Exercise: Difference between revisions
(minor edits) |
m (Seeing if the visual editor will let me change the image sizes.) |
||
| (13 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
Exercise is any movement or activity considered to contribute to general health and well-being. Exercise may be recommended as part of a wellness regimen in chronic illness.<ref>{{Cite journal|last=Pederson|first=B.K.|last2=Saltin|first2=B.|date=2006|title=Evidence for prescribing exercise as therapy in chronic disease | |||
|url=https://www.essa.org.au/wp-content/uploads/2015/06/Chronic-disease_Review-2006.pdf|journal=Scand J Med Sci Sports|volume=16(Suppl 1)|pages=3-63|via=}}</ref> <ref>{{Cite journal|last=Hovanec|first=Nina|last2=Bellemore|first2=Derek|last3=Kuhnow|first3=Jason|last4=Miller|first4=Felicia|last5=van Vloten|first5=Alexi|last6=Vandervoort|first6=Anthony A.|date=March 3 2015|title=Exercise Prescription Considerations for Individuals with Multiple Chronic Diseases: Systematic Review|url=https://www.omicsonline.org/open-access/exercise-prescription-considerations-for-individuals-with-multiple-chronic-diseases-systematic-review-2167-7182-1000201.php?aid=41826|journal=J Gerontol Geriatr Res|volume=4:201|pages=|via=}}<nowiki></ref> However, [[Post-exertional malaise|exercise intolerance]] is a central feature of ME/CFS, and patients show multiple documented abnormal responses to exercise. Rather than increase health and well-being, ME/CFS patients report that increased activity has reduced their physical and cognitive capacity over time, sometimes permanently.<ref>{{Cite web|url=http://www.meassociation.org.uk/wp-content/uploads/2015-ME-Association-Illness-Management-Report-No-decisions-about-me-without-me-30.05.15.pdf|title=ME Association illness management report: no decisions about me without me|last=ME Association|first=|date=May 2015|website=ME Association|archive-url=|archive-date=|dead-url=|access-date=25 April 2018}}</ref> | |||
==Physiological effects of exercise== | ==Physiological effects of exercise== | ||
Exercise causes a variety of temporary physiological changes in healthy people. This includes an increase in respiratory rate, heart rate, and blood pressure in order to keep up with higher energy demands.<ref name=":0">{{Cite journal|last=Burton|first=Deborah Anne|last2=Stokes|first2=Keith|last3=Hall|first3=George M|date= | Exercise causes a variety of temporary physiological changes in healthy people. This includes an increase in respiratory rate, heart rate, and blood pressure in order to keep up with higher energy demands.<ref name=":0">{{Cite journal|last=Burton|first=Deborah Anne|last2=Stokes|first2=Keith|last3=Hall|first3=George M|date=December 1, 2004|title=Physiological effects of exercise|url=https://academic.oup.com/bjaed/article/4/6/185/314696|journal=Continuing Education in Anaesthesia Critical Care & Pain|publisher=|volume=4|issue=6|pages=185-8|via=BJA Education}}</ref> The chemical reactions that break down nutrients -- [[glycolysis]], the [[Citric Acid Cycle|Krebs Cycle]], and the [[electron transport chain]] -- move more rapidly to liberate energy, and blood flow to muscles should increase. In healthy individuals, the amount of oxygen and carbon dioxide present in the blood should not alter significantly.<ref name=":0" /> | ||
===Immune system=== | ===Immune system=== | ||
| Line 14: | Line 17: | ||
===Post Exertional Malaise=== | ===Post Exertional Malaise=== | ||
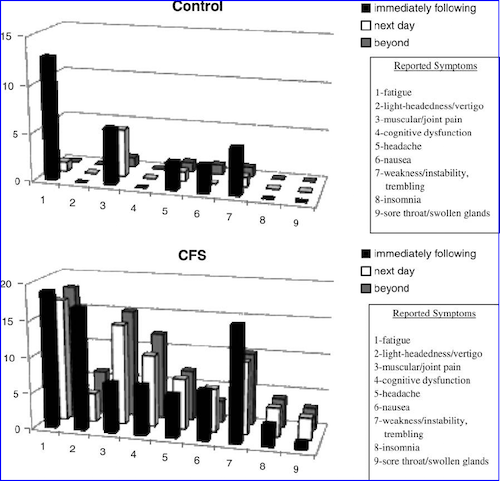
[[File:2010 VanNess Post exertional worsening of symptoms chart.png|right|frame|Post-exertional worsening of symptoms, VanNess et al 2010.png]] | |||
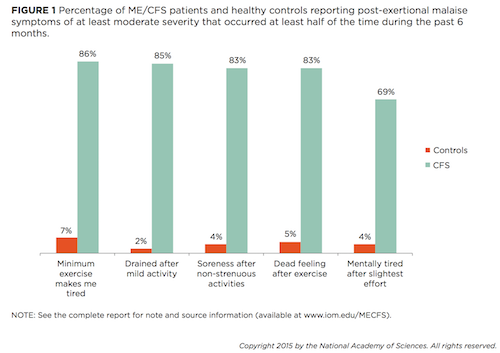
[[File:2015 IOM report PEM chart.png|right|frame|PEM chart from the 2015 Institute of Medicine report]] | [[File:2010 VanNess Post exertional worsening of symptoms chart.png|right|frame|Post-exertional worsening of symptoms, VanNess et al 2010.png|377x377px]] | ||
[[File:2015 IOM report PEM chart.png|right|frame|PEM chart from the 2015 Institute of Medicine report|378x378px]] | |||
