from the afternoon ( when I failed to nap 30-60 minutes). I am Not [[Severe and very severe ME|severely ill]], and my life is ok, even [so] I wish that one day science will help me & all the #MeCfs sufferers around the globe.<ref>{{Cite web | title = #TwoFacesofME First photo from the morning, the other one from the afternoon ( when I failed to nap 30-60 minutes). I am Not severely ill, and my life is ok, even do I wish that one day science will help me & all the #MeCfs sufferers around the globe.pic.twitter.com/wmhfHcfP0p | url = https://twitter.com/Authorportrait/status/1085815918846832640 | website = @Authorportrait | date = 2019-01-17|access-date=2019-01-17|language=en | first = Henry | last = Köhler}}</ref>]] | |||
*[[Post-exertional malaise]] (PEM) is the hallmark symptom of ME/CFS. After physical, mental or emotional [[exertion]] (which for some patients can be a shower or making out a to-do list, others grocery shopping, socializing or reading a news article, while some just walking to the mailbox, getting to the doctor or mentally following a T.V. program)<ref name="what-is" /><ref name="symptoms"/><ref name="Cairns2005" /> there is a payback of significant '''worsening''' [[List of symptoms in ME CFS|ME/CFS symptoms]] which can be [[Delayed onset of post-exertional symptoms|delayed for 24-72 hours or more]]<ref name="symptoms"/><ref name="Lindheimer2017">{{Cite journal | last = Lindheimer | first=Jacob B. | last2 = Meyer | first2 = Jacob D. | last3 = Stegner | first3 = Aaron J. | last4 = Dougherty | first4 = Ryan J. | last5 = Van Riper | first5 = Stephanie M. | last6 = Shields | first6 = Morgan | last7 = Reisner | first7 = Amanda | last8 = Shukla | first8 = Sanjay K. | last9 = Light | first9 = Alan R. | date = 2017-04-03 | title = Symptom variability following acute exercise in myalgic encephalomyelitis/chronic fatigue syndrome: a perspective on measuring post-exertion malaise | url = https://www.tandfonline.com/doi/full/10.1080/21641846.2017.1321166|journal = Fatigue: Biomedicine, Health & Behavior |language=en|volume=5|issue=2 | pages = 69–88|doi=10.1080/21641846.2017.1321166|issn=2164-1846}}</ref><ref name="Yoshiuchi2007">{{Cite journal | last = Yoshiuchi | first = Kazuhiro | last2 = Cook | first2 = Dane B. | last3 = Ohashi | first3 = Kyoko | last4 = Kumano | first4 = Hiroaki | last5 = Kuboki | first5 = Tomifusa | last6 = Yamamoto | first6 = Yoshiharu | last7 = Natelson | first7 = Benjamin H. | date = 2007-12-05 | title = A real-time assessment of the effect of exercise in chronic fatigue syndrome | url = https://www.ncbi.nlm.nih.gov/pubmed/17655887|journal=Physiology & Behavior|volume=92|issue=5 | pages = 963–968|doi=10.1016/j.physbeh.2007.07.001|issn=0031-9384|pmc=2170105|pmid=17655887}}</ref> and can last 24 hours and even days, weeks, or months.<ref name="VanNess2010">{{Cite journal | last = VanNess | first=J. Mark | last2 = Stevens | first2 = Staci R. | last3 = Bateman | first3 = Lucinda | last4 = Stiles | first4 = Travis L. | last5 = Snell | first5 = Christopher R. | date = Feb 2010 | title = Postexertional malaise in women with chronic fatigue syndrome | url = https://www.ncbi.nlm.nih.gov/pubmed/20095909|journal=Journal of Women's Health (2002)|volume=19|issue=2|pages=239–244|doi=10.1089/jwh.2009.1507|issn=1931-843X|pmid=20095909}}</ref><ref>[https://www.fda.gov/downloads/forindustry/userfees/prescriptiondruguserfee/ucm368806.pdf The Voice of the Patient.] A series of reports from the U.S. Food and Drug Administration’s (FDA’s) Patient-Focused Drug Development Initiative. September 2013</ref> The patient will experience even greater fatigue as well as exasperate the [[flu-like symptoms]] and body [[pain]]. Every patient experiences different symptoms and symptom severity from different activities and exertion output according to how sick he or she is with the disease.<ref name="prognosis" /><ref name="what-is" /><ref name="Cairns2005" /> Regarding PEM the [[CFIDS Association of America]] states: | |||
<blockquote>This is a term which describes a symptom in which exercise or exertion can bring on [[malaise]] (illness). In the case of people with ME/CFS, malaise often occurs during a period some 24-72 hours after exertion. For example, in some cases, a short walk can worsen ME/CFS symptoms two days later. This lack of understanding about the delayed onset of symptoms has, in the past, made it harder to test for ME/CFS. Follow up tests, taken less than 24 hours after an initial exercise test, may show that the patient can still perform activities at the same level (before post exertional malaise has a chance to take hold).<ref>[http://www.whathealth.com/awareness/event/internationalcfsmeawarenessday.html What Health - International CFS/ME Awareness Day 2017 - CFIDS Association of America]</ref></blockquote> | |||
*[[chronic fatigue]] | |||
*[[cognitive dysfunction]] | |||
*[[orthostatic intolerance]] (OI) such as [[postural orthostatic tachycardia syndrome]] (POTS) or [[neurally mediated hypotension]] (NMH) | |||
*[[unrefreshing sleep]]/[[sleep dysfunction|sleep disturbance]] <ref name="DiagnosticAlgorithm" /><ref name="clinicians" /> | |||
==== Other possible symptoms ==== | |||
*[[chronic pain]] | |||
*[[immune system]] | |||
*<span class="plainlinks">[[:Category:Neurological signs and symptoms|neurological signs and symptoms]]</span> See also: [[neuroinflammation]]. | |||
*[[List of symptoms in ME CFS|List of symptoms in ME/CFS]] | |||
=== Comorbids === | |||
*[[fibromyalgia]] (FMS) | |||
*[[irritable bowel syndrome]] (IBS) | |||
*[[multiple chemical sensitivity]] (MCS) | |||
*[[temporomandibular joint disorder]] (TMJ) <ref>[http://solvecfs.org/what-is-mecfs/ What is ME/CFS? - Solve ME/CFS Initiative]</ref> | |||
=== Government guides on symptoms === | |||
'''US Government guides on symptoms''' | |||
*[https://www.nap.edu/resource/19012/MECFScliniciansguide.pdf Clinicians Guide] via The [[Institute of Medicine report]] (IOM) | |||
*[https://www.cdc.gov/me-cfs/symptoms-diagnosis/symptoms.html CDC - ME/CFS Symptoms] | |||
'''Canada guides on symptoms''' | |||
*[http://linkis.com/org/tUheh Alberta Clinicians Guide] | |||
*[ | |||
===Biological abnormalities=== | ===Biological abnormalities=== | ||
Because there is currently no biomedical test for ME/CFS, many have incorrectly assumed that there are no medical abnormalities found in people with the | Because there is currently no biomedical test for ME/CFS, many have incorrectly assumed that there are no medical abnormalities found in people with the illness. As a result, ME/CFS symptoms are often considered to be [[Medically unexplained physical symptoms|medically unexplained]], and therefore [[Psychologization|psychological]] in origin. While it is true that the illness is poorly understood, many biological abnormalities have been found in a range of different body systems, particularly in the [[central nervous system]], [[autonomic nervous system]], [[immune system]], and [[Metabolic|energy metabolism]].<ref name="IOM2015MECFS" /> Unfortunately, none have yet proved to be specific enough to ME/CFS as to be useful as a [[Diagnostic biomarker|biomarker]] of the disease, and many were identified in small studies, which need replication. Whilst there have been [[List of abnormal findings in chronic fatigue syndrome and myalgic encephalomyelitis|many abnormalities identified]] found to be associated with the disease, it cannot yet be determined whether these are a cause or consequence. | ||
* [[Gastrointestinal system]] | |||
* [[Natural killer cell]] | |||
==== Notable studies ==== | |||
* | * [[Cytokine#Notable_studies|Cytokine ("Notable studies")]] | ||
*Immune findings | *Immune findings by [[Mady Hornig]] & [[Ian Lipkin]]<ref name="Hornig20150201immune" /> | ||
*[[ | *[[List of enterovirus infection studies]] | ||
=== | *2014, [[Neuroinflammation]] Japanese Neuroinflammation study<ref name="NakatomiY2014" /> | ||
*2015, Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: Evidence of inflammatory pathology<ref name="stanfordleptin">{{Cite journal | last1 = Stringer | first1 = EA | last2 = Baker | first2 = KS | last3 = Carrol | first3 = IR | last4 = Montoya | first4 = JG | authorlink4 = Jose Montoya | last5 = Chu | first5 = L | authorlink5 = Lily Chu | last6 = Maeker | first6 = HT | last7 = Younger | first7 = JW | authorlink7 = Jarred Younger| title = Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: Evidence of inflammatory pathology | journal = J Transl Med.| date = Apr 9, 2013 | pmid = 23570606 | pmc = 3637529 | doi = 10.1186/1479-5876-11-93| url = http://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-11-93 }}</ref> - [https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-11-93 (Full text)] | |||
::Younger's Leptin study | |||
*2014, Right Arcuate Fasciculus Abnormality in Chronic Fatigue Syndrome<ref name="Zeineh2014">{{Cite journal | last = Zeineh | first = Michael M. | author-link = Michael Zeineh | last2 = Kang | first2 = James | last3 = Atlas | first3 = Scott W. | last4 = Raman | first4 = Mira M. | last5 = Reiss | first5 = Allan L. | last6 = Norris | first6 = Jane L. | last7 = Valencia | first7 = Ian | last8 = Montoya | first8 = Jose G. | date = 2014-10-29 | title = Right Arcuate Fasciculus Abnormality in Chronic Fatigue Syndrome | url = https://pubs.rsna.org/doi/10.1148/radiol.14141079|journal=Radiology|volume=274|issue=2 | pages = 517–526|doi=10.1148/radiol.14141079|issn=0033-8419}}</ref> | |||
<blockquote>Bilateral [[white matter]] atrophy is present in CFS. No differences in perfusion were noted. Right hemispheric increased FA may reflect degeneration of crossing fibers or strengthening of short-range fibers. Right anterior arcuate FA may serve as a [[Diagnostic biomarker|biomarker]] for CFS.</blockquote> | |||
:*2014, [[Brains of People With Chronic Fatigue Syndrome Offer Clues About Disorder - New York Times: Well (2014)|Brains of People With Chronic Fatigue Syndrome Offer Clues About Disorder By David Tuller - New York Times: Well]] | |||
[[File:ME-CFS Brain Images.jpg|500px|thumb|center|Top scans: Healthy control patient; Bottom scans: chronic fatigue syndrome (CFS) patient. Image By: [[Michael Zeineh]]]] | |||
*2016, [[Metabolic features of chronic fatigue syndrome]] | |||
*2019, [[Evidence of widespread metabolite abnormalities in Myalgic encephalomyelitis/chronic fatigue syndrome: assessment with whole-brain magnetic resonance spectroscopy (2019) Mueller, et al|Evidence of widespread metabolite abnormalities in Myalgic encephalomyelitis/chronic fatigue syndrome: assessment with whole-brain magnetic resonance spectroscopy]]<ref name="Mueller2019">{{Cite journal | url = https://link.springer.com/epdf/10.1007/s11682-018-0029-4 | title = Evidence of widespread metabolite abnormalities in Myalgic encephalomyelitis/chronic fatigue syndrome: assessment with whole-brain magnetic resonance spectroscopy | last = Mueller | first = Christina | authorlink= | last2 = Lin | first2 = Joanne | authorlink2 = | date = 2019 | journal=Brain Imaging and Behavior|volume=14|issue= | pages = 562–572|doi=10.1007/s11682-018-0029-4|archive-url=|archive-date=|access-date=2019-01-17 | last3 = Sheriff | first3 =Sulaiman | authorlink3 = | last4 = Maudsley | first4 = Andrew | authorlink4 = | last5 = Younger | first5 = Jarred | authorlink5 = Jarred Younger}}</ref> | |||
**2018, [https://www.youtube.com/watch?v=rxdzaWD5wfU ME/CFS Involves Brain Inflammation: Results from a Ramsay Pilot Study]<ref>{{Cite web | url = https://www.youtube.com/watch?v=rxdzaWD5wfU | title = ME/CFS Involves Brain Inflammation: Results from a Ramsay Pilot Study | date = Dec 14, 2018|access-date=|website=YouTube | last = Younger | first=Jarred | authorlink=Jarred Younger|archive-url=|archive-date=|publisher=SolveCFS}}</ref> (TALK) | |||
===Causes & triggers=== | |||
*Outbreaks - see [[List of myalgic encephalomyelitis and chronic fatigue syndrome outbreaks|List of outbreaks]] | |||
*Outbreaks - see [[List of outbreaks]] | *Possible infectious triggers: [[Enterovirus]]es, [[Epstein-Barr virus]]<ref name="Hickie2006" />, [[Q fever]]<ref name="Hickie2006" />, [[Ross River virus]]<ref name="Hickie2006" />, [[mononucleosis]]<ref name="Jason, Katz, 2017" />, ([[Ebola virus disease|Ebola]]?)<ref name="Hickie2006" /> | ||
*Possible infectious triggers: [[Enterovirus]]es, [[Epstein-Barr virus]]<ref name="Hickie2006"/>, Q | *Non-viral triggers - [[trauma]], chemical | ||
*Non-viral triggers - trauma, chemical | |||
== Tests == | |||
* [[Natural killer cell]] (NKC) Blood Test | |||
* Sleep study for [[sleep apnea]], [[Restless legs syndrome|restless leg syndrome]], and other sleep disturbances. | |||
* [[Tilt table test]] for [[Orthostatic intolerance|OI]] or [[Postural orthostatic tachycardia syndrome|POTS]]. | |||
=== | ==Treatments== | ||
There are currently no [[U.S. Food and Drug Administration|Food and Drug Administration]] (FDA) approved treatments for ME/CFS. Treatments consist mostly of symptom management, rather than treatment of the underlying cause of the disease, which is not yet understood.<ref name="Primer2014" /> There are many [[:Category:Potential_treatments|potential treatments]], though their evidence-base is limited, as most research into treatments has gone into psychological approaches to treatment. | |||
=== | === Drugs === | ||
[[File:Ampligen.jpg|200px|thumb|right|Ampligen]] | |||
Two treatments that have garnered much attention are [[Ampligen]], produced by [[AIM ImmunoTech]] (formerly Hemispherx Biopharma), and [[Rituximab]]. Many people have reported improvements from Ampligen, and a few recovered but relapsed when they stopped taking it.<ref name="TownCFS">{{Cite web | url = https://www.newyorker.com/culture/personal-history/a-town-for-people-with-chronic-fatigue | title = A Town for People with Chronic Fatigue Syndrome|website=New Yorker | date = Sep 3, 2019 | first = Mike | last = Mariani|access-date=2022-04-13}}</ref> | |||
''' | Attempts to obtain FDA approval for Ampligen in the US have failed, but it is available to some people on [[compassionate use]].<ref name="experimental">{{Cite web | url = https://ammes.org/experimental-treatments/ | title = Experimental treatments | last = | first = | date = |website=[[American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society]]|language=en-US|archive-url=|archive-date=|access-date=2021-03-18}}</ref> [[Argentina]] approved the use of Ampligen for [[Severe and very severe ME|severe ME/CFS]] in 2016.<ref>{{Cite news | url = http://www.globenewswire.com/news-release/2016/08/23/866212/0/en/Hemispherx-Biopharma-Announces-Major-Breakthrough-Approval-for-Commercial-Sale-of-Rintatolimod-U-S-Tradename-Ampligen-to-Treat-Severe-Cases-of-Myalgic-Encephalomyelitis-Chronic-Fat.html | title = Hemispherx Biopharma Announces Major Breakthrough: Approval for Commercial Sale of Rintatolimod (U.S. Tradename: Ampligen®) to Treat Severe Cases of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) in the Argentine Republic | last = Hemispherx Biopharma, Inc. | date = Aug 23, 2016|work=GlobeNewswire News Room|access-date=2018-08-13|archive-url=|archive-date=|language=en-US}}</ref><ref>{{Cite news | url = http://cdn2.hubspot.net/hubfs/150154/docs/Hemispherx-Executive-Informational-Overview-11-27-16.pdf | title = Hemispherx Biopharma, Inc. Executive Informational Overview | last = | first = | date = Nov 27, 2016|work=Crystal Research Associates|access-date=|archive-url=|archive-date=|format=PDF}}</ref> Also in 2016, it was made available on a limited basis in Europe.<ref>{{Cite web | url = https://www.bizjournals.com/philadelphia/news/2016/07/25/hemispherx-ships-ampligen-for-european-chronic.html | title = Hemispherx ships Ampligen for European chronic fatigue syndrome program | last = George | first = John | date = Jul 25, 2016 | website = bizjournals.com|archive-url=|archive-date=|access-date=2018-08-13}}</ref> In July 2018, AIM ImmunoTech announced the expansion of its US [[compassionate use]] program, '''AMP-511''', to new ME/CFS patients for the first time in over a year.<ref>[http://www.4-traders.com/HEMISPHERX-BIOPHARMA-INC-31148494/news/Hemispherx-BioPharma-Opens-FDA-Approved-Reimbursement-Based-Expanded-Access-Treatment-Program-for-26862569/ Hemispherx BioPharma : Opens FDA-Approved Reimbursement Based Expanded Access Treatment Program for ME/CFS to New Enrollees - 4 Traders]</ref><ref>{{Cite web | url = https://finance.yahoo.com/news/hemispherx-biopharma-inc-announces-advancement-133000883.html | title = Hemispherx Biopharma Inc. Announces Advancement in Expanded Access Program for Ampligen in the Treatment of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | last = | first = | author-link =| date = Jan 2, 2019|website=finance.yahoo.com|publisher=GlobeNewswire|language=en-US|archive-url=|archive-date=|access-date=2019-02-10}}</ref> | ||
