Exercise
Evidence for graded exercise[edit | edit source]
Physiological effects of exercise[edit | edit source]
Exercise causes a variety of temporary physiological changes in healthy people.
Immune system[edit | edit source]
In healthy people, exercise induces a variety of temporary changes to immune markers. Immediately after exercise, natural killer cell activity is decreased and Leukotriene B4 (LTB4) increase, along with the LTB4/PGE2 ratio. Exercise elevates levels of prostaglandin E2 (PGE2) for up to five days.[1]
Neurotransmitters[edit | edit source]
Acetylcholine, an important neurotransmitter that regulates immune response and muscle strength, decreases during exercise.
Effects of exercise in Chronic Fatigue Syndrome[edit | edit source]
Post Exertional Malaise[edit | edit source]
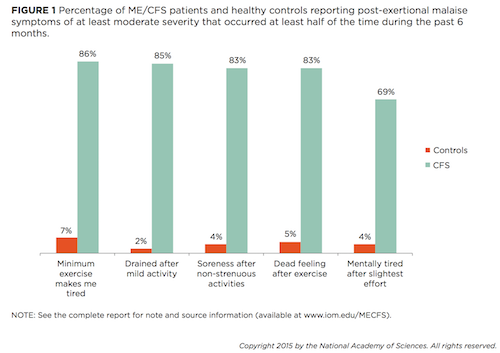
ME patients who exercise are likely to experience Post-exertional malaise which is a worsening of symptoms following physical, mental, emotional or sensory exertion.
Read the main page: Post-exertional malaise.
Pain threshold[edit | edit source]
Pain thresholds drop in people with CFS (as per the Fukuda criteria) after graded exercise, whereas in healthy controls, pain thresholds rise. This phenomenon is attributed by the study researchers to a dysfunction of the central anti-nociceptive mechanism in CFS patients.[2]
Microbiome[edit | edit source]
A small study of ten CFS patients found significant changes in the composition of the microbiome and increased bacterial translocation (movement from the intestine into the bloodstream following exercise. In the blood, the study found increased Clostridium fifteen minutes after exercise and increased Bacilli 48 hours later.[3]
Musculature[edit | edit source]
Exercise has also been found to induce both early and excessive lactic acid formation in the muscles[4] with reduced intracellular concentrations of ATP and acceleration of glycolysis.[5] Several studies have found abnormal increases in plasma lactate following short period of moderate exercise that cannot be explained by deconditioning.[6]
There is evidence of loss of capacity to recover from acidosis on repeat exercise.[7]
There is evidence of abnormalities of AMPK activation and glucose uptake in cultured skeletal muscle cells in ME/CFS patients.[8][9]
There is evidence of abnormalities in pH handling by peripheral muscle,[10] and possible evidence of an increased acidosis and lactate accumulation.[11]
Gene expression[edit | edit source]
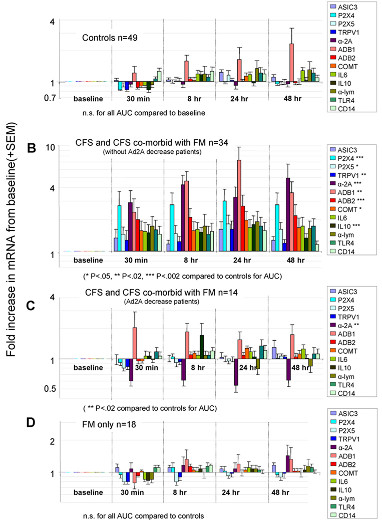
There is evidence of increased gene expression following muscular exertion.[12][13][14]
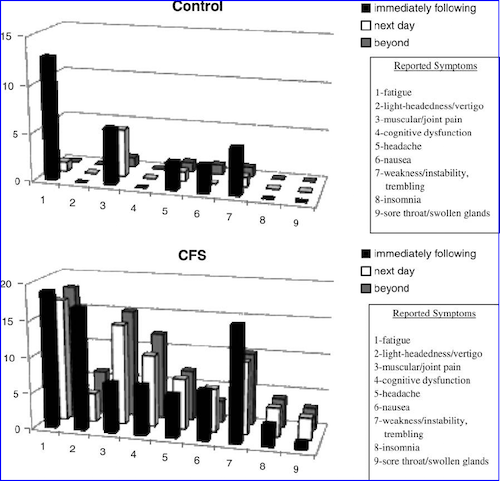
A 2011 study found that moderate exercise in CFS increased the expression of 13 genes (sensory, adrenergic and 1 cytokine) for 48 hours, and the increases correlated with fatigue and pain levels.[13] (see graph at right)
Second day exercise test[edit | edit source]
The seminal study on the response by CFS patients to a 2-day cardiopulmonary exercise test was published by Mark VanNess, Christopher Snell & Staci Stevens in 2007: "Diminished Cardiopulmonary Capacity During Post-Exertional Malaise"[15] A repeat study in 2013 confirmed these results.[16]
In a confirmation study, Doctor Betsy Keller found that patients could not repeat their performance on a second cardiopulmonary exercise test performed a day after the first.[17]
A review by Nijs et al. found that multiple studies showed reduced peak heart rate, reduced endurance, reduced peak work rate, reduced peak oxygen uptake, lower blood lactate values, and an increased respiratory exchange ratio;[18] see 'Oxidative impairment', below.