[[ME]] patients who exercise are likely to experience [[Post-exertional malaise]] which is a worsening of symptoms following physical, cognitive, or sensory exertion. | [[ME]] patients who exercise are likely to experience [[Post-exertional malaise]] which is a worsening of symptoms following physical, cognitive, or sensory exertion. | ||
| Line 22: | Line 26: | ||
===Pain threshold=== | ===Pain threshold=== | ||
Pain thresholds, or the point at which a stimulus becomes painful, drop in people with [[CFS]] (as per the [[Fukuda criteria]]) after graded exercise. In healthy controls, pain thresholds rise. This phenomenon has been attributed to a dysfunction of the central anti-nociceptive mechanism in [[CFS]] patients.<ref name="Whiteside, 2004" /> | Pain thresholds, or the point at which a stimulus becomes painful, drop in people with [[CFS]] (as per the [[Fukuda criteria]]) after graded exercise. In healthy controls, pain thresholds rise. This phenomenon has been attributed to a dysfunction of the central anti-nociceptive mechanism in [[CFS]] patients.<ref name="Whiteside, 2004" /> | ||
===Immune System=== | |||
Histamine, a chemical that is released in response to cellular damage and inflammation, is released during exercise in healthy individuals. The histamine dilates blood vessels in order to deliver nutrients to working muscles.<ref>{{Cite journal|last=Romero|first=S.A.|last2=Hocker|first2=A.D.|last3=Magnum|first3=J.E.|last4=Luttrell|first4=M.J.|last5=Turnbull|first5=D.W. ...|last6=Halliwill|first6=J.R.|date=2016|title=Evidence of a broad histamine footprint on the human exercise transcriptome|url=http://doi.org/10.1113/JP272177|journal=The Journal of Physiology|volume=594|issue=17|pages=5009-5023|via=}}</ref> However, patients with ME may experience increased histamine release due to increased mast cell populations.<ref>{{Cite journal|last=Rönnberg|first=E|last2=Calounova|first2=G|last3=Pejler|first3=G|date=June 2017|title=Novel characterisation of mast cell phenotypes from peripheral blood mononuclear cells in chronic fatigue syndrome/myalgic encephalomyelitis patients|url=https://www.ncbi.nlm.nih.gov/pubmed/27362406|journal=Asian Pac J Allergy Immunol|volume=35|issue=2|pages=75-81|via=}}</ref> | |||
===Microbiome=== | ===Microbiome=== | ||
| Line 30: | Line 38: | ||
=== Musculature === | === Musculature === | ||
Exercise has also been found to induce both early and excessive lactic acid formation in the [[muscle fatigability|muscles]]<ref name="Plioplys1995" /> with reduced intracellular concentrations of [[ATP]] and acceleration of [[glycolysis]].<ref name="McCully1996" /> Several studies have found abnormal increases in plasma lactate following short period of moderate exercise that cannot be explained by [[deconditioning]].<ref name="LaneRJ1998" /> There is evidence of abnormalities in pH handling by peripheral muscle, | Exercise has also been found to induce both early and excessive lactic acid formation in the [[muscle fatigability|muscles]]<ref name="Plioplys1995" /> with reduced intracellular concentrations of [[ATP]] and acceleration of [[glycolysis]].<ref name="McCully1996" /> Several studies have found abnormal increases in plasma lactate following short period of moderate exercise that cannot be explained by [[deconditioning]].<ref name="LaneRJ1998" /> There is evidence of abnormalities in pH handling by peripheral muscle, and possible evidence of an increased acidosis and lactate accumulation.<ref name="JonesDE2010" /><ref name="LengertN2015" /> | ||
There is also evidence of loss of capacity to recover from acidosis on repeat exercise.<ref name="JonesDE2012" /> | There is also evidence of loss of capacity to recover from acidosis on repeat exercise.<ref name="JonesDE2012" /> | ||
Finally, there is evidence of abnormalities of [[AMPK]] activation and glucose uptake in cultured skeletal muscle cells in ME/CFS patients.<ref name="BrownAE2015" /><ref name="Wellness20150420" /> | Finally, there is evidence of abnormalities of [[AMPK]] activation and glucose uptake in cultured skeletal muscle cells in ME/CFS patients.<ref name="BrownAE2015" /><ref name="Wellness20150420" /> | ||