[[Rituximab]], a lymphoma drug, had shown promising results in initial trials in Norway,<ref>{{Cite journal | last = Fluge | first = Øystein | authorlink = Øystein Fluge | last2 = Risa | first2 = Kristin | authorlink2 = | last3 = Lunde | first3 = Sigrid | author-link3 = | last4 = Alme | first4 = Kine | authorlink4 = | last5 = Rekeland | first5 = Ingrid Gurvin | authorlink5 = | last6 = Sapkota | first6 = Dipak | authorlink6 = | last7 = Kristoffersen | first7 = Einar Kleboe | last8 = Sørland | first8 = Kari | last9 = Bruland | first9 = Ove | date = 2015-07-01 | editor-last = van der Feltz-Cornelis|editor-first = Christina | title = B-Lymphocyte Depletion in Myalgic Encephalopathy/ Chronic Fatigue Syndrome. An Open-Label Phase II Study with Rituximab Maintenance Treatment | url = http://dx.plos.org/10.1371/journal.pone.0129898|journal=PLOS ONE|language=en|volume=10|issue=7| pages = e0129898|doi=10.1371/journal.pone.0129898|issn=1932-6203|pmc=4488509|pmid=26132314|access-date=|quote=|via=}}</ref> and there were groups crowdsourcing funding for further trials in other countries. In 2017, Drs. [[Øystein Fluge]] and [[Olav Mella]] announced that their Rituximab trial had failed. They stated that they would focus their efforts on attempting to identify a subgroup of ME/CFS patients with an immune profile that would be responsive to Rituximab.<ref>{{Cite web | url = https://www.simmaronresearch.com/blog/2017/11/norwegian-rituximab-chronic-fatigue-syndrome-mecfs-trial-fails | title = Norwegian Rituximab Chronic Fatigue Syndrome (ME/CFS) Trial Fails|website=Simmaron Research|language=en-US|access-date=2021-11-21}}</ref> A phase III trial published in 2019 showed Rituximab does not improve ME/CFS.<ref name="phase3-2019">{{Cite journal | last = Fluge | first = Øystein | last2 = Rekeland | first2 = Ingrid G. | last3 = Lien | first3 = Katarina | last4 = Thürmer | first4 = Hanne | last5 = Borchgrevink | first5 = Petter C. | last6 = Schäfer | first6 = Christoph | last7 = Sørland | first7 = Kari | last8 = Aßmus | first8 = Jörg | last9 = Ktoridou-Valen | first9 = Irini | date = 2019-04-02 | title = B-Lymphocyte Depletion in Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial | url = https://www.ncbi.nlm.nih.gov/pubmed/30934066|journal=Annals of Internal Medicine|doi=10.7326/M18-1451|issn=1539-3704|pmid=30934066}}</ref><br> | |||
[[Jarred Younger]] announced in March 2016 that he will be undertaking a trial of [[low dose naltrexone]] (LDN) in ME/CFS.<ref name="younger-research">{{Cite web | last = Younger | first=Jarred | authorlink = Jarred Younger | title = Research. Neuroinflammation Pain and Fatigue Laboratory|access-date= Nov 21, 2021 | url = https://sites.uab.edu/younger/research/}}</ref> | |||
=== Treating other conditions === | |||
Different forms of [[Orthostatic intolerance|OI]] are treated with beta-blockers (Metopropol), [[Fludrocortisone]] (Florinef), and [[Mestinon|Pyridostigmine]].<ref name="Carruthers, 2003" /> When treating other diseases, illnesses, and conditions, and ME/CFS comorbidities or overlapping conditions such as sleep difficulties, cognitive problems, pain, and other symptoms it is important to remember that patients are [[Medicine sensitivities|sensitive to medications]].<ref name="monitor">{{Cite web | title = Monitoring the Use of All Medicines and Supplements {{!}} Clinical Care of Patients {{!}} Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | url = https://www.cdc.gov/me-cfs/healthcare-providers/clinical-care-patients-mecfs/monitoring-medication.html|website=[[Centers for Disease Control and Prevention]] | date = 2018-11-08|access-date=2019-01-27|language=en-us}}</ref> The CDC advice to health care practitioners is to be aware that because all drugs can cause side effects, ME/CFS patient symptoms can worsen. "This is particularly true of any medication that acts on the [[central nervous system]], such as sedating medications: therapeutic benefits can often be achieved at lower-than-standard doses. Patients with ME/CFS might tolerate or need only a fraction of the usual recommended doses for medications. After initial management with lower dosing, one or more gradual increases may be considered as necessary and as tolerated by the patient."<ref name="prognosis" /> For instance, tricyclic drugs can improve mood and help with sleep and pain. However, in some in can worsen OI.<ref name="prognosis" /> | |||
===Exercise as treatment=== | |||
[[File:J Brea TED.JPG|200px|thumb|right|[[Jen Brea|Jennifer Brea]] is an [[United States|American]] who was studying at Harvard; while on a trip to [[Kenya]] she became very ill with what would eventually be diagnosed as [[ME/CFS]]. Brea began experiencing [[Nervous system|neurological]] problems. Her neurologist diagnosed her with "conversion disorder" ([[hysteria]]). When walking home from his office, she collapsed. [[Severe and very severe ME|Jen then needed to use a wheelchair]] keeping her legs up due to [[Postural orthostatic tachycardia syndrome|POTS]] as her blood pooled into her legs]]. | |||
Previously, two common treatment recommendations for ME/CFS were [[graded exercise therapy]] (GET) and [[cognitive behavioral therapy]] (CBT). These treatments are based on disproven the hypothesis that the disease might have begun with a viral infection but has been perpetuated by [[deconditioning]] from lack of activity, and [[illness beliefs|fear and avoidance]] of activity. GET and CBT are aimed at addressing these hypothesized causes by challenging the proposed unhelpful thoughts that result in avoidance of activity and reconditioning through a gradual increase in exercise. These treatments are controversial and are at odds with much of the research literature, which suggests that exercise is harmful to people with ME/CFS. A large patient survey of treatment responses found that 74% of people who had tried GET, reported that their symptoms subsequently worsened,<ref name="MEASSUK20150529survey" /> which is consistent with other patient surveys and many research findings.<ref name="Phoenix20160222Norway2012" /><ref name="OxfordBrookesSurvey">{{Cite web|url = https://www.meassociation.org.uk/wp-content/uploads/NICE-Patient-Survey-Outcomes-CBT-and-GET-Final-Consolidated-Report-03.04.19.pdf| title = Evaluation of a survey exploring the experiences of adults and children with ME/CFS who have participated in CBT and GET interventional programmes. FINAL REPORT | last = Oxford Clinical Allied Technology and Trials Services Unit (OxCATTS)|location=Oxford Brookes University | date = Feb 27, 2019}}</ref> | |||
The [[PACE trial]], published in 2011, is the largest GET trial ever conducted. It has received much publicity as a result of its recovery rate claims, though it has come under strong criticism from within both the scientific and patient community for significant flaws in its design, and for overstating (and in some cases misrepresenting) outcomes in both the initial trial, and follow-up studies.<ref>{{Cite journal | last = Coyne | first = James Charles | last2 = Laws | first2 = Keith R | date = 2016 | title=Results of the PACE follow-up study are uninterpretable | url = http://www.thelancet.com/journals/lanpsy/article/PIIS2215-0366(15)00551-9/fulltext|journal=The Lancet Psychiatry|language=English|volume=3|issue=2| pages = e6–e7|doi=10.1016/S2215-0366(15)00551-9|issn=2215-0366|via=}}</ref> From 2015 to present day, the study was the subject of a series of investigative pieces that were highly critical of the trial by journalist Dr. [[David Tuller]]<ref name="viroblogMECFS" />, science writer [[Julie Rehmeyer]], patient advocate [[Tom Kindlon]], Dr. [[Keith Geraghty]]<ref name="Geraghty, 2017">{{Cite journal | last1 = Geraghty | first1 = Keith | authorlink1 = Keith Geraghty| title = Further Commentary on the PACE Trial: Biased Methods and Unreliable Outcomes| journal = Journal of Health Psychology | volume = | issue = | page = | date = May 2017 | doi = 10.1177/1359105317714486}}</ref>, psychologist [[Carolyn Wilshire]]<ref name="Wilshire C, et al, 2017">{{Cite journal | last1 = Wilshire | first1 = C | authorlink1 = Carolyn Wilshire | last2 = Kindlon | first2 = T | authorlink2 = Tom Kindlon | last3 = McGrath | first3 = S | authorlink3 = Simon McGrath | title = PACE trial claims of recovery are not justified by the data: a rejoinder to Sharpe, Chalder, Johnson, Goldsmith and White | journal = Fatigue: Biomedicine, Health & Behavior | volume = 5 | issue = 1 | page = 62-67 | date = 2017 | doi = 10.1080/21641846.2017.1259724}}</ref> and others. A petition signed by almost 12,000 ME/CFS patients and allies,<ref name="MEACTIONpacepetition" /> and an open letter signed by 42 ME/CFS experts from around the world,<ref name="openletrLANCET2">{{Cite web | last1 = Davis | first1 = Ronald W | authorlink1 = Ronald Davis | last2 = Edwards | first2 = Jonathan C W | authorlink2 = Jonathan Edwards | last3 = Jason | first3 = Leonard A | authorlink3 = Leonard Jason | last4 = Levin | first4 = Bruce | authorlink4 = Bruce Levin | last5 = Racaniello | first5 = Vincent R | authorlink5 = Vincent Racaniello | last6 = Reingold | first6 = Arthur L | authorlink6 = Arthur Reingold | last7 = Ablashi | first7 = Dharam V | authorlink7 = Dharam Ablashi | last8 = Baraniuk | first8 = James N | authorlink8 = James Baraniuk | last9 = Barcellos | first9 = Lisa F | authorlink9 = Lisa Barcellos | last10 = Bateman | first10 = Lucinda | authorlink10 = Lucinda Bateman | last11 = Bell | first11 = David S | authorlink11 = David Bell | last12 = Bested | first12 = Alison C | authorlink12= Alison Bested | last13 = Broderick | first13 = Gordon | authorlink13 = Gordon Broderick | last14 = Chia | first14 = John | authorlink14 = John Chia | last15 = Chu | first15 = Lily | authorlink15 = Lily Chu | last16 = Enlander | first16 = Derek | authorlink16 = Derek Enlander | last17 = Fletcher | first17 = Mary Ann | authorlink17 = Mary Ann Fletcher | last18 = Friedman | first18 = Kenneth | authorlink18 = Kenneth Friedman | last19 = Kaufman | first19 = David L | authorlink19 = David Kaufman | last20 = Klimas | first20 = Nancy | authorlink20 = Nancy Klimas | last21 = Lapp | first21 = Charles W | authorlink21 = Charles Lapp | last22 = Levine | first22 = Susan | authorlink22 = Susan Levine | last23 = Light | first23 = Alan R | authorlink23 = Alan Light | last24 = Marshall-Gradisnik | first24 = Sonya | authorlink24 = Sonya Marshall-Gradisnik | last25 = Medveczky | first25 = Peter G | authorlink25= Peter Medveczky | last26 = Nahle | first26 = Zaher | authorlink26 = Zaher Nahle | last27 = Oleske | first27 = James M | authorlink27= James Oleske | last28 = Podell | first28 = Richard N | authorlink28= Richard Podell | last29 = Shepherd | first29 = Charles | authorlink29= Charles Shepherd | last30 = Snell | first30 = Christopher R | authorlink30 = Christopher Snell | last31 = Speight | first31 = Nigel | authorlink31= Nigel Speight | last32 = Staines | first32 = Donald | authorlink32= Donald Staines | last33 = Stark | first33 = Philip B | authorlink33= Philip Stark | last34 = Stein | first34 = Eleanor | authorlink34= Eleanor Stein | last35 = Swartzberg | first35 = John | authorlink35= John Swartzberg | last36 = Tompkins | first36 = Ronald G | authorlink36= Ronald Tompkins | last37 = Underhill | first37 = Rosemary | authorlink37= Rosemary Underhill | last38 = Vallings | first38 = Rosamund | authorlink38= Rosamund Vallings | last39 = VanElzakker | first39 = Michael | authorlink39= Michael VanElzakker | last40 = Weir | first40 = William | authorlink40= William Weir | last41 = Zinn | first41 = Marcie L | authorlink41= Marcie Zinn | last42 = Zinn | first42 = Mark A | authorlink42= Mark Zinn | title = An open letter to the Lancet - again | date = Feb 10, 2016 | |||
| website = Virology Blog| url = http://www.virology.ws/2016/02/10/another-request-for-data-from-the-pace-trial/ }}</ref> were sent to The Lancet, both calling for the data to be reanalysed. Twenty-four ME/CFS organizations from 14 different countries have written to Queen Mary University London requesting that the trial data be released for reanalysis.<ref name="MEACTION20160313openletr" /> To date, the authors of the trial and editor of The Lancet have refused such requests. Despite such criticism, the PACE trial continues to influence both government and the medical profession's approach to the treatment of ME/CFS in many countries. | |||
One of the reasons that exercise may be harmful to people with ME/CFS, is the presence of [[post-exertional malaise]] (PEM), which is an exacerbation of symptoms following physical, mental or even emotional [[exertion]]. Studies have revealed immunological, muscular, [[Nervous system|neurological]], [[Autonomic nervous system|autonomic]] and [[Cardiovascular system|cardiovascular]] abnormalities in response to exercise in people with ME/CFS. As these results are not also found in healthy sedentary controls, the adverse effects of exercise cannot be said to be due to deconditioning.<ref name="TwiskF2015">{{Cite journal | last1 = Twisk | first1 = Frank NM | authorlink1 = Frank Twisk | last2 = Geraghty | first2 = Keith J | authorlink2 = Keith Geraghty | title = Deviant Cellular and Physiological Responses to Exercise in Myalgic Encephalomyelitis and Chronic Fatigue Syndrome| journal = Jacobs Journal of Physiology | volume = 1 | issue =2 | pages = 007 | date = Jul 11, 2015 | url = http://www.jacobspublishers.com/images/Physiology/J_J_Physiology_1_2_007.pdf}}</ref>{{citation needed|reason=VanNess2010 / Workwell Foundation studies need to be cited here.}}{{citation needed|reason=The Lights epigenetic changes post-exercise study needs to be cited here.}} | |||
People with ME/CFS should approach [[exercise]] with caution, as there is much evidence of potential for harm.<ref name="OxfordBrookesSurvey"/><ref name="ICC2011primer"/> | |||
[[Anaerobic threshold]], use of heart rate monitors for activity and [[pacing]]. Analeptic, not aerobic. [[Energy Envelope Theory|Energy envelope]]/pacing - people do better if stay within their envelope, than push to increase activity | |||
====Graded exercise therapy & Cognitive behavioral therapy ==== | |||
[[File:Emma Shorter.JPG|400px|thumb|right|[[Emma Shorter]], is a citizen of [[Scotland]]. Here, she gives testimony before Parliament's Petitions Committee on [[graded exercise therapy|GET]] and how it put her in a wheelchair]]. | |||
GET and CBT have been recently abandoned in the [[United Kingdom|UK]], [[Ireland]] and many parts of Europe by ME Clinics.<ref name="niceng206">{{Cite web | url = https://www.nice.org.uk/guidance/ng206 | title = Myalgic Encephalomyelitis (or Encephalopathy)/Chronic Fatigue Syndrome:diagnosis and management. NICE guideline. | last=NICE Guideline Development Group | first = | authorlink = |publisher=[[National Institute for Health and Care Excellence]] | date = 2021-10-29}}</ref> They are highly controversial and not recommended by patients, most patient advocates, and research organizations nor by many doctors or researchers outside of the UK. Based on the flawed [[PACE trial]] which used the flawed [[Oxford criteria]] to diagnose and recruit patients, GET and CBT found its way into treating people with ME/CFS. | |||
[[Exercise]], especially GET, can harm an ME/CFS patient further.<ref name="OxfordBrookesSurvey"/> | |||
*[[Jennifer Brea]] walked home from her Neurologist's office and became [[severe and very severe ME|wheelchair-bound]]. | |||
*This is an experience of serious harm due to GET shared [https://twitter.com/TomKindlon/status/846425974052966400 by K. Miles, via Tom Kindlon on Twitter]. | |||
*[[Emma Shorter]] was able to walk a few minutes a day until GET put her in a wheelchair. | |||
*[[Maik Speedy|Dr Maik Speedy]] was also seriously injured by GET and has been bedbound since. | |||
*British MP [[Brynmor John]] collapsed outside the House of Commons gym in 1998 and [[Causes of death|died]], as a result of following his doctor's advice to exercise back to health. | |||
==== Claims of recovery and cures ==== | |||
Charlatans claim they can cure CFS (per the CDC "there is no cure"<ref name="treatments">{{Cite web | url = https://www.cdc.gov/me-cfs/treatment/index.html | title = Treatment {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) | last = | first = | date = 2018-07-03 | website = [[Centers for Disease Control and Prevention]]|language=en-us|archive-url=|archive-date=|access-date=2021-11-22}}</ref>) when in reality they may be able to treat [[chronic fatigue]] (CF). ME/CFS patients experience an ongoing improper immune response and other abnormalities for at least 6 months straight with a reduction in activity with a specific symptom set for at least 50% of the time.<ref name="etiology" /><ref>{{Cite web | url = https://www.cdc.gov/me-cfs/healthcare-providers/diagnosis/iom-2015-diagnostic-criteria.html | title = IOM 2015 Diagnostic Criteria {{!}} Diagnosis {{!}} Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | date = 2018-07-10 | website = [[Centers for Disease Control and Prevention]]|language=en-us|access-date=2018-09-07}}</ref><ref>{{Cite web | url = https://www.cdc.gov/me-cfs/healthcare-providers/diagnosis/approach-to-diagnosis.html | title = Proposed Approach to ME/CFS Diagnosis in Children and Adults {{!}} Diagnosis {{!}} Healthcare Providers {{!}} Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | date = 2018-07-12 | website = [[Centers for Disease Control and Prevention]] |language=en-us|access-date=2018-09-07}}</ref> | |||