Read the main page: Two-day cardiopulmonary exercise testing.
Oxidative impairment[edit | edit source]
DeBecker et al (2000) and VanNess et al (2003) found low VO2 during exercise testing;[19][20] Fulle et al (2000) demonstrated oxidative damage to DNA.[21]; and Wong et al (1992) showed defects in oxidative metabolism and poor recovery of ATP after exercise.[22]
Notable quotations[edit | edit source]
Mark VanNess[edit | edit source]
Our studies clearly show that dynamic exercise like walking or jogging exacerbates symptoms associated with ME/CFS
Paul Cheney[edit | edit source]
The whole idea that you can take a disease like this and exercise your way to health is foolishness. It is insane
The most important thing about exercise is not to have (patients with ME / CFS) do aerobic exercise. I believe that even progressive aerobic exercise is counter-productive. If you have a defect in mitochondrial function and you push the mitochondria by exercise, you kill the DNA
(Lecture in Orlando, Florida, International Congress of Bioenergetic Medicine, 5th-7th February 1999).
Peter Behan[edit | edit source]
There is "... general agreement that (ME’s) distinguishing characteristic is severe muscle fatigability, made worse by exercise. It becomes apparent that any kind of muscle exercise can cause patients to be almost incapacitated (and) the patient is usually confined to bed."
Peter Behan (1988 Crit Rev Neurobiol: 1988:4:2:157-178)
MS Riley et al[edit | edit source]
Patients with the chronic fatigue syndrome have reduced aerobic work capacity compared with normal subjects and patients with the irritable bowel syndrome. They also have an altered perception of their degree of exertion and their premorbid level of physical activity.[23]
Examples of clinical recommendations[edit | edit source]
While there has been no research on physical therapy alternatives to graded exercise, and many patients find it harmful, many clinicians recommend some exercise or strength training for patients who are able, tending to apply this to non-severely affected patients.
Dr Sarah Myhill[edit | edit source]
Dr Myhill recommends patients who are well enough engage in strength training, specifically Body by Science created by Dr Doug McGuff and John Little. "If muscle strength is correctly developed, this automatically translates into cardiovascular fitness and increased numbers of mitochondria". Dr Myhill has a page on her web site detailing her recommendations[24].
Dr. Lucinda Bateman[edit | edit source]
Dr Bateman encourages her patients to find a way to exercise: "we try to focus on maintaining or improving muscle strength, flexibility and also bit of cardiovascular exercise". She discusses exercise and gene expression in an interview[25].
Dr. Nancy Klimas[edit | edit source]
Dr Klimas recommends patients engage in exercise or movement without exceeding a certain heart rate, a proxy for an individual's anaerobic threshold, as established by a VO2 max test.[26] She also recommends alternating periods of exercise and rest.[27] She says that exercise tends to be better tolerated when performed in a horizontal position, like recumbent bicycling or swimming.
Dr. Ritchie Shoemaker[edit | edit source]
See YouTube video regarding resuming exercise gradually for mold illness aka CIRS patients.