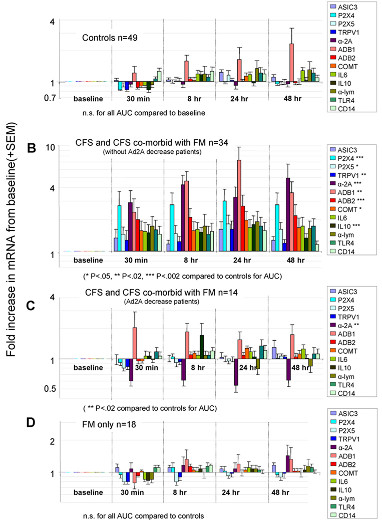
[[File:Light2011-geneexpression-figure3.jpg|right|frame|Gene expression changes following moderate exercise (Light et al, 2011)|516x516px]] | |||
=== Gene expression === | === Gene expression === | ||
There is evidence of increased expression of certain genes following muscular exertion.<ref name="LightAR2009" /><ref name="LightAR2011" /><ref name="WhiteAT2012" /> A 2011 study found that moderate exercise in CFS increased the expression of 13 genes (sensory, adrenergic and 1 cytokine) for 48 hours, and the increases correlated with fatigue and pain levels.<ref name="LightAR2011" /> (see graph at right) | |||
There is evidence of increased | |||
=== Second day exercise test === | === Second day exercise test === | ||
The seminal study on the response by CFS patients to a 2-day cardiopulmonary exercise test was published by [[Mark VanNess]], [[Christopher Snell]] and [[Staci Stevens]] in 2007: "Diminished Cardiopulmonary Capacity During Post-Exertional Malaise"<ref name="VanNess2007" /> A repeat study in 2013 confirmed these results.<ref name="SnellCR2013" /> | The seminal study on the response by CFS patients to a 2-day cardiopulmonary exercise test was published by [[Mark VanNess]], [[Christopher Snell]] and [[Staci Stevens]] in 2007: "Diminished Cardiopulmonary Capacity During Post-Exertional Malaise"<ref name="VanNess2007" /> A repeat study in 2013 confirmed these results.<ref name="SnellCR2013" /> | ||
| Line 61: | Line 64: | ||
== Graded exercise == | == Graded exercise == | ||
{{main|Graded exercise therapy}} | {{main|Graded exercise therapy}} | ||
Graded exercise therapy, or the incremental increase in physical activity over time, is a controversial treatment for ME/CFS, due to exercise intolerance being a central feature of the disease. See the main page for more. | |||
Graded exercise therapy | |||
==Talks & Interviews== | ==Talks & Interviews== | ||
| Line 361: | Line 330: | ||
| url = http://www.prohealth.com/library/showarticle.cfm?libid=25096 | | url = http://www.prohealth.com/library/showarticle.cfm?libid=25096 | ||
}}</ref> | }}</ref> | ||
<ref name="RutherfordG2016">{{citation | <ref name="RutherfordG2016">{{citation | ||
| last1 = Rutherford | first1 = Gina | authorlink1 = Gina Rutherford | | last1 = Rutherford | first1 = Gina | authorlink1 = Gina Rutherford | ||
Revision as of 06:21, April 26, 2018
Exercise is any movement or activity considered to contribute to general health and well-being. Exercise may be recommended as part of a wellness regimen in chronic illness.[1] [2] However, exercise intolerance is a central feature of ME/CFS, and patients show multiple documented abnormal responses to exercise. Rather than increase health and well-being, ME/CFS patients report that increased activity has reduced their physical and cognitive capacity over time, sometimes permanently.[3]
Physiological effects of exercise[edit | edit source]
Exercise causes a variety of temporary physiological changes in healthy people. This includes an increase in respiratory rate, heart rate, and blood pressure in order to keep up with higher energy demands.[4] The chemical reactions that break down nutrients -- glycolysis, the Krebs Cycle, and the electron transport chain -- move more rapidly to liberate energy, and blood flow to muscles should increase. In healthy individuals, the amount of oxygen and carbon dioxide present in the blood should not alter significantly.[4]
Immune system[edit | edit source]
In healthy people, exercise induces a variety of temporary changes to immune markers. Immediately after exercise, natural killer cell activity is decreased and Leukotriene B4 (LTB4) increase, along with the LTB4/PGE2 ratio. Exercise elevates levels of prostaglandin E2 (PGE2) for up to five days.[5]
Neurotransmitters[edit | edit source]
Acetylcholine, an important neurotransmitter that regulates immune response and muscle strength, decreases during exercise.