Additionally, there have been media reports of some athletes―usually amateur athletes,―diagnosed with CFS that recovered after a relatively short period of time with rest, supplementation, and diet changes,<ref name="Inews2018" /><ref name="Times2017" /><ref name="ABC2018" /><ref name="London2019" /> but they may have had [[overtraining syndrome]],<ref name="spence">{{Cite web | last = Spence | first = Vance | authorlink = Vance Spence|website=Irish M.E. Association| title = Snippets {{!}} A presentation by MERGE Chairman Dr Vance Spence on 12 November 2005 at the Oak Tree Court Conference Centre, Coventry, at the invitation of the Warwickshire Network for ME|url = https://www.imet.ie/imet_website/snippets/7th_december_2005_snippets.html|quote=(Mommersteeg et al, 2005) shows that the "burnout" experienced by athletes differs from CFS, and is certainly not ME as described in earlier literature. This is just one example of many media stories - thrown out into the public arena - which have an uncertain meaning in the context of ME/CFS}}</ref> while some people with adrenal failure, [[idiopathic chronic fatigue]] or another fatiguing illness may be erroneously diagnosed with CFS<ref name="ICC"/><ref name="recovery">{{Cite web | url = https://www.researchgate.net/profile/Diane_Cox2/publication/257764167_Severe_Chronic_Fatigue_Syndrome_CFSME_Recovery_is_possible/links/00b49525d3a11018ad000000/Severe-Chronic-Fatigue-Syndrome-CFS-ME-Recovery-is-possible.pdf | title = Severe Chronic Fatigue Syndrome: Recovery is Possible | last = Burley | first = Lucy | authorlink=Lucy Burley | last2 = Cox | first2 = Diane | authorlink2 = Diane Cox | date = Aug 1, 2007|pages=339-344|language=en|doi=10.1177/030802260707000803|archive-url=|archive-date=|url-status=|access-date=2019-02-11 | last3 = Findley | first3 = Leslie|journal=British Journal of Occupational Therapy|volume=70|issue=8 | authorlink3 = Leslie Findley}}</ref><ref name="Anoop2012">{{Cite journal | last = Devasahayam | first = Anoop | author-link = | last2 = Lawn | first2 = Tara | authorlink2 = | last3 = Murphy | first3 = Maurice | authorlink3 = | last4 = White | first4 = Peter D | authorlink4 = Peter White | date = Jan 2012 | title = Alternative Diagnoses to Chronic Fatigue Syndrome in Referrals to a Specialist Service: Service Evaluation Survey | url = https://journals.sagepub.com/doi/epub/10.1258/shorts.2011.011127|journal=JRSM Short Reports|volume=3|issue=1|pages=1–5|doi=10.1258/shorts.2011.011127|issn=2042-5333|pmc=PMC3269106|pmid=22299071|access-date=|quote=Half of all the referred patients to a specialist CFS clinic had alternative medical and psychiatric diagnoses.|via=}}</ref> ME and CFS in professional athletes normally results in very premature retirement.<ref name="Squash">{{Cite news | title = Illness robbed Marshall of crowning glory | first = Sam | last = Murley | date = Apr 10, 2019 | url = https://www.royalgazette.com/sport/article/20190410/illness-robbed-marshall-of-crowning-glory/|publisher =Royal Gazette}}</ref><ref name="Annadale">{{Cite web| title = Annadale Striders Interview - Derek Graham | url = http://annadalestriders.co.uk/derek-graham-interview/|website=Annadale Striders}}</ref><ref name="Shattered">{{Cite book |url = https://books.google.co.uk/books/about/Shattered.html?id=mkbxPAAACAAJ&redir_esc=y | title = Shattered: A Champion's Fight Against a Mystery Illness | first=Peter | last= Marshall | first2 = Nick | last2 = Kehoe | date = 2001|publisher =Mainstream}}</ref><ref name="Olympian">{{Cite news | date = May 4, 2012| title = Linley Frame: Olympian and Chronic Fatigue Syndrome sufferer|url = https://www.abc.net.au/local/audio/2012/05/04/3495770.htm|website =Australian Broadcasting Corporation}}</ref><ref name="FIFA">{{Cite web|url = http://www.fifa.com/womensworldcup/classic-players/player=michelle-akers-usa-1329785.html|archive-url=https://web.archive.org/web/20150610042710/http://www.fifa.com/womensworldcup/classic-players/player=michelle-akers-usa-1329785.html|archive-date = 2015-06-10| title = Michelle Akers USA|website=FIFA}}</ref><ref name="olaf">{{Cite news | url = https://www.welt.de/sport/gallery118782921/Benefizspiel-fuer-den-schwer-kranken-Olaf-Bodden.html | title = Benefizspiel für den schwer kranken Olaf Bodden | last = | first = | date = 2021 | website = Die Welt|archive-url=|archive-date=|url-status=|access-date=2021-11-17}}</ref><ref name="LA">{{Cite news | title = Garton enjoying life after United in LA | first = Andy | last = Mitten | date = Jul 24, 2014 | url = https://www.manchestereveningnews.co.uk/sport/football/football-news/andy-mitten-billy-garton-enjoying-7508558.amp|website =Manchester Evening News}}</ref> | |||
==Severely ill patients== | |||
Considerable variation exists in the severity of the | Considerable variation exists in the severity of the disease. The [[International Consensus Criteria]] lists the following severity levels (it should be noted that even "mild" ME/CFS consists of significant debility): | ||
*Mild = 50% reduction in pre-illness activity levels | *Mild = 50% reduction in pre-illness activity levels | ||
| Line 111: | Line 218: | ||
*Very Severe = totally bedridden, and needing help with basic functions. | *Very Severe = totally bedridden, and needing help with basic functions. | ||
At least 25% of people with ME/CFS are bedbound or housebound, often for years or even decades, so are largely an invisible population.<ref name="IOM2015MECFS"/> So invisible in fact, that they have rarely been included as part of research | At least [[Severe and very severe ME|25% of people with ME/CFS are bedbound or housebound]], often for years or even decades, so are largely an invisible population.<ref name="IOM2015MECFS" /><ref name="DerekPrisk2009" /><ref>[http://iacfsme.org/PDFS/2017JanNewsletter/8-Japan-2014-Patient-Survey.aspx ME/CFS Patient Survey Report: Ministry of Health Survey Reveals Harsh Reality of ME/CFS Patients in Japan - IACFSME - By Mieko Shinohara]</ref> So invisible in fact, that they have rarely been included as part of research because their level of debility precludes them from traveling to laboratories for required testing. The [[Open Medicine Foundation]]'s [[ME/CFS Severely Ill, Big Data Study]] will be the first in-depth study of people with a severe form of ME/CFS. This study has so far produced the groundbreaking paper [[Metabolic features of chronic fatigue syndrome]]. | ||
It is estimated that 25% of ME/CFS patients are severely ill and are housebound or bedbound. | |||
Notable patients with severe or very severe ME/CFS include [[Whitney Dafoe]], [[Karina Hansen]], [[Lynn Gilderdale]], [[Laura Hillenbrand]], [[Tom Kindlon]], [[Vanessa Li]], [[Doctor Speedy]], [[Naomi Whittingham]], [[Jamison Hill]] and [[Jessica Taylor-Bearman]]. | |||
Though uncommon, there have been [[causes of death|instances of deaths]] which have been attributed to the disease (see [[Sophia Mirza]], [[Merryn Crofts]]). National Statistics report an average of 10 - 12 deaths per year in England and Wales [[Causes of death|partly or fully caused by ME/CFS]], with almost all patients dying being of working age. | |||
<ref name="ONS2018">{{Cite web | url = https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/adhocs/008461mentionsofpostviralfatiguesyndromebenignmyalgicencephalomyelitisdeathsregisteredinenglandandwales2001to2016 | title = Mentions of postviral fatigue syndrome (benign myalgic encephalomyelitis), deaths registered in England and Wales, 2001 to 2016 | website = Office for National Statistics|access-date=2019-03-06}}</ref> | |||
==Patients and psychiatry/psychology== | |||
*Objections and scope | |||
*Objections | |||
*Mind-body dualism | *Mind-body dualism | ||
*[[Psychologization]] | |||
*[[Cognitive behavioral therapy]] | |||
*The [[PACE trial]]. See [http://www.meaction.net/wp-content/uploads/2015/05/MEAction%E2%80%93patient-view-of-the-PACE-Trial-Controversy.pdf Patient view of the PACE Trial controversy] | *The [[PACE trial]]. See [http://www.meaction.net/wp-content/uploads/2015/05/MEAction%E2%80%93patient-view-of-the-PACE-Trial-Controversy.pdf Patient view of the PACE Trial controversy] | ||
*[[Ethical issues]] | |||
*[[Patient mental health]] | *[[Patient mental health]] | ||
===Stigmatization=== | ===Stigmatization=== | ||
*Pretty young women slumped on desk | *Pretty young women slumped on desk | ||
*[[Yuppie Flu]] | *[[Yuppie Flu]] | ||
*Accusations of laziness/lethargy | *Accusations of laziness/lethargy | ||
*Epidemiological evidence - age, gender, demographic, racial/cultural | *Epidemiological evidence - age, gender, demographic, racial/cultural | ||
*[[Stigma and discrimination]] | |||
===Accusations of harassment=== | ===Accusations of harassment=== | ||
*No arrests or convictions | *No arrests or convictions<ref>{{Cite web | url = http://www.virology.ws/2016/02/01/trial-by-error-continued-a-few-words-about-harassment/ | title = Trial By Error, Continued: A Few Words About “Harassment” | last = Tuller | first = David | authorlink = David Tuller | date = Feb 1, 2016 | website = [[Virology blog]]|archive-url=|archive-date=|access-date=2019-01-21}}</ref> | ||
* | * Potential harassment and "wild speculations" about threats to researchers were unsuccessful arguments used in [[Queen Mary University of London]]'s failed attempt to deny access to the [[PACE trial]] data at the 2015 tribunal. The tribunal judgement stated that the only evidence of harassment provided was a single heckler in a single seminar.<ref name="FirstTierTribunal2015">{{Cite news | title = First-tier tribunal: Information Rights Appeal EA/2015/0269. | url = https://informationrights.decisions.tribunals.gov.uk//DBFiles/Decision/i1854/Queen%20Mary%20University%20of%20London%20EA-2015-0269%20(12-8-16).PDF | page = 40 | last = Kennedy | first = Brian | last2 = Stephenson | first2 = Darryl | last3 = Watson | first3 = Nigel|quote=The evidence of <nowiki>[expert witness]</nowiki> Professor Anderson that third parties could not identify participants from the information alone and that, when pressed, he said that the chance of an "activist" being able to discover information that would lead to individual identification was remote, it was clear that his assessment of activist behaviour was, in our view, grossly exaggerated and the only actual evidence was that an individual at a seminar had heckled Professor Chalder. The identity of those questioning the research, who had signed an open letter or supported it, was impressive.}}</ref> | ||
*Mistreatment of patients, including forced harmful treatment of children, is not mentioned. E.g., the story of "B", aged 8,<ref name="StoryofB">{{cite web | title = The Story of B - Children with ME. Appropriate ME Treatment Parliament debate | date = Jan 24, 2018 | url = https://www.youtube.com/watch?v=5HzZ4U6yU6o&autoplay=0}}</ref> and [[Ean Proctor]] and others "The Mental Health Movement: Persecution of Patients?"<ref>[http://www.theoneclickgroup.co.uk/documents/ME-CFS_docs/The%20Mental%20Health%20Movement%20-%20Persecution%20of%20Patients.pdf The Mental Health Movement: Persecution of Patients?]</ref> | |||
* A pattern of [[intimidation and bullying of PACE trial critics]] has included targeting scientists' employers, professional bodies, politicians including the [[Countess of Mar]], and smear tactics in the national press. | |||
== Working with government to move forward == | |||
Advocates met with senate staffers the week of March 16, 2016, and discussed research and drug development by the [[NIH]], the [[Centers for Disease Control and Prevention|CDC]] reinstating and increasing funding and education based on [[IOM]] recommendations and the [[HHS]] funding to develop Centers of Excellence.<ref>[http://www.meaction.net/2016/03/16/meaction-meets-with-senate-staffers/ #MEAction meets with Senate staffers]</ref> [[The MEAction Network]] reports on this ongoing process. | |||
====CDC Website updates==== | |||
*Jul 3, 2017, the CDC's Chronic Fatigue Syndrome page has been changed to [[ME/CFS|Myalgic Encephalomyelitis/Chronic Fatigue Syndrome]] (ME/CFS) and GET and CBT recommendations have been removed.<ref>{{Cite web|url = http://www.virology.ws/2017/07/10/trial-by-error-the-cdc-drops-cbtget/ | title = Trial By Error: The CDC Drops CBT/GET - Virology Blog | last = Tuller | first = David | authorlink = David Tuller | date = Jul 10, 2017 | website = [[Virology blog]]}}</ref><ref>[https://www.cdc.gov/me-cfs/index.html Myalgic Encephalomyelitis/Chronic Fatigue Syndrome - CDC.gov]</ref> | |||
*Jul 12, 2018, the "Information for Healthcare Providers" tab and its sub-tabs were updated.<ref>[https://www.cdc.gov/me-cfs/healthcare-providers/index.html Information for Healthcare Providers - ME/CFS - CDC]</ref><ref>[https://www.cdc.gov/media/releases/2018/a0712-new-website-me-cfs.html New ME/CFS Web Content for Healthcare Providers - CDC - Jul 12, 2018]</ref> | |||
* Feb 25, 2019, Dr. [[Elizabeth Unger]], Chief of CDC's Chronic Viral Disease Branch (CVDB), that houses the ME/CFS program, in collaboration between ''Medscape'' and the CDC put out brief video and commentary page with links to the CDC's July 12th, 2018 updates for medical professionals: ''[https://www.medscape.com/viewarticle/908622?src=rss Chronic Fatigue Syndrome: It's Real, and We Can Do Better].''<ref>{{Cite web | title = Chronic Fatigue Syndrome: It's Real, and We Can Do Better |url = https://www.medscape.com/viewarticle/908622?src=rss| website = Medscape |access-date=2019-02-25 | date = Feb 25, 2019 | last = Unger | first=Elizabeth | authorlink = Elizabeth Unger | last2 = Medscape | first2 = | authorlink2 = |archive-url=|archive-date=}}</ref> | |||
'''MEAction input''' | |||
*Jul 29, 2018, [https://www.meaction.net/2018/07/29/cdc-revises-its-information-on-me/ CDC Revises its Information on ME] #[[MEAction]] report on the CDC July 2017 and July 2018 website updates. Recommendations for the CDC's ME/CFS page have been created from patient feedback on the updates as well as asking for further patient input. | |||
==Expert opinions== | ==Expert opinions== | ||
===Quotes from ME/CFS experts and patients=== | ===Quotes from ME/CFS experts and patients=== | ||
*[[Individual quotes]] | |||
*[http://thoughtsaboutme.com/quotes/ Thoughts About ME - List of Quotes] | *[http://thoughtsaboutme.com/quotes/ Thoughts About ME - List of Quotes] | ||
===Doctors | ===Doctors=== | ||
< | '''UK''' | ||
*[[Jonathan Edwards]] | |||
*[[Charles Shepherd]] | |||
'''US''' | |||
<div style="column-count:4;-moz-column-count:4;-webkit-column-count:4"> | |||
*[[Lucinda Bateman]] | |||
*[[Lily Chu]] | |||
*[[David Kaufman]] | |||
*[[Nancy Klimas]] | |||
*[[Anthony Komaroff]] | |||
*[[Susan Levine]] | |||
*[[Jose Montoya]] | |||
*[[Benjamin Natelson]] | |||
*[[Daniel Peterson]] | |||
*[[Alan Pocinki]] | |||
*[[Peter Rowe]] | |||
*[[Ronald Tompkins]] | |||
*[[David Tuller]] | |||
</div> | |||
===Researchers=== | ===Researchers=== | ||
< | '''Australia''' | ||
*[[Neil McGregor]] | |||
'''UK''' | |||
*[[Keith Geraghty]] | |||
'''US''' | |||
<div style="column-count:4;-moz-column-count:4;-webkit-column-count:4"> | |||
*[[Ron Davis]] | |||
*[[Gunnar Gottschalk]] | |||
*[[Maureen Hanson]] | |||
*[[Mady Hornig]] | |||
*[[Leonard Jason]] | |||
*[[Betsy Keller]] | |||
*[[Ian Lipkin]] | |||
*[[Staci Stevens]] | |||
*[[Suzanne Vernon]] | |||
*[[Jarred Younger]] | |||
</div> | |||
===Patients=== | ===Patients=== | ||
==== | ====Australia==== | ||
==== | ===== Canada ===== | ||
*[[Scott Simpson]] | |||
====Scotland==== | |||
*[[Emma Shorter]] | |||
==== | ====US==== | ||
<div style="column-count:2;"> | |||
*[[Jennifer Brea]] | |||
*[[Carol Head]] | |||
*[[Ryan Prior]] | |||
*[[Julie Rehmeyer]] | |||
*[[Jaime Seltzer]] | |||
</div> | |||
====UK==== | |||
*[[Adam Lowe]] | |||
*[[Graham McPhee]] | |||
*[[Jessica Taylor-Bearman]] | |||
====Ireland==== | ====Ireland==== | ||
| Line 163: | Line 347: | ||
'''[[:Category:Patient groups|Patient groups]]''' | '''[[:Category:Patient groups|Patient groups]]''' | ||
<div style=" | <div style="column-count:3"> | ||
*[[:Category:American patient groups|American patient groups]] | *[[:Category:American patient groups|American patient groups]] | ||
*[[:Category:Australian patient groups|Australian patient groups]] | *[[:Category:Australian patient groups|Australian patient groups]] | ||
| Line 174: | Line 358: | ||
*[[:Category:New Zealand patient groups|New Zealand patient groups]] | *[[:Category:New Zealand patient groups|New Zealand patient groups]] | ||