Workwell Foundation[edit | edit source]
Workwell Foundation, which specialises in two-day cardiopulmonary exercise testing (CPET), recommends short periods (eg: 30 seconds) of analeptic exercise, with periods of rest which are 3-6 times longer than the period of exercise. The amount of exercise that the individual undertakes should be guided by VO2 max testing (or a safe heart rate threshold (generally 60% of maximum heart rate)), and the use of a heart rate monitor (both during exercise and to help with pacing) is recommended to ensure that the individual doesn't exceed their capacity. The Foundation also advises against aerobic exercise for people with ME/CFS.[28][29][30]
This approach to exercise differs from Graded Exercise Therapy (GET) in several important ways:
- There is no claim that the exercise program will cure the condition. The aim is to increase functional strength and flexibility, and to improve quality of life, whilst not exacerbating the condition[29]
- This program is based on a deep understanding of Post-exertional malaise (PEM), and the importance of staying within the energy envelope in order to not trigger PEM[28]
- There is a recognition that any approach to exercise with people with ME/CFS must be carefully tailored to the individual. There is no one-size fits all[29]
- This approach utilises objective measures such as VO2 max testing and heart rate monitoring to guide the level of activity suitable for the individual[30]
United States Centers for Disease Control[edit | edit source]
The Centers for Disease Control in the United States recommends patients perform strength and conditioning exercise.[31]
UK NICE Guidelines[edit | edit source]
British patient Sally Burch has written about the The UK National Institute for Health and Care Excellence (NICE) guidelines on maintaining a lower heart rate.[32]
Talks & Interviews[edit | edit source]
- 2016, Dr. Mark Van Ness, "Expanding Physical Capability in ME/CFS" Part 1 (of 2) (Mark VanNess)
- 2016, Dr. Mark Van Ness, "Expanding Physical Capability in ME/CFS" Part 2 (of 2) (Mark VanNess)
- 2015, 72. Gene-expression and exercise / Gen-expressie en inspanning – dr. Lucinda Bateman (Lucinda Bateman, Science for Patients)
- 2014, Mark VanNess 'Exercise and ME/CFS' at Bristol Watershed. Part One[33] (Mark VanNess)
- 2013, CFS gene expression after exercise (part 1) (Lucinda Bateman)
- 2012, Clinical exercise testing in CFS/ME research and treatment (Christopher Snell)
- 2012, MECFS Alert Episode 32: Staci Stevens, Director of the Pacific Fatigue Lab (Staci Stevens, ME/CFS Alert)
- 2012, Top 10 Things You Should Know About Post-Exertional Relapse (Staci Stevens)
- 2010, Slide presentation to CFSAC (Staci Stevens, CFSAC)
- 2009, Staci Steven speaking to CFSAC meeting (Staci Stevens)
Studies[edit | edit source]
- 2016, Effect of Acute Exercise on Fatigue in People with ME/CFS/SEID: A Meta-analysis
- 2016, Cochrane meta-analysis
- 2011, PACE trial
Learn more[edit | edit source]
- 2016, Neuromuscular Strain in ME/CFS – Research Study Conclusion
- 2016, Australian metabolomics study of young women with ME/CFS (CCC)
- 2016, Review Article: Understanding Muscle Dysfunction in Chronic Fatigue Syndrome[34]
- 2016, Lost in Translation - The ME-Polio Connection and the Dangers of Exercise[35]
- 2015, Exercise alteration of the CFS Microbiome
- 2015, Dr VanNess on recent press reports (Mark VanNess, January)[36]
- 2015, Deviant Cellular and Physiological Responses to Exercise in Myalgic Encephalomyelitis and Chronic Fatigue Syndrome [37]
- 2014, ME/CFS and Exercise: VO2 Max Testing with Nancy Klimas M.D. PREVIEW (this is a preview of a pay-per-view video)
- 2014, ME/CFS and Exercise: The VO2 Max Based Exercise Program, A Personal View (Dan Moricoli)
- 2014, Sufferers of chronic fatigue, fibromyalgia have hope in new diagnostic tool[38]
- 2011, Loss of capacity to recover from acidosis on repeat exercise in chronic fatigue syndrome: a case–control study (ME Research UK)
See also[edit | edit source]