*[[:Category:Norwegian patient groups|Norwegian patient groups]] | *[[:Category:Norwegian patient groups|Norwegian patient groups]] | ||
*[[:Category:Scottish patient groups|Scottish patient groups]] | |||
*[[:Category:Swedish patient groups|Swedish patient groups]] | *[[:Category:Swedish patient groups|Swedish patient groups]] | ||
</div> | </div> | ||
==Photos== | |||
*[https://phoenixrising.me/stock-photography Stock photographs suitable for ME/CFS articles] - curated by [[Phoenix Rising]] | |||
*[https://forums.phoenixrising.me/threads/the-real-me-a-stock-photography-resource-for-the-media.43734/ Advice on photograph choice] | |||
==History== | ==History== | ||
*[[Osler's Web]] is a book on the early history of CFS. | *[[Osler's Web|''Osler's Web'']] is a book by [[Hillary Johnson]] on the early history of CFS. | ||
*[[Thirty Years of Disdain]] picks up on the ME/CFS history where Osler's Web leaves off. | *[[Thirty Years of Disdain|''Thirty Years of Disdain'']] by [[Mary Dimmock]] and Matthew Lazell-Fairman picks up on the ME/CFS history where Osler's Web leaves off. | ||
*[[ | |||
*[[Sophia Mirza]]'s | === Deaths of ME/CFS patients === | ||
*[[Causes of death]] | |||
*[[Suicide]] | |||
'''Death certificates with ME or CFS''' | |||
*[[Merryn Crofts]]' death is attributed to ME. | |||
*[[Sophia Mirza]]'s death is attributed to CFS. | |||
==Other tips== | In the UK, United States, and Australia there are further reports of loved ones who have died due to ME/CFS.<ref>[https://www.newscientist.com/letter/mg19125620-600-not-sadly-the-first/ Sadly, not the first (Comment Section)]</ref> See Editor's Note<ref>[https://www.newscientist.com/article/dn9342-first-official-uk-death-from-chronic-fatigue-syndrome/ First official UK death from chronic fatigue syndrome - New Scientist]</ref> | ||
==Other tips and articles for journalists== | |||
*2021, [https://www.theopennotebook.com/2021/01/26/how-to-report-with-accuracy-and-sensitivity-on-contested-illnesses/ How to Report with Accuracy and Sensitivity on Contested Illnesses] - by ME/CFS patient and science writer Julie Rehmeyer, Open Notebook | |||
*Always interview a patient | *Always interview a patient | ||
*Interview more than one researcher (not just from the psychological | *Interview more than one researcher (not just from the psychological etiology view) | ||
*Avoid using derogatory, outdated & incorrect term "[[Yuppie Flu]]" | *Avoid using derogatory, outdated & incorrect term "[[Yuppie Flu]]" | ||
*Never shorten the disease name [[ | *Never shorten the disease name [[chronic fatigue syndrome]] (CFS) to the symptom [[chronic fatigue]] (CF). [[Chronic fatigue syndrome|CFS]], [[myalgic encephalomyelitis|ME]] or [[ME/CFS]] can be used to save print space. | ||
*Use photographic imagery that represents the reality for patients - serious illness & disability - not well-groomed & slightly tired office workers at their computer or students with a pile of books sleeping at their desk. [[Solve ME/CFS Initiative]]'s [https://www.youtube.com/watch?v=cF2OuYFDriY Times Square Public Awareness Ad] shows the reality of the disease ME/CFS. Using photos of patients whether chronically ill yet functioning or a severely ill patient | *Use photographic imagery that represents the reality for patients - serious illness & disability - not well-groomed & slightly tired office workers at their computer or students with a pile of books sleeping at their desk. [[Solve ME/CFS Initiative]]'s [https://www.youtube.com/watch?v=cF2OuYFDriY Times Square Public Awareness Ad] shows the reality of the disease ME/CFS. Using photos of patients whether chronically ill yet functioning or a severely ill patient or stock photos that reflect life with this disease is necessary. | ||
{{See also|Long_COVID#Articles_for_journalists_covering_Long_COVID|Articles for journalists covering Long COVID}} | |||
==Learn more== | ==Learn more== | ||
*[ | '''Key facts''' | ||
*[https://www.nap.edu/resource/19012/MECFS_KeyFacts.pdf Key Facts] - Institute of Medicine (2015) | |||
*[[Institute of Medicine report | |||
'''Research''' | |||
*[[Institute of Medicine report]] (2015) The CDC based its updated [https://www.cdc.gov/me-cfs/index.html ME/CFS page] on information in this report. | |||
*[[Notable studies]] | *[[Notable studies]] | ||
'''Films''' | |||
*[[ | *''[[Forgotten Plague]]'' is a US documentary about [[Ryan Prior]], an afflicted journalist who investigates the disease and its history and why the CDC has left millions sidelined from life; available for [http://www.forgottenplague.com/ streaming and DVD purchase]. (2015) | ||
[[File:Forgotten Plague.jpeg|200px|thumb|center]] | |||
*''[[Unrest]]'' is a US documentary film that aired on PBS's ''Independent Lens'' in 2018 and is available for [https://www.unrest.film/watch/#digital streaming] and [https://www.unrest.film/store/ DVD purchase]. [[Jennifer Brea]], a person with [[myalgic encephalomyelitis|ME]], directs. (2017) | |||
[[File:Unrest.jpg|400px|thumb|center]] | |||
= | '''ME/CFS organization and researchers material''' | ||
*[https://www.youtube.com/watch?v=hRdn4A2SGic Beyond the Data – Chronic Fatigue Syndrome: Advancing Research and Clinical Education] (The CDC's Dr. [[John Iskander]] interviews Dr. [[Anthony Komaroff]]. Video, 2016) | |||
*[https://drive.google.com/file/d/1h_ZwdR4567k-mSoWahnC_id0F_fAA3Fb/view Caring for People with Myalgic Encephalomyelitis] (2018) Guide for Caretakers | |||
*[http://youtu.be/c2vIQ92wU9Y ME/CFS Diagnosis and Name with Dr Nancy Klimas (video)] | |||
*[http://www.openmedicinefoundation.org/what-is-mecfs/ What is ME/CFS?] By the [[Open Medicine Foundation]] | |||
'''[[Patient mental health]]''' | |||
:Patients that had been deemed as suffering from mental health and not a biological illness: | |||
:*[[Karina Hansen]] is a young [[Denmark|Danish]] woman taken from her family for 3 1/2 years due to [[Per Fink]]'s insistence her ME was due to mental health issues. | |||
:*[[Sophia Mirza]] was taken forcibly from her home to a mental hospital only to be returned shortly after; she then died of ME. | |||
:*[[Ean Proctor]] was taken from his parents as a young boy and he was told his "parents were letting him die." He had become [[paralysis|paralyzed]] and mute and was let go in the deep end of a pool to make him swim and another time put him on a scary theme park ride to scare him into moving. | |||
<ref name=" | '''More mental health information''' | ||
| last1 | *ME/CFS is not [[depression]]. It causes a lack of energy, not a lack of desire.<ref name="Griffith, 2008">{{Cite journal | last1 = Griffith | first1 = J.P. | authorlink1 = | last2 = Zarrouf | first2 = F.A. | authorlink2 = | title = A Systematic Review of Chronic Fatigue Syndrome: Don’t Assume It’s Depression| url = https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2292451/| pmc =2292451| journal = Primary Care Companion to The Journal of Clinical Psychiatry | volume = 10 | issue = 2 | page = 120–128| date = 2008 | pmid = 18458765 | doi = 10.4088/pcc.v10n0206 }}</ref><ref name="Hawk, 2006">{{Cite journal | last1 = Hawk | first1 = C | authorlink1 = | last2 = Jason | first2 = L | authorlink2 = Leonard Jason | last3 = Torres-Harding | first3 = S | authorlink3 = Susan Torres-Harding| title = Differential diagnosis of chronic fatigue syndrome and major depressive disorder | journal = International Journal of Behavioral Medicine | volume = 13 | issue = 3 | page = 244-51 | date = 2006 | pmid = 17078775 | doi = 10.1207/s15327558ijbm1303_8 | ||
| last2 | | url = http://www.healthrising.org/wp-content/uploads/2014/04/Hawk.-Jason.-Differential-Diagnosis-of-Chronic-Fatigue-Syndrome-and-Major-Depressive-Disorder.pdf }}</ref><ref name="myhill">{{Cite web|url = http://drmyhill.co.uk/wiki/CFS_or_depression_-_what_are_the_differences| title = CFS or depression - what are the differences | last = Myhill | first = Sarah | authorlink = Sarah Myhill | website = DrMyhill|access-date = 2021-03-22}}</ref> | ||
| title | |||
| journal = | |||
| doi | |||
| url | |||
}}</ref> | |||
==See also== | |||
*[[Primer for the public#Disease_names_and_acronyms_around_the_world|Primer for the public (''Disease names and acronyms around the world'' section)]] | |||
| | |||
==References== | |||
<references> | |||
<ref name=" | <ref name="Hickie2006">{{Cite journal | last1 = Hickie | first1 = Ian | authorlink1 = Ian Hickie | last2 = Davenport | first2 = Tracey | authorlink2 = Tracey Davenport | last3 = Wakefield | first3 = Denis | authorlink3 = Denis Wakefield | last4 = Vollmer-Conna | first4 = Ute | authorlink4 = Ute Vollmer-Conna | last5 = Cameron | first5 = Barbara | authorlink5 = Barbara Cameron | last6 = Vernon | first6 = Suzanne D | authorlink6 = Suzanne Vernon | last7 = Reeves | first7 = William C | authorlink7 = William Reeves | last8 = Lloyd | first8 = Andrew | authorlink8 = Andrew Lloyd | last9 = Dubbo Infection Outcomes Study Group | title = Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study | journal = BMJ | volume = 333 | issue =575 | date = Sep 14, 2006 | pmid = 16950834 | doi = 10.1136/bmj.38933.585764.AE| url = http://www.bmj.com/content/333/7568/575.long}}</ref> | ||
| title | <ref name="Hornig20150201immune">{{Cite journal | last1 = Hornig | first1 = Mady | authorlink1 = Mady Hornig | last2 = Montoya | first2 = José G | authorlink2 = Jose Montoya | last3 = Klimas | first3 = Nancy G | authorlink3 = Nancy Klimas | last4 = Levine | first4 = Susan | authorlink4 = Susan Levine | last5 = Felsenstein | first5 = Donna | authorlink5 = Donna Felsenstein | last6 = Bateman | first6 = Lucinda | authorlink6 = Lucinda Bateman | last7 = Peterson | first7 = Daniel L | authorlink7 = Daniel Peterson | last8 = Gottschalk | first8 = C Gunnar | authorlink8 = Gunnar Gottschalk | last9 = Schultz | first9 = Andrew F | authorlink9 = Andrew Schultz | last10 = Che | first10 = Xiaoyu | authorlink10 = Xiaoyu Che | last11 = Eddy | first11 = Meredith L | authorlink11 = Meredith Eddy | last12 = Komaroff | first12 = Anthony L | authorlink12= Anthony Komaroff | last13 = Lipkin | first13 = W Ian | authorlink13 = Ian Lipkin | title = Distinct plasma immune signatures in ME/CFS are present early in the course of illness | journal = Science Advances | volume = 1 | issue = 1 | date = Feb 1, 2015 | url = http://advances.sciencemag.org/content/1/1/e1400121}}</ref> | ||
| journal = | <ref name="Primer2014">{{Cite web | last1 = ((International Association for Chronic Fatigue Syndrome / Myalgic Encephalomyelitis)) | authorlink = International Association for Chronic Fatigue Syndrome/Myalgic Encephalomyelitis | last2 = Friedberg | first2 = Fred | authorlink2 = Fred Friedberg | last3 = Bateman | first3 = Lucinda | authorlink3 = Lucinda Bateman | last4 = Bested | first4 = Alison C | authorlink4 = Alison Bested | last5 = Davenport | first5 = Todd | authorlink5 = Todd Davenport | last6 = Friedman | first6 = Kenneth J | authorlink6 = Kenneth Friedman | last7 = Gurwitt | first7 = Alan R | authorlink7 = Alan Gurwitt | last8 = Jason | first8 = Leonard A | authorlink8 = Leonard Jason | last9 = Lapp | first9 = Charles W | authorlink9 = Charles Lapp | last10 = Stevens | first10 = Staci R | authorlink10 = Staci Stevens | last11 = Underhill | first11 = Rosemary A | authorlink11 = Rosemary Underhill | last12 = Vallings | first12 = Rosamund | authorlink12= Rosamund Vallings | date = 2014 | url=https://www.massmecfs.org/images/pdf/Primer_2014.pdf | title =Chronic Fatigue Syndrome Myalgic Encephalomyelitis Primer for Clinical Practitioners }}</ref> | ||
| date | <ref name="IOM2015MECFS">{{Cite web | last1 = Institute of Medicine (US) | title = Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness| publisher = The National Academies Press | location = Washington, DC, US| date = Feb 10, 2015 | isbn = 978-0-309-31689-7| url = https://pubmed.ncbi.nlm.nih.gov/25695122/}}</ref> | ||
| url | <ref name="Jason, Katz, 2017">{{Cite journal | last1 = Jason | first1 = Leonard A | authorlink1 = Leonard Jason | last2 = Katz | first2 = Ben | authorlink2 = Ben Katz | last3 = Gleason | first3 = Kristen | authorlink3 = | last4 = McManimen | first4 = Stephanie | authorlink4 = Stephanie McManimen | last5 = Sunnquist | first5 = Madison | authorlink5 = Madison Sunnquist | last6 = Thorpe | first6 = Taylor | authorlink6 = | title = A Prospective Study of Infectious Mononucleosis in College Students | journal = International Journal of Psychiatry | volume = 2 | issue = 1 | page = | date = 2017| doi = | url = https://www.researchgate.net/profile/Leonard_Jason/publication/312936696_A_prospective_study_of_Infectious_Mononucleosis_in_college_students/links/588a23cc92851c2779b2568c/A-prospective-study-of-Infectious-Mononucleosis-in-college-students.pdf }}</ref> | ||
}}</ref> | <ref name="Klimas20140621video">{{Cite web | last1 = Klimas | first1 = Nancy | authorlink1 = Nancy Klimas | title = ME/CFS Diagnosis and Name with Dr. Nancy Klimas (video)| date = Jun 21, 2014 | url = http://youtu.be/c2vIQ92wU9Y}}</ref> | ||
<ref name="Komaroff20160217video">{{citation | last1 = Komaroff | first1 = Anthony | authorlink1 = Anthony Komaroff | last2 = Iskander | first2 = John | authorlink2 = John Iskander | title = Interview with Dr Anthony Komaroff | journal = CDC Public Health Ground Rounds - Beyond the Data - Chronic Fatigue Syndrome: Advancing Research and Clinical Education | date = Feb 17, 2016 | url = https://youtu.be/hRdn4A2SGic}}</ref> | |||
<ref name="MEACTIONpacepetition">{{Cite web | last1 = #MEAction | authorlink1 = #MEAction | title = Petition: Misleading Claims Should Be Retracted| website = #MEAction | date = Oct 2015 | url = http://my.meaction.net/petitions/pace-trial-needs-review-now}}</ref> | |||
<ref name="MEACTION20160313openletr">{{Cite web | last1 = #MEAction | authorlink1 = #MEAction | title = 24 organisations in 14 countries tell QMUL: Release the PACE data | date = Mar 13, 2016| url = http://www.meaction.net/2016/03/13/24-organisations-in-14-countries-tell-qmul-release-pace-data/#comment-2518}}</ref> | |||
<ref name="MEASSUK20150529survey">{{Cite web | last1 = ME Association (UK) | authorlink1 = ME Association | date = May 29, 2015 | title = Our CBT, GET and Pacing Report calls for major changes to therapies offered for ME/CFS| url = http://www.meassociation.org.uk/2015/05/23959/ }}</ref> | |||
<ref name="NakatomiY2014">{{Cite journal | last1 = Nakatomi | first1 = Yasuhito | authorlink1 = Yasuhito Nakatomi | last2 = Mizuno | first2 = Kei | authorlink2 = Kei Mizuno | last3 = Ishii | first3 = Ishii | authorlink3 = Akira Ishii | last4 = Yasuhiro | first4 = Wada | authorlink4 = Yasuhiro Wada | last5 = Masaaki | first5 = Tanaka | authorlink5 = Masaaki Tanaka | last6 = Shusaku | first6 = Tazawa | authorlink6 = Shusaku Tazawa | last7 = Kayo | first7 = Onoe | authorlink7 = Kayo Onoe | last8 = Sanae | first8 = Fukuda | authorlink8 = Sanae Fukuda | last9 = Joji | first9 = Kawabe | authorlink9 = Joji Kawabe | last10 = Kazuhiro | first10 = Takahashi | authorlink10 = Kazuhiro Takahashi | last11 = Yosky | first11 = Kataoka | authorlink11 = Yosky Kataoka | last12 = Susumu | first12 = Shiomi | authorlink12= Susumu Shiomi | last13 = Kouzi | first13 = Yamaguti | authorlink13 = Kouzi Yamaguti | last14 = Masaaki | first14 = Inaba | authorlink14 = Masaaki Inaba | last15 = Hirohiko | first15 = Kuratsune | authorlink15 = Hirohiko Kuratsune | last16 = Yasuyoshi | first16 = Watanabe | authorlink16 = Yasuyoshi Watanabe | title = Neuroinflammation in Patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: An ¹¹C-(R)-PK11195 PET Study| journal = Journal of Nuclear Medicine | volume = 55 | issue =6 | page = 945-50 | date = Mar 24, 2014 | pmid = 24665088 | doi = 10.2967/jnumed.113.131045| url = http://jnm.snmjournals.org/content/55/6/945.long}}</ref> | |||
<ref name="NIHP2PFIN">{{citation | author = National Institutes of Health (US)| title = NIH Pathways to Prevention Workshop: Advancing the Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | date = Dec 9, 2014| url = https://prevention.nih.gov/docs/programs/mecfs/ODP-P2P-MECFS-FinalReport.pdf}}</ref> | |||
<ref name="viroblogMECFS">{{ | <ref name="Phoenix20160222Norway2012">{{Citation | title = Norwegian patient survey: Experiences of therapeutic approaches (2012) | journal = Phoenix Rising Forum | date = Feb 22, 2016| url = http://forums.phoenixrising.me/index.php?threads/norwegian-patient-survey-experiences-of-therapeutic-approaches-2012-update.43193/ }}</ref> | ||
| title | <ref name="viroblogMECFS">{{Cite web | title = List of ME/CFS articles published at Virology Blog| url = http://www.virology.ws/mecfs/ }}</ref> | ||
| url | <ref name="DerekPrisk2009">{{Cite journal | last1 = Pheby | first1 = D | authorlink1 = Derek Pheby | last2 = Saffron | first2 = L | authorlink2 = | title = Risk factors for severe ME/CFS | journal = Biology and Medicine | volume = 1 | issue = 4 | date = 2009 | ||
}}</ref> | | eissn = 09748369 | doi = | url = http://biolmedonline.com/Articles/vol1_4_50-74.pdf}}</ref> | ||
</references> | </references> | ||
[[Category:Primers]] | [[Category:Primers]] | ||
Latest revision as of 22:19, November 17, 2023
Editors: Edits to this Primer may require the same edits to the other Primers. |
Myalgic encephalomyelitis (ME), chronic fatigue syndrome (CFS), and chronic fatigue (CF) are widely misunderstood. In this Primer for journalists, we provide evidence-based statements (with links to further reading & sources) to support journalists writing about the disease. Chronic Fatigue Syndrome must never be shortened to Chronic Fatigue in the body of an article or its headline. This has caused much confusion for readers who do not understand CFS is a debilitating lifelong illness and it is not the same as chronic fatigue (CF); CF is a symptom of many different illnesses. Although the Fukuda[1] and the Oxford Criteria[2] are used for diagnosing CFS, they are both overly broad and there is criticism that patients are being misdiagnosed in both clinical and research settings as having CFS when in fact they are suffering from the symptom CF or another fatiguing diagnosis.[3][4][5][6][1][7][8]
There have been media reports of athletes diagnosed with ME or CFS who have recovered in a relatively short period of time after rest, supplementation, and diet changes;[9][10][11][12] these athletes may have had overtraining syndrome (which has the symptom of chronic fatigue) and not ME or CFS,[13] while people with adrenal failure, idiopathic chronic fatigue or other fatiguing illnesses may be erroneously diagnosed with CFS.[14][15][16] ME and CFS in professional athletes is normally a career-ending diagnosis.[17][18][19][20][21][22][23]
The core ME/CFS symptoms are: chronic fatigue (CF); post-exertional malaise (PEM); unrefreshing sleep/sleep problems; and cognitive impairment/brain fog and/or orthostatic intolerance (OI).[24][25]:9-10 A patient can have many more symptoms[26] and meet different criteria. Systemic Exertion Intolerance Disease (SEID), an ME/CFS criterion, allows for a patient to be diagnosed with the minimum core symptoms[27] and the patient may have other symptoms.[28] The Canadian Consensus Criteria (CCC) requires the core symptoms and neurological, autonomic, neuroendocrine, immune system, and myalgia symptoms to meet its ME/CFS diagnostic criteria.[4] The International Consensus Criteria (ICC) is used to diagnose myalgic encephalomyelitis (ME) which requires the core symptoms and neurological, immune/gastrointestinal/genitourinary impairment, and energy metabolism/ion transport impairment symptoms for a diagnosis.[16]
The acronym ME/CFS is widely used in research, by clinicians, patient organizations, and patients.
"The most common overlapping condition with ME/CFS is fibromyalgia."[5][29][30] While some have posited ME/CFS and fibromyalgia are variants of the same illness, Benjamin Natelson, MD summoned considerable amounts of data that suggest the two illnesses differ with different pathophysiologic processes leading to different treatments.[31]
Unfortunately, a psychiatric approach has been taken with ME/CFS, but this is changing. At this time there are no approved drug treatments. Graded exercise therapy (GET) and cognitive behavioral therapy (CBT) are used in the UK inappropriately for treating ME/CFS. The Centers for Disease Control and Prevention (CDC) website states "ME/CFS is a biological illness, not a psychologic disorder" and impacts multiple body systems.[32] The CDC recognizes the hallmark symptom of PEM which is a worsening of symptoms after physical, mental or emotional exertion[24] and says ME/CFS is a "disabling and complex disease."[33]
What do we know?[edit | edit source]
ME is a debilitating illness that has been recognized as a neurological disease by the World Health Organization (WHO) since 1969.[34]
It is a systemic neuroimmune disease characterized by post-exertional malaise (PEM) (a severe worsening of symptoms after even minimal exertion). It causes dysregulation of both the immune system and the nervous system. The effects of ME are devastating enough to leave 25% of patients housebound or bedbound. For moderate to severe patients, the disability of living with ME is like living with late-stage cancer, advanced stage AIDS, or congestive heart failure for decades.
In many parts of the world, it is commonly called chronic fatigue syndrome.
ME/CFS costs the US economy up to $24 billion per year in direct medical costs, and lost production.[35] Despite this, funding for research is not commensurate with the level of disease burden. In the 2015 financial year, the National Institutes of Health (NIH) provided only $5 million in research funding for ME/CFS, which is less funding than hayfever. This is in stark contrast to funding levels for other similarly disabling illnesses, like multiple sclerosis ($105 million) and HIV/AIDS ($3 billion).[citation needed] The Institute of Medicine, a special advisory committee of the U.S. Department of Health and Human Services (HHS) (ref: CFSAC recommendations) and NIH expert advisory panel agree that it is imperative to increase research funding into ME/CFS.[36]
Disease onset and course of illness[edit | edit source]
ME/CFS can begin from many acute/sudden[37] events: usually viral or bacterial infections, but also trauma, surgery or childbirth, allergic reaction, and stress.[38] There is also a gradual onset in some people,[37][39] that is not attributed to any one event. Occasionally, ME/CFS has been triggered by environmental toxins or the receipt of an immunizing injection.[40] Some say that the disease ME always has an acute/sudden infectious onset.[41]
The disease ME/CFS is often diagnosed when a person does not recover from a flu-like illness, mononucleosis or another herpesvirus, Q fever, an unidentified virus, or other infection, and meets one or more diagnostic criteria for either ME, CFS, or ME/CFS.[28]:157-158[42] Patients experience numerous symptoms and disease severity which fluctuate from day to day, week to week, month to month, year to year, and even decade to decade. Furthermore, symptoms and disease severity vary among patients.[29][43]
The CDC recognizes that there can be different causes and it is possible that two or more things could cause the illness. Areas of research include infections, immune system changes, physical or psychological stress affecting body chemistry, changes in energy production, and a possible genetic link.[44][32] The CDC notes there are abnormalities with the immune system, cellular metabolism, neuroendocrine disturbances, and blood pressure or heart rate regulation.[32]
Not a mental health disorder[edit | edit source]
In the past, CFS was believed to be a mental health disorder. This is why the CDC now states: "ME/CFS is a biological illness, not a psychologic disorder. Patients with ME/CFS are neither malingering nor seeking secondary gain. These patients have multiple pathophysiological changes that affect multiple systems."[32]
No clear evidence that ME/CFS is contagious[edit | edit source]
Infectious episodes have led to outbreaks over the years and 72% of ME/CFS patients report an onset of a viral or bacterial infection.[45] Nowadays, the vast majority of ME/CFS cases are sporadic rather than epidemic - although some outbreaks have been caused by known viruses such as the SARS pandemic and COVID-19 - there is no clear evidence that sporadic ME/CFS cases are contagious.[46]
Families, partners, and friends do not report contracting ME/CFS from someone with the disease nor do patients report passing it on to others.[47] However, Underhill and O'Gorman (2006) researched 219 patients with ME/CFS, and concluded that close household contact and genetics were both risk factors for CFS, finding 3.2% of spouses/partners of those with CFS also had the illness.[48] This was a higher prevalence than all genetic relatives except children of patients. Because ME/CFS can run in families, a genetic link is a line of research recommended by the CDC.[44]
Michael Sikora and collaborators at the Open Medicine Foundation hope that their research on the role of T cells and immune-related genes will help address "whether ME/CFS is an autoimmune or infectious disease, or simply an activation of the immune system".[49]
Blood donation and organ transplant[edit | edit source]
A tissue and blood donation ban is in force for ME/CFS in the United Kingdom (even if recovered),[50] Australia,[51] New Zealand,[52] most of Canada,[53] and for a time also in the United States,[54] initially due to the research on XMRV as being the likely infectious trigger of CFS[55] and showing that patients carried the virus.[54] Two papers on XMRV were retracted as the result was caused by laboratory contamination,[56][57] but many blood donation bans remain.[53]
The US American Red Cross no longer has statements barring transfusions or transplants for CFS,[58] but patients are expected to be in "good health" which would exclude most.[58] The American Association of Blood Banks advises to either accept or defer ME/CFS donors based on "clinical judgment of the donor's health status".[59] Patient charities discourage ME/CFS patients from donating blood,[60]
Mini-Docs[edit | edit source]
What happens when you have a disease doctors can't diagnose By Jen Brea/TED
Five years ago, TED Fellow Jen Brea became progressively ill with myalgic encephalomyelitis, commonly known as chronic fatigue syndrome, a debilitating illness that severely impairs normal activities and on bad days makes even the rustling of bed sheets unbearable. In this poignant talk, Brea describes the obstacles she's encountered in seeking treatment for her illness, whose root causes and physical effects we don't fully understand, as well as her mission to document through film the lives of patients that medicine struggles to treat.[61][62]
Invisible Illness - Stories of Chronic Fatigue Syndrome By Veronica Weber/Palo Alto Online
This mini documentary reveals 3 stories of people who have been impacted by Chronic Fatigue Syndrome - a little known disease that affects roughly 836,000-2.5 million people in the U.S. and receives little research funding. They share emotions of treating loved ones with the disease, their frustrations of being ignored by members of society and the healthcare industry and express hopes of treatment and research. Video by Veronica Weber/Palo Alto Online[63]
Diagnosis and Management of Myalgic Encephalomyelitis and Chronic Fatigue Syndrome By Dr. David Kaufman/Unrest
This video on the diagnosis and management of myalgic encephalomyelitis and chronic fatigue syndrome is part of the Unrest Continuing Education module, made available through the American Medical Women’s Association and Indiana University School of Medicine, and in partnership with #MEAction. US medical providers can visit: https://www.unrest.film/cme to register to watch Unrest online for free and receive Continuing Education credit.[64]
Epidemiology[edit | edit source]
In the United States, 836,000 - 2.5 million people suffer from ME/CFS. "The total economic costs of ME/CFS are estimated at $17 to $24 billion annually."[25] Some CFS patients can work with job accommodations but 1/3 to 1/2 become unemployed and many rely on SSDI/SSI.[65]
- All races and cultures are afflicted with ME/CFS.[66][67] Children and adolescents are also diagnosed.[68][69]
- Like many autoimmune and neuro-immune diseases where mostly women are afflicted,[70] the ME/CFS female/male patient ratio per Capelli et al. is 6:1[71] while the CDC states 4:1.[67]
- Pediatric ME/CFS is defined by the CDC[72] and the National Academy of Medicine (NAM)[28]:181 although it is usually diagnosed in adults.[33] "Children below the age of 8 or 9 do not have the symptom pattern of adolescents past puberty. If the onset of the disease occurs during adolescence, the most common time of onset, the pattern is similar to that of adults."[73] The prognosis in adolescents is considered to be better than in adults.[74][75] Children are diagnosed with ME/CFS at three months of illness under SEID and CCC and ME is diagnosed immediately under ICC.[76][25][4][16]
- "Worldwide, there may be as many as 17 – 24 million people with ME/CFS."[77] 25% of ME/CFS patients are housebound or bedbound at some point in their illness.[78][28]:32 90% of patients are undiagnosed.[33]
- The prognosis for a patient diagnosed with ME/CFS is considered to be poor with only a minority (a median estimate of 5%) returning to pre-morbid levels of functioning.[79] The majority of patients remains significantly impaired. A substantial improvement however is noted in an estimated 40% of patients.[79][80]
ME vs CFS vs CF[edit | edit source]
The name myalgic encephalomyelitis (ME) was coined following an outbreak of an illness at the Royal Free Hospital in the UK, in 1955. The name chronic fatigue syndrome (CFS) was coined by the Centers for Disease Control and Prevention (CDC) following an outbreak of a flu-like illness at Incline Village, at Lake Tahoe, in the 1980s. There is disagreement as to whether ME and CFS are the same disease, entirely separate illnesses, or whether ME constitutes a more severe subset of CFS. Adding to the confusion, the diagnostic name given to patients is more often dependent on the country in which they live, than differing characteristics of their illness, as some countries use CFS (eg: US, Australia), and other countries (particularly in Europe) use ME. At this point in time, there is no clear biological evidence to resolve whether the illnesses are the same or different, and there is unlikely to be a resolution until firm biomarkers have been identified. As such, many patients and researchers use the term ME/CFS.[81] See: Definitions of ME and CFS.
The name Chronic Fatigue Syndrome is itself controversial, as many consider it stigmatizing. In February 2016, Dr Anthony Komaroff, who was part of the CDC group of clinicians who coined the name Chronic Fatigue Syndrome, said of it:
"I think that was a big mistake because the name, in my opinion, and the opinion of a lot of people, it both trivializes and stigmatizes the illness. It makes it seem unimportant, maybe not even real"[82]
It is important to distinguish between ME/CFS and chronic fatigue (CF), which is a symptom of many different medical conditions (e.g.: anemia, hepatitis, multiple sclerosis, hypothyroidism, depression, ME/CFS). "Chronic fatigue" is not an illness in its own right and it is incorrect and misleading to refer to ME/CFS as "chronic fatigue". While fatigue is a component of ME/CFS, many consider post-exertional malaise (PEM) to be the cardinal feature of ME/CFS.[4][35]
Evidence of a disease[edit | edit source]
Symptoms[edit | edit source]
Symptom presentation varies enormously between individuals. Symptom presentation also varies within individuals, as individuals often report that symptoms change over time (increasing or decreasing) and new symptoms may appear while others disappear.[83] There are many symptoms which people with ME/CFS experience, though those listed below are the core symptoms found in all patients.






- Post-exertional malaise (PEM) is the hallmark symptom of ME/CFS. After physical, mental or emotional exertion (which for some patients can be a shower or making out a to-do list, others grocery shopping, socializing or reading a news article, while some just walking to the mailbox, getting to the doctor or mentally following a T.V. program)[26][24][79] there is a payback of significant worsening ME/CFS symptoms which can be delayed for 24-72 hours or more[24][87][88] and can last 24 hours and even days, weeks, or months.[89][90] The patient will experience even greater fatigue as well as exasperate the flu-like symptoms and body pain. Every patient experiences different symptoms and symptom severity from different activities and exertion output according to how sick he or she is with the disease.[74][26][79] Regarding PEM the CFIDS Association of America states:
This is a term which describes a symptom in which exercise or exertion can bring on malaise (illness). In the case of people with ME/CFS, malaise often occurs during a period some 24-72 hours after exertion. For example, in some cases, a short walk can worsen ME/CFS symptoms two days later. This lack of understanding about the delayed onset of symptoms has, in the past, made it harder to test for ME/CFS. Follow up tests, taken less than 24 hours after an initial exercise test, may show that the patient can still perform activities at the same level (before post exertional malaise has a chance to take hold).[91]
- orthostatic intolerance (OI) such as postural orthostatic tachycardia syndrome (POTS) or neurally mediated hypotension (NMH)
- unrefreshing sleep/sleep disturbance [27][25]
Other possible symptoms[edit | edit source]
- chronic pain
- immune system
- neurological signs and symptoms See also: neuroinflammation.