- Two-day cardiopulmonary exercise testing
- Graded exercise therapy
- Muscle fatigability
- Mitochondria
- Deconditioning
- Post-exertional malaise
- Body by Science
References[edit | edit source]
- ↑ Gray, J B; Martinovic, A M (July 1994), "Eicosanoids and essential fatty acid modulation in chronic disease and the chronic fatigue syndrome", Medical Hypotheses, 43 (1): 31–42, doi:10.1016/0306-9877(94)90046-9, PMID 7968718
- ↑ Whiteside, Alan; Hansen, Stig; Chaudhuri, Abhijit (2004), "Exercise lowers pain threshold in chronic fatigue syndrome", Pain, 109 (3): 497-9, doi:10.1016/j.pain.2004.02.029, PMID 15157711
- ↑ Shukla, Sanjay K; Cook, Dane; Meyer, Jacob; et al. (December 18, 2015), "Changes in Gut and Plasma Microbiome following Exercise Challenge in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)", PLoS ONE, doi:10.1371/journal.pone.0145453, PMID 26683192
- ↑ Plioplys, AV; Plioplys, S (1995), "Serum levels of carnitine in chronic fatigue syndrome: clinical correlates", Neuropsychobiology, 32 (3): 132-8, PMID 8544970
- ↑ McCully, KK; Natelson, BH; Iotti, S; Sisto, S; Leigh, JS Jr. (May 1996h), "Reduced oxidative muscle metabolism in chronic fatigue syndrome", Muscle Nerve, 19 (5): 621-5, PMID 8618560
- ↑ Lane, R J; Barrett, M C; Taylor, D J; Kemp, G J; Lodi, R (May 1998), "Heterogeneity in chronic fatigue syndrome: evidence from magnetic resonance spectroscopy of muscle", Neuromuscul Disord, 1998 May, 8 (3–4): 204-9, PMID 9631403
- ↑ Jones, David EJ; Hollingsworth, Kieren G; Jakovljevic, Djordje G; et al. (July 12, 2011), "Loss of capacity to recover from acidosis on repeat exercise in chronic fatigue syndrome", Eur J Clin Invest, 2012 Feb, 42 (2): 186-94, doi:10.1111/j.1365-2362.2011.02567.x, PMID 21749371
- ↑ Brown, Audrey E; Jones, David E; Walker, Mark; Newton, Julia L (April 2, 2015), "Abnormalities of AMPK activation and glucose uptake in cultured skeletal muscle cells", PLoS One, 10 (4), doi:10.1371/journal.pone.0122982, PMID 25836975
- ↑ Dobberstein, Linda J. (April 20, 2015), "Master Enzyme Switch Deactivated In Chronic Fatigue Syndrome and Fibromyalgia", Wellness Resources
- ↑ Jones, David EJ; Hollingsworth, Kieren G; Taylor, Renee R; Blamire, Andrew M; Newton, Julia L (April 2010), "Abnormalities in pH handling by peripheral muscle and potential regulation by the autonomic nervous system in chronic fatigue syndrome", J Intern Med, 267 (4): 394-401, doi:10.1111/j.1365-2796.2009.02160.x, PMID 20433583
- ↑ Lengert, Nicor; Drossel, Barbara (July 2015), "In silico analysis of exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome", Biophysical Chemistry, 202: 21–31, doi:10.1016/j.bpc.2015.03.009, PMID 25899994
- ↑ Light, Alan R; White, Andrea T; Hughen, Ronald W; Light, Kathleen C (July 31, 2009), "Moderate exercise increases expression for sensory, adrenergic, and immune genes in chronic fatigue syndrome patients but not in normal subjects", J Pain, 2009 Oct, 10 (10): 1099-112, doi:10.1016/j.jpain.2009.06.003, PMID 19647494
- ↑ 13.0 13.1 Light, Alan R; Bateman, Lucinda; Jo, D; et al. (July 13, 2011), "Gene expression alterations at baseline and following moderate exercise in patients with Chronic Fatigue Syndrome and Fibromyalgia Syndrome", J Intern Med, 2012 271 (1): 64-81, doi:10.1111/j.1365-2796.2011.02405.x, PMID 21615807
- ↑ White, Andrea T; Light, Alan R; Hughen, Ronald W; VanHaitsma, Timothy A; Light, Kathleen C (December 30, 2011), "Differences in metabolite-detecting, adrenergic, and immune gene expression after moderate exercise in patients with chronic fatigue syndrome, patients with multiple sclerosis, and healthy controls", Psychosom Med, 2012 Jan, 74 (1): 46-54, doi:10.1097/PSY.0b013e31824152ed, PMID 22210239
- ↑ Van Ness, J Mark; Snell, Christopher R; Stevens, Staci R (2007), "Diminished Cardiopulmonary Capacity During Post-Exertional Malaise", Journal of Chronic Fatigue Syndrome, 14 (2): 77-85, doi:10.1300/J092v14n02_07