- List of symptoms in ME/CFS
Comorbids[edit | edit source]
- fibromyalgia (FMS)
- irritable bowel syndrome (IBS)
- multiple chemical sensitivity (MCS)
- temporomandibular joint disorder (TMJ) [92]
Government guides on symptoms[edit | edit source]
US Government guides on symptoms
Canada guides on symptoms
Biological abnormalities[edit | edit source]
Because there is currently no biomedical test for ME/CFS, many have incorrectly assumed that there are no medical abnormalities found in people with the illness. As a result, ME/CFS symptoms are often considered to be medically unexplained, and therefore psychological in origin. While it is true that the illness is poorly understood, many biological abnormalities have been found in a range of different body systems, particularly in the central nervous system, autonomic nervous system, immune system, and energy metabolism.[35] Unfortunately, none have yet proved to be specific enough to ME/CFS as to be useful as a biomarker of the disease, and many were identified in small studies, which need replication. Whilst there have been many abnormalities identified found to be associated with the disease, it cannot yet be determined whether these are a cause or consequence.
Notable studies[edit | edit source]
- Cytokine ("Notable studies")
- Immune findings by Mady Hornig & Ian Lipkin[93]
- List of enterovirus infection studies
- 2014, Neuroinflammation Japanese Neuroinflammation study[94]
- 2015, Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: Evidence of inflammatory pathology[95] - (Full text)
- Younger's Leptin study
- 2014, Right Arcuate Fasciculus Abnormality in Chronic Fatigue Syndrome[96]
Bilateral white matter atrophy is present in CFS. No differences in perfusion were noted. Right hemispheric increased FA may reflect degeneration of crossing fibers or strengthening of short-range fibers. Right anterior arcuate FA may serve as a biomarker for CFS.
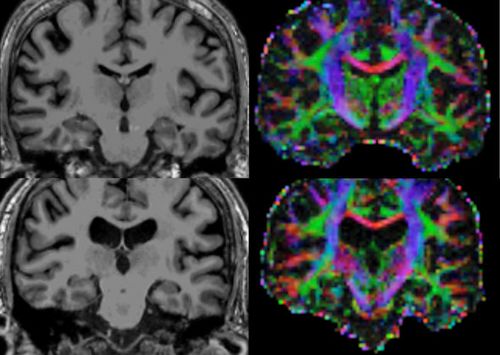
- 2019, Evidence of widespread metabolite abnormalities in Myalgic encephalomyelitis/chronic fatigue syndrome: assessment with whole-brain magnetic resonance spectroscopy[97]
Causes & triggers[edit | edit source]
- Outbreaks - see List of outbreaks
- Possible infectious triggers: Enteroviruses, Epstein-Barr virus[99], Q fever[99], Ross River virus[99], mononucleosis[100], (Ebola?)[99]
- Non-viral triggers - trauma, chemical
Tests[edit | edit source]
- Natural killer cell (NKC) Blood Test
- Sleep study for sleep apnea, restless leg syndrome, and other sleep disturbances.
- Tilt table test for OI or POTS.
Treatments[edit | edit source]
There are currently no Food and Drug Administration (FDA) approved treatments for ME/CFS. Treatments consist mostly of symptom management, rather than treatment of the underlying cause of the disease, which is not yet understood.[29] There are many potential treatments, though their evidence-base is limited, as most research into treatments has gone into psychological approaches to treatment.
Drugs[edit | edit source]
Two treatments that have garnered much attention are Ampligen, produced by AIM ImmunoTech (formerly Hemispherx Biopharma), and Rituximab. Many people have reported improvements from Ampligen, and a few recovered but relapsed when they stopped taking it.[101]
Attempts to obtain FDA approval for Ampligen in the US have failed, but it is available to some people on compassionate use.[102] Argentina approved the use of Ampligen for severe ME/CFS in 2016.[103][104] Also in 2016, it was made available on a limited basis in Europe.[105] In July 2018, AIM ImmunoTech announced the expansion of its US compassionate use program, AMP-511, to new ME/CFS patients for the first time in over a year.[106][107]
Rituximab, a lymphoma drug, had shown promising results in initial trials in Norway,[108] and there were groups crowdsourcing funding for further trials in other countries. In 2017, Drs. Øystein Fluge and Olav Mella announced that their Rituximab trial had failed. They stated that they would focus their efforts on attempting to identify a subgroup of ME/CFS patients with an immune profile that would be responsive to Rituximab.[109] A phase III trial published in 2019 showed Rituximab does not improve ME/CFS.[110]
Jarred Younger announced in March 2016 that he will be undertaking a trial of low dose naltrexone (LDN) in ME/CFS.[111]
Treating other conditions[edit | edit source]
Different forms of OI are treated with beta-blockers (Metopropol), Fludrocortisone (Florinef), and Pyridostigmine.[4] When treating other diseases, illnesses, and conditions, and ME/CFS comorbidities or overlapping conditions such as sleep difficulties, cognitive problems, pain, and other symptoms it is important to remember that patients are sensitive to medications.[112] The CDC advice to health care practitioners is to be aware that because all drugs can cause side effects, ME/CFS patient symptoms can worsen. "This is particularly true of any medication that acts on the central nervous system, such as sedating medications: therapeutic benefits can often be achieved at lower-than-standard doses. Patients with ME/CFS might tolerate or need only a fraction of the usual recommended doses for medications. After initial management with lower dosing, one or more gradual increases may be considered as necessary and as tolerated by the patient."[74] For instance, tricyclic drugs can improve mood and help with sleep and pain. However, in some in can worsen OI.[74]
Exercise as treatment[edit | edit source]

.
Previously, two common treatment recommendations for ME/CFS were graded exercise therapy (GET) and cognitive behavioral therapy (CBT). These treatments are based on disproven the hypothesis that the disease might have begun with a viral infection but has been perpetuated by deconditioning from lack of activity, and fear and avoidance of activity. GET and CBT are aimed at addressing these hypothesized causes by challenging the proposed unhelpful thoughts that result in avoidance of activity and reconditioning through a gradual increase in exercise. These treatments are controversial and are at odds with much of the research literature, which suggests that exercise is harmful to people with ME/CFS. A large patient survey of treatment responses found that 74% of people who had tried GET, reported that their symptoms subsequently worsened,[113] which is consistent with other patient surveys and many research findings.[114][115]
The PACE trial, published in 2011, is the largest GET trial ever conducted. It has received much publicity as a result of its recovery rate claims, though it has come under strong criticism from within both the scientific and patient community for significant flaws in its design, and for overstating (and in some cases misrepresenting) outcomes in both the initial trial, and follow-up studies.[116] From 2015 to present day, the study was the subject of a series of investigative pieces that were highly critical of the trial by journalist Dr. David Tuller[117], science writer Julie Rehmeyer, patient advocate Tom Kindlon, Dr. Keith Geraghty[118], psychologist Carolyn Wilshire[119] and others. A petition signed by almost 12,000 ME/CFS patients and allies,[120] and an open letter signed by 42 ME/CFS experts from around the world,[121] were sent to The Lancet, both calling for the data to be reanalysed. Twenty-four ME/CFS organizations from 14 different countries have written to Queen Mary University London requesting that the trial data be released for reanalysis.[122] To date, the authors of the trial and editor of The Lancet have refused such requests. Despite such criticism, the PACE trial continues to influence both government and the medical profession's approach to the treatment of ME/CFS in many countries.
One of the reasons that exercise may be harmful to people with ME/CFS, is the presence of post-exertional malaise (PEM), which is an exacerbation of symptoms following physical, mental or even emotional exertion. Studies have revealed immunological, muscular, neurological, autonomic and cardiovascular abnormalities in response to exercise in people with ME/CFS. As these results are not also found in healthy sedentary controls, the adverse effects of exercise cannot be said to be due to deconditioning.[123][citation needed][citation needed]
People with ME/CFS should approach exercise with caution, as there is much evidence of potential for harm.[115][5]
Anaerobic threshold, use of heart rate monitors for activity and pacing. Analeptic, not aerobic. Energy envelope/pacing - people do better if stay within their envelope, than push to increase activity
Graded exercise therapy & Cognitive behavioral therapy[edit | edit source]

.
GET and CBT have been recently abandoned in the UK, Ireland and many parts of Europe by ME Clinics.[124] They are highly controversial and not recommended by patients, most patient advocates, and research organizations nor by many doctors or researchers outside of the UK. Based on the flawed PACE trial which used the flawed Oxford criteria to diagnose and recruit patients, GET and CBT found its way into treating people with ME/CFS.
Exercise, especially GET, can harm an ME/CFS patient further.[115]
- Jennifer Brea walked home from her Neurologist's office and became wheelchair-bound.
- This is an experience of serious harm due to GET shared by K. Miles, via Tom Kindlon on Twitter.
- Emma Shorter was able to walk a few minutes a day until GET put her in a wheelchair.
- Dr Maik Speedy was also seriously injured by GET and has been bedbound since.
- British MP Brynmor John collapsed outside the House of Commons gym in 1998 and died, as a result of following his doctor's advice to exercise back to health.
Claims of recovery and cures[edit | edit source]
Charlatans claim they can cure CFS (per the CDC "there is no cure"[125]) when in reality they may be able to treat chronic fatigue (CF). ME/CFS patients experience an ongoing improper immune response and other abnormalities for at least 6 months straight with a reduction in activity with a specific symptom set for at least 50% of the time.[32][126][127]
Additionally, there have been media reports of some athletes―usually amateur athletes,―diagnosed with CFS that recovered after a relatively short period of time with rest, supplementation, and diet changes,[9][10][11][12] but they may have had overtraining syndrome,[13] while some people with adrenal failure, idiopathic chronic fatigue or another fatiguing illness may be erroneously diagnosed with CFS[16][14][15] ME and CFS in professional athletes normally results in very premature retirement.[17][18][19][20][21][22][23]
Severely ill patients[edit | edit source]
Considerable variation exists in the severity of the disease. The International Consensus Criteria lists the following severity levels (it should be noted that even "mild" ME/CFS consists of significant debility):
- Mild = 50% reduction in pre-illness activity levels
- Moderate = mostly housebound
- Severe = mostly bedridden
- Very Severe = totally bedridden, and needing help with basic functions.
At least 25% of people with ME/CFS are bedbound or housebound, often for years or even decades, so are largely an invisible population.[35][128][129] So invisible in fact, that they have rarely been included as part of research because their level of debility precludes them from traveling to laboratories for required testing. The Open Medicine Foundation's ME/CFS Severely Ill, Big Data Study will be the first in-depth study of people with a severe form of ME/CFS. This study has so far produced the groundbreaking paper Metabolic features of chronic fatigue syndrome. It is estimated that 25% of ME/CFS patients are severely ill and are housebound or bedbound.
Notable patients with severe or very severe ME/CFS include Whitney Dafoe, Karina Hansen, Lynn Gilderdale, Laura Hillenbrand, Tom Kindlon, Vanessa Li, Doctor Speedy, Naomi Whittingham, Jamison Hill and Jessica Taylor-Bearman.
Though uncommon, there have been instances of deaths which have been attributed to the disease (see Sophia Mirza, Merryn Crofts). National Statistics report an average of 10 - 12 deaths per year in England and Wales partly or fully caused by ME/CFS, with almost all patients dying being of working age. [130]
Patients and psychiatry/psychology[edit | edit source]
- Objections and scope
- Mind-body dualism
- Psychologization
- Cognitive behavioral therapy
- The PACE trial. See Patient view of the PACE Trial controversy
- Ethical issues
- Patient mental health
Stigmatization[edit | edit source]
- Pretty young women slumped on desk
- Yuppie Flu
- Accusations of laziness/lethargy
- Epidemiological evidence - age, gender, demographic, racial/cultural
- Stigma and discrimination
Accusations of harassment[edit | edit source]
- No arrests or convictions[131]
- Potential harassment and "wild speculations" about threats to researchers were unsuccessful arguments used in Queen Mary University of London's failed attempt to deny access to the PACE trial data at the 2015 tribunal. The tribunal judgement stated that the only evidence of harassment provided was a single heckler in a single seminar.[132]
- Mistreatment of patients, including forced harmful treatment of children, is not mentioned. E.g., the story of "B", aged 8,[133] and Ean Proctor and others "The Mental Health Movement: Persecution of Patients?"[134]
- A pattern of intimidation and bullying of PACE trial critics has included targeting scientists' employers, professional bodies, politicians including the Countess of Mar, and smear tactics in the national press.
Working with government to move forward[edit | edit source]
Advocates met with senate staffers the week of March 16, 2016, and discussed research and drug development by the NIH, the CDC reinstating and increasing funding and education based on IOM recommendations and the HHS funding to develop Centers of Excellence.[135] The MEAction Network reports on this ongoing process.
CDC Website updates[edit | edit source]
- Jul 3, 2017, the CDC's Chronic Fatigue Syndrome page has been changed to Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) and GET and CBT recommendations have been removed.[136][137]
- Jul 12, 2018, the "Information for Healthcare Providers" tab and its sub-tabs were updated.[138][139]
- Feb 25, 2019, Dr. Elizabeth Unger, Chief of CDC's Chronic Viral Disease Branch (CVDB), that houses the ME/CFS program, in collaboration between Medscape and the CDC put out brief video and commentary page with links to the CDC's July 12th, 2018 updates for medical professionals: Chronic Fatigue Syndrome: It's Real, and We Can Do Better.[140]
MEAction input
- Jul 29, 2018, CDC Revises its Information on ME #MEAction report on the CDC July 2017 and July 2018 website updates. Recommendations for the CDC's ME/CFS page have been created from patient feedback on the updates as well as asking for further patient input.
Expert opinions[edit | edit source]
Quotes from ME/CFS experts and patients[edit | edit source]
Doctors[edit | edit source]
UK
US
Researchers[edit | edit source]
Australia
UK
US
Patients[edit | edit source]
Australia[edit | edit source]
Canada[edit | edit source]
Scotland[edit | edit source]
US[edit | edit source]
UK[edit | edit source]
Ireland[edit | edit source]
Patient groups & charities[edit | edit source]
Photos[edit | edit source]
- Stock photographs suitable for ME/CFS articles - curated by Phoenix Rising
- Advice on photograph choice
History[edit | edit source]
- Osler's Web is a book by Hillary Johnson on the early history of CFS.
- Thirty Years of Disdain by Mary Dimmock and Matthew Lazell-Fairman picks up on the ME/CFS history where Osler's Web leaves off.
Deaths of ME/CFS patients[edit | edit source]
Death certificates with ME or CFS
- Merryn Crofts' death is attributed to ME.
- Sophia Mirza's death is attributed to CFS.
In the UK, United States, and Australia there are further reports of loved ones who have died due to ME/CFS.[141] See Editor's Note[142]
Other tips and articles for journalists[edit | edit source]
- 2021, How to Report with Accuracy and Sensitivity on Contested Illnesses - by ME/CFS patient and science writer Julie Rehmeyer, Open Notebook
- Always interview a patient
- Interview more than one researcher (not just from the psychological etiology view)
- Avoid using derogatory, outdated & incorrect term "Yuppie Flu"
- Never shorten the disease name chronic fatigue syndrome (CFS) to the symptom chronic fatigue (CF). CFS, ME or ME/CFS can be used to save print space.
- Use photographic imagery that represents the reality for patients - serious illness & disability - not well-groomed & slightly tired office workers at their computer or students with a pile of books sleeping at their desk. Solve ME/CFS Initiative's Times Square Public Awareness Ad shows the reality of the disease ME/CFS. Using photos of patients whether chronically ill yet functioning or a severely ill patient or stock photos that reflect life with this disease is necessary.
Learn more[edit | edit source]
Key facts
- Key Facts - Institute of Medicine (2015)
Research
- Institute of Medicine report (2015) The CDC based its updated ME/CFS page on information in this report.
- Notable studies
Films
- Forgotten Plague is a US documentary about Ryan Prior, an afflicted journalist who investigates the disease and its history and why the CDC has left millions sidelined from life; available for streaming and DVD purchase. (2015)
- Unrest is a US documentary film that aired on PBS's Independent Lens in 2018 and is available for streaming and DVD purchase. Jennifer Brea, a person with ME, directs. (2017)
ME/CFS organization and researchers material
- Beyond the Data – Chronic Fatigue Syndrome: Advancing Research and Clinical Education (The CDC's Dr. John Iskander interviews Dr. Anthony Komaroff. Video, 2016)
- Caring for People with Myalgic Encephalomyelitis (2018) Guide for Caretakers
- ME/CFS Diagnosis and Name with Dr Nancy Klimas (video)
- What is ME/CFS? By the Open Medicine Foundation
- Patients that had been deemed as suffering from mental health and not a biological illness:
- Karina Hansen is a young Danish woman taken from her family for 3 1/2 years due to Per Fink's insistence her ME was due to mental health issues.
- Sophia Mirza was taken forcibly from her home to a mental hospital only to be returned shortly after; she then died of ME.
- Ean Proctor was taken from his parents as a young boy and he was told his "parents were letting him die." He had become paralyzed and mute and was let go in the deep end of a pool to make him swim and another time put him on a scary theme park ride to scare him into moving.
More mental health information
- ME/CFS is not depression. It causes a lack of energy, not a lack of desire.[143][144][145]
See also[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Fukuda, K.; Straus, S.E.; Hickie, I.; Sharpe, M.C.; Dobbins, J.G.; Komaroff, A. (December 15, 1994). "The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group" (PDF). Annals of Internal Medicine. American College of Physicians. 121 (12): 953–959. doi:10.7326/0003-4819-121-12-199412150-00009. ISSN 0003-4819. PMID 7978722.
- ↑ Sharpe, MC; Archard, LC; Banatvala, JE; Borysiewicz, LK; Clare, AW; David, A; Edwards, RH; Hawton, KE; Lambert, HP (February 1991). "A report--chronic fatigue syndrome: guidelines for research". Journal of the Royal Society of Medicine. 84 (2): 118–121. ISSN 0141-0768. PMC 1293107. PMID 1999813.
- ↑ Vink, Mark; Vink-Niese, Alexandra (September 20, 2019). "Work Rehabilitation and Medical Retirement for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. A Review and Appraisal of Diagnostic Strategies". Diagnostics. 9 (4): 124. doi:10.3390/diagnostics9040124. ISSN 2075-4418.
- ↑ 4.0 4.1 4.2 4.3 4.4 Carruthers, Bruce M.; Jain, Anil Kumar; De Meirleir, Kenny L.; Peterson, Daniel L.; Klimas, Nancy G.; Lerner, A. Martin; Bested, Alison C.; Flor-Henry, Pierre; Joshi, Pradip; Powles, AC Peter; Sherkey, Jeffrey A.; van de Sande, Marjorie I. (2003). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Clinical Working Case Definition, Diagnostic and Treatment Protocols" (PDF). Journal of Chronic Fatigue Syndrome. 11 (2): 7–115. doi:10.1300/J092v11n01_02.
- ↑ 5.0 5.1 5.2 Carruthers, BM; van de Sande, MI; De Meirleir, KL; Klimas, NG; Broderick, G; Mitchell, T; Staines, D; Powles, ACP; Speight, N; Vallings, R; Bateman, L; Bell, DS; Carlo-Stella, N; Chia, J; Darragh, A; Gerken, A; Jo, D; Lewis, DP; Light, AR; Light, KC; Marshall-Gradisnik, S; McLaren-Howard, J; Mena, I; Miwa, K; Murovska, M; Stevens, SR (2012), Myalgic encephalomyelitis: Adult & Paediatric: International Consensus Primer for Medical Practitioners (PDF), ISBN 978-0-9739335-3-6
- ↑ "What Does a True ME Definition Look Like?". MEadvocacy.org. Retrieved January 25, 2019.
- ↑ US NIH Report Calls for UK Definition of ME/CFS to be Scrapped - The Argus Report By: Penny Swift
- ↑ Spotila, Jennie; Dimmock, Mary (August 16, 2016). "AHRQ Evidence Review Changes Its Conclusions". occupyme.net. Retrieved January 25, 2019.
- ↑ 9.0 9.1 Tanner, Claudia (2018). "Marathon runner forced to quit work after developing ME claims diet change gave him his life back". iNews.
- ↑ 10.0 10.1 Broadbent, Rick (December 2, 2017). "Muslim fighter with ME who left an arranged marriage to win world". The Times. ISSN 0140-0460. Retrieved February 28, 2019.
- ↑ 11.0 11.1 Park, Andy; O'Halloran, Clare. "Committee reviews 'potentially harmful and old fashioned' chronic fatigue treatments". ABC News. 6mins 18s.
- ↑ 12.0 12.1 Broadbent, Rick (February 27, 2019). "Nathan Douglas: London 2012 was the darkest period of my life". The Times. ISSN 0140-0460. Retrieved February 28, 2019.
- ↑ 13.0 13.1 Spence, Vance. "Snippets | A presentation by MERGE Chairman Dr Vance Spence on 12 November 2005 at the Oak Tree Court Conference Centre, Coventry, at the invitation of the Warwickshire Network for ME". Irish M.E. Association.
(Mommersteeg et al, 2005) shows that the "burnout" experienced by athletes differs from CFS, and is certainly not ME as described in earlier literature. This is just one example of many media stories - thrown out into the public arena - which have an uncertain meaning in the context of ME/CFS
- ↑ 14.0 14.1 Burley, Lucy; Cox, Diane; Findley, Leslie (August 1, 2007). "Severe Chronic Fatigue Syndrome: Recovery is Possible" (PDF). British Journal of Occupational Therapy. pp. 339–344. doi:10.1177/030802260707000803. Retrieved February 11, 2019.
- ↑ 15.0 15.1 Devasahayam, Anoop; Lawn, Tara; Murphy, Maurice; White, Peter D (January 2012). "Alternative Diagnoses to Chronic Fatigue Syndrome in Referrals to a Specialist Service: Service Evaluation Survey". JRSM Short Reports. 3 (1): 1–5. doi:10.1258/shorts.2011.011127. ISSN 2042-5333. PMC 3269106. PMID 22299071.
Half of all the referred patients to a specialist CFS clinic had alternative medical and psychiatric diagnoses.
- ↑ 16.0 16.1 16.2 16.3 Carruthers, Bruce M.; van de Sande, Marjorie I.; De Meirleir, Kenny L.; Klimas, Nancy G.; Broderick, Gordon; Mitchell, Terry; Staines, Donald; Powles, A.C. Peter; Speight, Nigel; Vallings, Rosamund; Bateman, Lucinda; Baumgarten-Austrheim, Barbara; Bell, David; Carlo-Stella, Nicoletta; Chia, John; Darragh, Austin; Jo, Daehyun; Lewis, Donald; Light, Alan; Marshall-Gradisnik, Sonya; Mena, Ismael; Mikovits, Judy; Miwa, Kunihisa; Murovska, Modra; Pall, Martin; Stevens, Staci (August 22, 2011). "Myalgic encephalomyelitis: International Consensus Criteria". Journal of Internal Medicine. 270 (4): 327–338. doi:10.1111/j.1365-2796.2011.02428.x. ISSN 0954-6820. PMC 3427890. PMID 21777306.
- ↑ 17.0 17.1 Murley, Sam (April 10, 2019). "Illness robbed Marshall of crowning glory". Royal Gazette.
- ↑ 18.0 18.1 "Annadale Striders Interview - Derek Graham". Annadale Striders.
- ↑ 19.0 19.1 Marshall, Peter; Kehoe, Nick (2001). Shattered: A Champion's Fight Against a Mystery Illness. Mainstream.
- ↑ 20.0 20.1 "Linley Frame: Olympian and Chronic Fatigue Syndrome sufferer". Australian Broadcasting Corporation. May 4, 2012.
- ↑ 21.0 21.1 "Michelle Akers USA". FIFA. Archived from the original on June 10, 2015.
- ↑ 22.0 22.1 "Benefizspiel für den schwer kranken Olaf Bodden". Die Welt. 2021. Retrieved November 17, 2021.
- ↑ 23.0 23.1 Mitten, Andy (July 24, 2014). "Garton enjoying life after United in LA". Manchester Evening News.
- ↑ 24.0 24.1 24.2 24.3 "Symptoms of ME/CFS | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. January 18, 2019. Retrieved January 22, 2019.
- ↑ 25.0 25.1 25.2 25.3 "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome - Redefining an Illness | Clinicians Guide" (PDF). Nation Academies Press. 2015.
- ↑ 26.0 26.1 26.2 "What is ME/CFS?". Open Medicine Foundation.
- ↑ 27.0 27.1 "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness - Diagnostic Algorithm". nap.edu. 2015. Archived from the original on May 28, 2019.
- ↑ 28.0 28.1 28.2 28.3 "Beyond Myalgid Encephalomyelitis/Chronic Fatigue Syndrome - Redefining an Illness - Clinician's Guide" (PDF). nap.edu. 2015. p. 9.
- ↑ 29.0 29.1 29.2 International Association for Chronic Fatigue Syndrome / Myalgic Encephalomyelitis; Friedberg, Fred; Bateman, Lucinda; Bested, Alison C; Davenport, Todd; Friedman, Kenneth J; Gurwitt, Alan R; Jason, Leonard A; Lapp, Charles W; Stevens, Staci R; Underhill, Rosemary A; Vallings, Rosamund (2014). "Chronic Fatigue Syndrome Myalgic Encephalomyelitis Primer for Clinical Practitioners" (PDF).
- ↑ Jason, Leonard; Taylor, R.R.; Kennedy, C.L.; Song, S; Johnson, D; Torres, S.R. (January 1, 2001). "Chronic fatigue syndrome: Comorbidity with fibromyalgia and psychiatric illness". Medicine and Psychiatry. 4: 29–34.
- ↑ Natelson, Benjamin H. (February 19, 2019). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and Fibromyalgia: Definitions, Similarities, and Differences". Clinical Therapeutics. 41 (4): 612. doi:10.1016/j.clinthera.2018.12.016. ISSN 0149-2918. PMID 30795933.
- ↑ 32.0 32.1 32.2 32.3 32.4 "Etiology and Pathophysiology | Presentation and Clinical Course | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. November 8, 2018. Retrieved January 22, 2019.
- ↑ 33.0 33.1 33.2 "What is ME/CFS? | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. January 18, 2019. Retrieved April 12, 2019.
- ↑ World Health Organization (1969). International Classification of Diseases (PDF). 2 (Eighth revision ed.). Geneva: WHO. p. 173.
Encephalomyelitis (chronic),
(myalgic, benign) 323 - ↑ 35.0 35.1 35.2 35.3 Institute of Medicine (US) (February 10, 2015). "Beyond Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: Redefining an Illness". Washington, DC, US: The National Academies Press. ISBN 978-0-309-31689-7.
- ↑ National Institutes of Health (US) (December 9, 2014), NIH Pathways to Prevention Workshop: Advancing the Research on Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (PDF)
- ↑ 37.0 37.1 Chu, Lily; Valencia, Ian J.; Garvert, Donn W.; Montoya, Jose G. (January 14, 2019). "Onset patterns and course of myalgic encephalomyelitis/chronic fatigue syndrome". Frontiers in Pediatrics. doi:10.3389/fped.2019.00012.
- ↑ "CDC Public Health Grand Rounds - Chronic Fatigue Syndrome - Advancing Research and Clinical Education" (PDF). Centers for Disease Control and Prevention. p. 6.
- ↑ "Presentation and Clinical Course of ME/CFS | Information for Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome ME/CFS". Centers for Disease Control and Prevention. December 12, 2018. Retrieved February 7, 2019.
- ↑ Chronic Fatigue Syndrome Myalgic Encephalomyelitis - Primer for Clinical Practitioners - 2014 Edition - Massachusettes CFIDS/FM Assoc
- ↑ Evans, Meredyth; Jason, Leonard (2018). "Onset patterns of chronic fatigue syndrome and myalgic encephalomyelitis" (PDF). Research on Chronic Diseases: 2.
- ↑ The Lipkin Study, The Vagus Nerve Infection Hypothesis and HHV-6: Kristin Loomis of the HHV-6 Foundation Talks – Pt. I - Health Rising - By: Cort Johnson - June 2014
- ↑ Chronic Fatigue Syndrome - Symptoms - Web MD
- ↑ 44.0 44.1 "Possible Causes | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. January 18, 2019. Retrieved January 27, 2019.
- ↑ "CDC Public Health Grand Rounds - Chronic Fatigue Syndrome - Advancing Research and Clinical Education" (PDF). cdc.gov. p. 6.
- ↑ Rowe, Katherine S.; Vallings, Rosamund; Stewart, Julian M.; Speight, Nigel; Schwartz, Malcolm S.; Medow, Marvin S.; Gurwitt, Alan; Friedman, Kenneth J.; Underhill, Rosemary A. (2017). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer". Frontiers in Pediatrics. 5. doi:10.3389/fped.2017.00121. ISSN 2296-2360.
- ↑ "Is CFS contagious?". ProHealth Forums. Retrieved February 13, 2019.
- ↑ Underhill, Rosemary A.; O'Gorman, Ruth (January 1, 2006). "Prevalence of Chronic Fatigue Syndrome and Chronic Fatigue Within Families of CFS Patients". Journal of Chronic Fatigue Syndrome. 13 (1): 3–13. doi:10.1300/J092v13n01_02. ISSN 1057-3321.
- ↑ "OMF funded research". Open Medicine Foundation. June 4, 2018.
- ↑ "Knowledgebase". My Donor Record - Health, Eligibility & Travel. Retrieved October 8, 2021.
- ↑ "Chronic fatigue syndrome – I have/had chronic fatigue syndrome. Can I donate?". Australian Red Cross. Retrieved May 25, 2022.
- ↑ "Detailed Eligibility Criteria". NZ Blood. Retrieved May 25, 2022.
- ↑ 53.0 53.1 Wilson, Kumanan; Atkinson, Katherine; Keelan, Jennifer (April 8, 2014). "The Use of Preliminary Scientific Evidence in Public Health: A Case Study of XMRV". PLOS Medicine. 11 (4): e1001623. doi:10.1371/journal.pmed.1001623. ISSN 1549-1676. PMC 3979645. PMID 24714396.
- ↑ 54.0 54.1 Stein, Rob (December 3, 2010). "Red Cross bars chronic fatigue patients from donating blood". Washington Post. Retrieved May 25, 2022.
- ↑ "XMRV testing in the UK". ME Association. 2010. Retrieved February 13, 2019.
- ↑ "Redaction, retraction and reaction". Nature Reviews Microbiology. 10 (12): 799. December 2012. doi:10.1038/nrmicro2928. ISSN 1740-1534.
- ↑ "Multicenter Study Finds No Correlation between Chronic Fatigue Syndrome and XMRV". transfusionnews.com. Retrieved February 13, 2019.
- ↑ 58.0 58.1 "Frequently Asked Questions". American Red Cross. Retrieved February 13, 2019.
Your search for "Chronic fatigue syndrome" returned no results.
- ↑ American Association of Blood Banks (October 2012). "Xenotropic Murine Leukemia Virus-Related Virus (XMRV) and other Polytropic Murine Leukemia Viruses (pMLV)" (PDF). p. 3. Retrieved May 25, 2022.
An updated AABB Association Bulletin #12-05 (November 2012) states that individual collectors of blood and cellular therapy products should accept or defer donors with a history of CFS based on their clinical judgment of the donor's health status.
- ↑ "AABB's recommendation on ME/CFS and blood donation". Massachusetts ME/CFS & FM Association. November 25, 2015. Retrieved May 25, 2022.
- ↑ Brea, Jennifer (January 17, 2017). "What happens when you have a disease doctors can't diagnose". YouTube. TED.
- ↑ Brea, Jennifer (June 2016). "What happens when you have a disease doctors can't diagnose". TED.
- ↑ Weber, Veronica (July 10, 2015). "Invisible Illness - Stories of Chronic Fatigue Syndrome". YouTube. Palo Alto Online.
- ↑ "Diagnosis and Management of Myalgic Encephalomyelitis and Chronic Fatigue Syndrome". YouTube. Unrest Film. October 16, 2018.
- ↑ Job Accommodations - MASS CFIDS
- ↑ Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-sectional study in primary care - July 2011
- ↑ 67.0 67.1 "Epidemiology | Presentation and Clinical Course | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. November 8, 2018. Retrieved January 29, 2019.
- ↑ "ME/CFS in Children | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. January 18, 2019. Retrieved January 29, 2019.
- ↑ "Pediatric ME/CFS Home Page". massmecfs.org. Retrieved January 29, 2019.
- ↑ Fact Sheet Autoimmune Disease in Women: NWHIC - Right Diagnosis - Aug 2015
- ↑ Capelli, E.; Zola, R.; Lorusso, L.; Venturini, L.; Sardi, F.; Ricevuti, G. (October 2010). "Chronic fatigue syndrome/myalgic encephalomyelitis: an update". International Journal of Immunopathology and Pharmacology. 23 (4): 981–989. doi:10.1177/039463201002300402. ISSN 0394-6320. PMID 21244747.
- ↑ "Pediatric ME/CFS: Fact Sheet for Healthcare Professionals | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. October 10, 2017. Retrieved October 13, 2018.
- ↑ Bell, David (June 25, 2016). "ME/CFS in Children - by David S. Bell, MD". Open Medicine Foundation. Retrieved August 11, 2018.
- ↑ 74.0 74.1 74.2 74.3 "Prognosis | Presentation and Clinical Course | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. November 8, 2018. Retrieved January 31, 2019.
- ↑ Rowe, Peter C.; Underhill, Rosemary A.; Friedman, Kenneth J.; Gurwitt, Alan; Medow, Marvin S.; Schwartz, Malcolm S.; Speight, Nigel; Stewart, Julian M.; Vallings, Rosamund (2017). "Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Diagnosis and Management in Young People: A Primer". Frontiers in Pediatrics. 5. doi:10.3389/fped.2017.00121. ISSN 2296-2360.
- ↑ "Pediatric ME/CFS links". Massachusetts ME/CFS & FM Association. Retrieved August 11, 2018.
- ↑ "How Many People Have ME/CFS?". American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society. Retrieved January 31, 2019.