- ↑ Snell, Christopher R; Stevens, Staci R; Davenport, Todd E; Van Ness, J Mark (October 31, 2013), "Discriminative Validity of Metabolic and Workload Measurements for Identifying People With Chronic Fatigue Syndrome", Physical Therapy (APTA), 93 (11): 1484-1492, doi:10.2522/ptj.20110368, PMID 23813081
- ↑ Keller, Betsy A; Pryor, John Luke; Giloteaux, Ludovic (April 23, 2014), "Inability of myalgic encephalomyelitis/chronic fatigue syndrome patients to reproduce VO₂peak indicates functional impairment", J Transl Med, 2014 Apr 23 (12): 104, doi:10.1186/1479-5876-12-104, PMID 24755065
- ↑ Nijs, J; Nees, A; Paul, L; De Kooning, M; Ickmans, K; Meeus, M; Van Oosterwijck, J (2014), "Altered immune response to exercise in patients with chronic fatigue syndrome/myalgic encephalomyelitis: a systematic literature review", Exercise Immunology Review, 2014 (20): 94-116., PMID 24974723
- ↑ De Becker, P; Roeykens, J; Reynders, M; et al. (November 27, 2000), "Exercise capacity in chronic fatigue syndrome", Archives of Internal Medicine, 160 (21): 3270–3277, doi:10.1001/archinte.160.21.3270, ISSN 0003-9926, PMID 11088089
- ↑ Vanness, JM; Snell, CR; Strayer, DR; Dempsey, L; Stevens, SR (June 2003), "Subclassifying chronic fatigue syndrome through exercise testing" (PDF), Medicine and Science in Sports and Exercise, 35 (6): 908–913, doi:10.1249/01.MSS.0000069510.58763.E8, ISSN 0195-9131, PMID 12783037
- ↑ Fulle, S; Mecocci, P; Fanó, G; et al. (December 15, 2000), "Specific oxidative alterations in vastus lateralis muscle of patients with the diagnosis of chronic fatigue syndrome", Free Radical Biology & Medicine, 29 (12): 1252–1259, doi:10.1016/S0891-5849(00)00419-6, ISSN 0891-5849, PMID 11118815
- ↑ Wong, R; Lopaschuk, G; Zhu, G; et al. (December 1992), "Skeletal muscle metabolism in the chronic fatigue syndrome. In vivo assessment by 31P nuclear magnetic resonance spectroscopy", Chest, 102 (6): 1716–1722, doi:10.1378/chest.102.6.1716, ISSN 0012-3692, PMID 1446478
- ↑ Aerobic work capacity in patients with chronic fatigue syndrome
- ↑ Myhill, Sarah, Exercise - the right sort
- ↑ Bateman, Lucinda (November 3, 2015), "Video interview: Gene-expression and exercise", Wetenschap voor Patienten - ME/cvs Vereniging
- ↑ Klimas, Nancy; Moricoli, Dan (July 24, 2011), "Safe Exercise? The Heart Rate Based Exercise Video Series with Dr. Klimas on ME-CFS Community Center: Pt I", Phoenix Rising
- ↑ Klimas: Exercise for Those with ME/CFS
- ↑ 28.0 28.1 Van Ness, J Mark; Snell, Christopher R; Stevens, Staci R (April 2014), "A Realistic Approach to Exercise for CFS Patients" (PDF), The CFS Research Review
- ↑ 29.0 29.1 29.2 Snell, Christopher R; Van Ness, J Mark; Stevens, Staci R (2004), "When Working Out Doesn't Work Out" (PDF), The CFIDS Chronicle
- ↑ 30.0 30.1 Stevens, Staci R; Davenport, Todd E (2010), "Functional Outcomes of Anaerobic Rehabilitation in a Patient with Chronic Fatigue Syndrome: case report with 1-year follow-up" (PDF), Bulletin of the IACFS/ME, 2010, 18 (3): 93-98
- ↑ Chronic Fatigue Syndrome (CFS)
- ↑ Burch, Sally (November 14, 2015), Slideshow: Heart rate monitoring and NICE guideline for ME
- ↑ Van Ness, J Mark (February 5, 2014), Video: A Realistic Approach to Exercise and Rehabilitation in ME/CFS, Bristol Watershed
- ↑ Rutherford, Gina; Manning, Philip; Newton, Julia L (January 13, 2016), "Review Article: Understanding Muscle Dysfunction in Chronic Fatigue Syndrome", Journal of Aging Research, 2016 (2016) (Article ID 2497348, 13 pages), doi:10.1155/2016/2497348, PMID 26998359
- ↑ Blake, Nancy (February 10, 2016), "Lost in Translation - The ME-Polio Connection and the Dangers of Exercise", ProHealth website
- ↑ Burch, Sally; Van Ness, J Mark (January 17, 2015), Dr Van Ness on recent press reports
- ↑ Twisk, Frank NM; Geraghty, Keith J (July 11, 2015), "Deviant Cellular and Physiological Responses to Exercise in Myalgic Encephalomyelitis and Chronic Fatigue Syndrome" (PDF), Jacobs Journal of Physiology, 2015, 1(2): 007
- ↑ Deseret News (May 16, 2014), Sufferers of chronic fatigue, fibromyalgia have hope in new diagnostic tool