- ↑ "Myalgic Encelphalomyelitis/Chronic Fatigue Syndrome (ME/CFS) Key Facts" (PDF). nap.edu. 2015. Archived from the original (PDF) on March 27, 2019.
- ↑ 79.0 79.1 79.2 79.3 Cairns, R.; Hotopf, M. (January 2005). "A systematic review describing the prognosis of chronic fatigue syndrome". Occupational Medicine (Oxford, England). 55 (1): 20–31. doi:10.1093/occmed/kqi013. ISSN 0962-7480. PMID 15699087.
- ↑ Joyce, J.; Hotopf, M.; Wessely, S. (March 1997). "The prognosis of chronic fatigue and chronic fatigue syndrome: a systematic review". QJM: monthly journal of the Association of Physicians. 90 (3): 223–233. ISSN 1460-2725. PMID 9093600.
- ↑ Klimas, Nancy (June 21, 2014). "ME/CFS Diagnosis and Name with Dr. Nancy Klimas (video)".
- ↑ Komaroff, Anthony; Iskander, John (February 17, 2016), "Interview with Dr Anthony Komaroff", CDC Public Health Ground Rounds - Beyond the Data - Chronic Fatigue Syndrome: Advancing Research and Clinical Education
- ↑ "Symptoms and Diagnosis of ME/CFS | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. January 18, 2019. Retrieved February 1, 2019.
- ↑ Croxall, Jack (January 17, 2019). "I think #TwoFacesofME is a really important hashtag. We're only out and about at our best, and our (more frequent) worst often remains hidden. I'm convinced it's why #MEcfs research funding is so low - the problem isn't visible enough. I'm seriously ill in both these photos.pic.twitter.com/hNjK5140kv". @JackCroxall. Retrieved January 17, 2019.
- ↑ Karen (January 17, 2019). "First photo, me in my wheelchair on a rare trip out. Second photo, the inevitable crash. Eye half closed, slurred speech, dizzy, weak, etc. #TwoFacesofMEpic.twitter.com/P2OPnnpQvF". @hopeforMEyet. Retrieved January 17, 2019.
- ↑ Köhler, Henry (January 17, 2019). "#TwoFacesofME First photo from the morning, the other one from the afternoon ( when I failed to nap 30-60 minutes). I am Not severely ill, and my life is ok, even do I wish that one day science will help me & all the #MeCfs sufferers around the globe.pic.twitter.com/wmhfHcfP0p". @Authorportrait. Retrieved January 17, 2019.
- ↑ Lindheimer, Jacob B.; Meyer, Jacob D.; Stegner, Aaron J.; Dougherty, Ryan J.; Van Riper, Stephanie M.; Shields, Morgan; Reisner, Amanda; Shukla, Sanjay K.; Light, Alan R. (April 3, 2017). "Symptom variability following acute exercise in myalgic encephalomyelitis/chronic fatigue syndrome: a perspective on measuring post-exertion malaise". Fatigue: Biomedicine, Health & Behavior. 5 (2): 69–88. doi:10.1080/21641846.2017.1321166. ISSN 2164-1846.
- ↑ Yoshiuchi, Kazuhiro; Cook, Dane B.; Ohashi, Kyoko; Kumano, Hiroaki; Kuboki, Tomifusa; Yamamoto, Yoshiharu; Natelson, Benjamin H. (December 5, 2007). "A real-time assessment of the effect of exercise in chronic fatigue syndrome". Physiology & Behavior. 92 (5): 963–968. doi:10.1016/j.physbeh.2007.07.001. ISSN 0031-9384. PMC 2170105. PMID 17655887.
- ↑ VanNess, J. Mark; Stevens, Staci R.; Bateman, Lucinda; Stiles, Travis L.; Snell, Christopher R. (February 2010). "Postexertional malaise in women with chronic fatigue syndrome". Journal of Women's Health (2002). 19 (2): 239–244. doi:10.1089/jwh.2009.1507. ISSN 1931-843X. PMID 20095909.
- ↑ The Voice of the Patient. A series of reports from the U.S. Food and Drug Administration’s (FDA’s) Patient-Focused Drug Development Initiative. September 2013
- ↑ What Health - International CFS/ME Awareness Day 2017 - CFIDS Association of America
- ↑ What is ME/CFS? - Solve ME/CFS Initiative
- ↑ Hornig, Mady; Montoya, José G; Klimas, Nancy G; Levine, Susan; Felsenstein, Donna; Bateman, Lucinda; Peterson, Daniel L; Gottschalk, C Gunnar; Schultz, Andrew F; Che, Xiaoyu; Eddy, Meredith L; Komaroff, Anthony L; Lipkin, W Ian (February 1, 2015). "Distinct plasma immune signatures in ME/CFS are present early in the course of illness". Science Advances. 1 (1).
- ↑ Nakatomi, Yasuhito; Mizuno, Kei; Ishii, Ishii; Yasuhiro, Wada; Masaaki, Tanaka; Shusaku, Tazawa; Kayo, Onoe; Sanae, Fukuda; Joji, Kawabe; Kazuhiro, Takahashi; Yosky, Kataoka; Susumu, Shiomi; Kouzi, Yamaguti; Masaaki, Inaba; Hirohiko, Kuratsune; Yasuyoshi, Watanabe (March 24, 2014). "Neuroinflammation in Patients with Chronic Fatigue Syndrome/Myalgic Encephalomyelitis: An ¹¹C-(R)-PK11195 PET Study". Journal of Nuclear Medicine. 55 (6): 945-50. doi:10.2967/jnumed.113.131045. PMID 24665088.
- ↑ Stringer, EA; Baker, KS; Carrol, IR; Montoya, JG; Chu, L; Maeker, HT; Younger, JW (April 9, 2013). "Daily cytokine fluctuations, driven by leptin, are associated with fatigue severity in chronic fatigue syndrome: Evidence of inflammatory pathology". J Transl Med. doi:10.1186/1479-5876-11-93. PMC 3637529. PMID 23570606.
- ↑ Zeineh, Michael M.; Kang, James; Atlas, Scott W.; Raman, Mira M.; Reiss, Allan L.; Norris, Jane L.; Valencia, Ian; Montoya, Jose G. (October 29, 2014). "Right Arcuate Fasciculus Abnormality in Chronic Fatigue Syndrome". Radiology. 274 (2): 517–526. doi:10.1148/radiol.14141079. ISSN 0033-8419.
- ↑ Mueller, Christina; Lin, Joanne; Sheriff, Sulaiman; Maudsley, Andrew; Younger, Jarred (2019). "Evidence of widespread metabolite abnormalities in Myalgic encephalomyelitis/chronic fatigue syndrome: assessment with whole-brain magnetic resonance spectroscopy". Brain Imaging and Behavior. 14: 562–572. doi:10.1007/s11682-018-0029-4. Retrieved January 17, 2019.
- ↑ Younger, Jarred (December 14, 2018). "ME/CFS Involves Brain Inflammation: Results from a Ramsay Pilot Study". YouTube. SolveCFS.
- ↑ 99.0 99.1 99.2 99.3 Hickie, Ian; Davenport, Tracey; Wakefield, Denis; Vollmer-Conna, Ute; Cameron, Barbara; Vernon, Suzanne D; Reeves, William C; Lloyd, Andrew; Dubbo Infection Outcomes Study Group (September 14, 2006). "Post-infective and chronic fatigue syndromes precipitated by viral and non-viral pathogens: prospective cohort study". BMJ. 333 (575). doi:10.1136/bmj.38933.585764.AE. PMID 16950834.
- ↑ Jason, Leonard A; Katz, Ben; Gleason, Kristen; McManimen, Stephanie; Sunnquist, Madison; Thorpe, Taylor (2017). "A Prospective Study of Infectious Mononucleosis in College Students" (PDF). International Journal of Psychiatry. 2 (1).
- ↑ Mariani, Mike (September 3, 2019). "A Town for People with Chronic Fatigue Syndrome". New Yorker. Retrieved April 13, 2022.
- ↑ "Experimental treatments". American Myalgic Encephalomyelitis and Chronic Fatigue Syndrome Society. Retrieved March 18, 2021.
- ↑ Hemispherx Biopharma, Inc. (August 23, 2016). "Hemispherx Biopharma Announces Major Breakthrough: Approval for Commercial Sale of Rintatolimod (U.S. Tradename: Ampligen®) to Treat Severe Cases of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) in the Argentine Republic". GlobeNewswire News Room. Retrieved August 13, 2018.
- ↑ "Hemispherx Biopharma, Inc. Executive Informational Overview" (PDF). Crystal Research Associates. November 27, 2016.
- ↑ George, John (July 25, 2016). "Hemispherx ships Ampligen for European chronic fatigue syndrome program". bizjournals.com. Retrieved August 13, 2018.
- ↑ Hemispherx BioPharma : Opens FDA-Approved Reimbursement Based Expanded Access Treatment Program for ME/CFS to New Enrollees - 4 Traders
- ↑ "Hemispherx Biopharma Inc. Announces Advancement in Expanded Access Program for Ampligen in the Treatment of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". finance.yahoo.com. GlobeNewswire. January 2, 2019. Retrieved February 10, 2019.
- ↑ Fluge, Øystein; Risa, Kristin; Lunde, Sigrid; Alme, Kine; Rekeland, Ingrid Gurvin; Sapkota, Dipak; Kristoffersen, Einar Kleboe; Sørland, Kari; Bruland, Ove (July 1, 2015). van der Feltz-Cornelis, Christina (ed.). "B-Lymphocyte Depletion in Myalgic Encephalopathy/ Chronic Fatigue Syndrome. An Open-Label Phase II Study with Rituximab Maintenance Treatment". PLOS ONE. 10 (7): e0129898. doi:10.1371/journal.pone.0129898. ISSN 1932-6203. PMC 4488509. PMID 26132314.
- ↑ "Norwegian Rituximab Chronic Fatigue Syndrome (ME/CFS) Trial Fails". Simmaron Research. Retrieved November 21, 2021.
- ↑ Fluge, Øystein; Rekeland, Ingrid G.; Lien, Katarina; Thürmer, Hanne; Borchgrevink, Petter C.; Schäfer, Christoph; Sørland, Kari; Aßmus, Jörg; Ktoridou-Valen, Irini (April 2, 2019). "B-Lymphocyte Depletion in Patients With Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial". Annals of Internal Medicine. doi:10.7326/M18-1451. ISSN 1539-3704. PMID 30934066.
- ↑ Younger, Jarred. "Research. Neuroinflammation Pain and Fatigue Laboratory". Retrieved November 21, 2021.
- ↑ "Monitoring the Use of All Medicines and Supplements | Clinical Care of Patients | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. November 8, 2018. Retrieved January 27, 2019.
- ↑ ME Association (UK) (May 29, 2015). "Our CBT, GET and Pacing Report calls for major changes to therapies offered for ME/CFS".
- ↑ "Norwegian patient survey: Experiences of therapeutic approaches (2012)", Phoenix Rising Forum, February 22, 2016
- ↑ 115.0 115.1 115.2 Oxford Clinical Allied Technology and Trials Services Unit (OxCATTS) (February 27, 2019). "Evaluation of a survey exploring the experiences of adults and children with ME/CFS who have participated in CBT and GET interventional programmes. FINAL REPORT" (PDF). Oxford Brookes University.
- ↑ Coyne, James Charles; Laws, Keith R (2016). "Results of the PACE follow-up study are uninterpretable". The Lancet Psychiatry. 3 (2): e6–e7. doi:10.1016/S2215-0366(15)00551-9. ISSN 2215-0366.
- ↑ "List of ME/CFS articles published at Virology Blog".
- ↑ Geraghty, Keith (May 2017). "Further Commentary on the PACE Trial: Biased Methods and Unreliable Outcomes". Journal of Health Psychology. doi:10.1177/1359105317714486.
- ↑ Wilshire, C; Kindlon, T; McGrath, S (2017). "PACE trial claims of recovery are not justified by the data: a rejoinder to Sharpe, Chalder, Johnson, Goldsmith and White". Fatigue: Biomedicine, Health & Behavior. 5 (1): 62-67. doi:10.1080/21641846.2017.1259724.
- ↑ #MEAction (October 2015). "Petition: Misleading Claims Should Be Retracted". #MEAction.
- ↑ Davis, Ronald W; Edwards, Jonathan C W; Jason, Leonard A; Levin, Bruce; Racaniello, Vincent R; Reingold, Arthur L; Ablashi, Dharam V; Baraniuk, James N; Barcellos, Lisa F; Bateman, Lucinda; Bell, David S; Bested, Alison C; Broderick, Gordon; Chia, John; Chu, Lily; Enlander, Derek; Fletcher, Mary Ann; Friedman, Kenneth; Kaufman, David L; Klimas, Nancy; Lapp, Charles W; Levine, Susan; Light, Alan R; Marshall-Gradisnik, Sonya; Medveczky, Peter G; Nahle, Zaher; Oleske, James M; Podell, Richard N; Shepherd, Charles; Snell, Christopher R; Speight, Nigel; Staines, Donald; Stark, Philip B; Stein, Eleanor; Swartzberg, John; Tompkins, Ronald G; Underhill, Rosemary; Vallings, Rosamund; VanElzakker, Michael; Weir, William; Zinn, Marcie L; Zinn, Mark A (February 10, 2016). "An open letter to the Lancet - again". Virology Blog.
- ↑ #MEAction (March 13, 2016). "24 organisations in 14 countries tell QMUL: Release the PACE data".
- ↑ Twisk, Frank NM; Geraghty, Keith J (July 11, 2015). "Deviant Cellular and Physiological Responses to Exercise in Myalgic Encephalomyelitis and Chronic Fatigue Syndrome" (PDF). Jacobs Journal of Physiology. 1 (2): 007.
- ↑ NICE Guideline Development Group (October 29, 2021). "Myalgic Encephalomyelitis (or Encephalopathy)/Chronic Fatigue Syndrome:diagnosis and management. NICE guideline". National Institute for Health and Care Excellence.
- ↑ "Treatment | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)". Centers for Disease Control and Prevention. July 3, 2018. Retrieved November 22, 2021.
- ↑ "IOM 2015 Diagnostic Criteria | Diagnosis | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. July 10, 2018. Retrieved September 7, 2018.
- ↑ "Proposed Approach to ME/CFS Diagnosis in Children and Adults | Diagnosis | Healthcare Providers | Myalgic Encephalomyelitis/Chronic Fatigue Syndrome". Centers for Disease Control and Prevention. July 12, 2018. Retrieved September 7, 2018.
- ↑ Pheby, D; Saffron, L (2009). "Risk factors for severe ME/CFS" (PDF). Biology and Medicine. 1 (4). eISSN 0974-8369.
- ↑ ME/CFS Patient Survey Report: Ministry of Health Survey Reveals Harsh Reality of ME/CFS Patients in Japan - IACFSME - By Mieko Shinohara
- ↑ "Mentions of postviral fatigue syndrome (benign myalgic encephalomyelitis), deaths registered in England and Wales, 2001 to 2016". Office for National Statistics. Retrieved March 6, 2019.
- ↑ Tuller, David (February 1, 2016). "Trial By Error, Continued: A Few Words About "Harassment"". Virology blog. Retrieved January 21, 2019.
- ↑ Kennedy, Brian; Stephenson, Darryl; Watson, Nigel. "First-tier tribunal: Information Rights Appeal EA/2015/0269" (PDF). p. 40.
The evidence of [expert witness] Professor Anderson that third parties could not identify participants from the information alone and that, when pressed, he said that the chance of an "activist" being able to discover information that would lead to individual identification was remote, it was clear that his assessment of activist behaviour was, in our view, grossly exaggerated and the only actual evidence was that an individual at a seminar had heckled Professor Chalder. The identity of those questioning the research, who had signed an open letter or supported it, was impressive.
- ↑ "The Story of B - Children with ME. Appropriate ME Treatment Parliament debate". January 24, 2018.
- ↑ The Mental Health Movement: Persecution of Patients?
- ↑ #MEAction meets with Senate staffers
- ↑ Tuller, David (July 10, 2017). "Trial By Error: The CDC Drops CBT/GET - Virology Blog". Virology blog.
- ↑ Myalgic Encephalomyelitis/Chronic Fatigue Syndrome - CDC.gov
- ↑ Information for Healthcare Providers - ME/CFS - CDC
- ↑ New ME/CFS Web Content for Healthcare Providers - CDC - Jul 12, 2018
- ↑ Unger, Elizabeth; Medscape (February 25, 2019). "Chronic Fatigue Syndrome: It's Real, and We Can Do Better". Medscape. Retrieved February 25, 2019.
- ↑ Sadly, not the first (Comment Section)
- ↑ First official UK death from chronic fatigue syndrome - New Scientist
- ↑ Griffith, J.P.; Zarrouf, F.A. (2008). "A Systematic Review of Chronic Fatigue Syndrome: Don't Assume It's Depression". Primary Care Companion to The Journal of Clinical Psychiatry. 10 (2): 120–128. doi:10.4088/pcc.v10n0206. PMC 2292451. PMID 18458765.
- ↑ Hawk, C; Jason, L; Torres-Harding, S (2006). "Differential diagnosis of chronic fatigue syndrome and major depressive disorder" (PDF). International Journal of Behavioral Medicine. 13 (3): 244-51. doi:10.1207/s15327558ijbm1303_8. PMID 17078775.
- ↑ Myhill, Sarah. "CFS or depression - what are the differences". DrMyhill. Retrieved March 22, 2021.