Effects of exercise in Chronic Fatigue Syndrome[edit | edit source]
Post Exertional Malaise[edit | edit source]
ME patients who exercise are likely to experience Post-exertional malaise which is a worsening of symptoms following physical, cognitive, or sensory exertion.
Read the main page: Post-exertional malaise.
Pain threshold[edit | edit source]
Pain thresholds, or the point at which a stimulus becomes painful, drop in people with CFS (as per the Fukuda criteria) after graded exercise. In healthy controls, pain thresholds rise. This phenomenon has been attributed to a dysfunction of the central anti-nociceptive mechanism in CFS patients.[6]
Immune System[edit | edit source]
Histamine, a chemical that is released in response to cellular damage and inflammation, is released during exercise in healthy individuals. The histamine dilates blood vessels in order to deliver nutrients to working muscles.[7] However, patients with ME may experience increased histamine release due to increased mast cell populations.[8]
Microbiome[edit | edit source]
A small study of ten CFS patients found significant changes in the composition of the microbiome and increased bacterial translocation (movement from the intestine into the bloodstream) following exercise. The study found increased Clostridium in the blood fifteen minutes after exercise and increased Bacilli 48 hours later.[9]
Musculature[edit | edit source]
Exercise has also been found to induce both early and excessive lactic acid formation in the muscles[10] with reduced intracellular concentrations of ATP and acceleration of glycolysis.[11] Several studies have found abnormal increases in plasma lactate following short period of moderate exercise that cannot be explained by deconditioning.[12] There is evidence of abnormalities in pH handling by peripheral muscle, and possible evidence of an increased acidosis and lactate accumulation.[13][14]
There is also evidence of loss of capacity to recover from acidosis on repeat exercise.[15]
Finally, there is evidence of abnormalities of AMPK activation and glucose uptake in cultured skeletal muscle cells in ME/CFS patients.[16][17]
Gene expression[edit | edit source]
There is evidence of increased expression of certain genes following muscular exertion.[18][19][20] A 2011 study found that moderate exercise in CFS increased the expression of 13 genes (sensory, adrenergic and 1 cytokine) for 48 hours, and the increases correlated with fatigue and pain levels.[19] (see graph at right)
Second day exercise test[edit | edit source]
The seminal study on the response by CFS patients to a 2-day cardiopulmonary exercise test was published by Mark VanNess, Christopher Snell and Staci Stevens in 2007: "Diminished Cardiopulmonary Capacity During Post-Exertional Malaise"[21] A repeat study in 2013 confirmed these results.[22]
In a confirmation study, Doctor Betsy Keller found that patients could not repeat their performance on a second cardiopulmonary exercise test performed a day after the first.[23]
A review by Nijs et al. found that multiple studies showed reduced peak heart rate, reduced endurance, reduced peak work rate, reduced peak oxygen uptake, lower blood lactate values, and an increased respiratory exchange ratio;[24] see 'Oxidative impairment', below.
It is important to note that CPET testing oxygen uptake (VO2), carbon dioxide output (VCO2), tidal volume (VT), blood pressure, oxygen saturation, and other objective measures, and cannot be invalidated with inadequate effort.
Read the main page: Two-day cardiopulmonary exercise testing.
Oxidative impairment[edit | edit source]
DeBecker et al (2000) and VanNess et al (2003) found low VO2 during exercise testing;[25][26] Fulle et al (2000) demonstrated oxidative damage to DNA.[27]; and Wong et al (1992) showed defects in oxidative metabolism and poor recovery of ATP after exercise.[28]
Graded exercise[edit | edit source]
Graded exercise therapy, or the incremental increase in physical activity over time, is a controversial treatment for ME/CFS, due to exercise intolerance being a central feature of the disease. See the main page for more.
Talks & Interviews[edit | edit source]
- 2016, Dr. Mark Van Ness, "Expanding Physical Capability in ME/CFS" Part 1 (of 2) (Mark VanNess)
- 2016, Dr. Mark Van Ness, "Expanding Physical Capability in ME/CFS" Part 2 (of 2) (Mark VanNess)
- 2015, 72. Gene-expression and exercise / Gen-expressie en inspanning – dr. Lucinda Bateman (Lucinda Bateman, Science for Patients)
- 2014, Mark VanNess 'Exercise and ME/CFS' at Bristol Watershed. Part One[29] (Mark VanNess)
- 2013, CFS gene expression after exercise (part 1) (Lucinda Bateman)
- 2012, Clinical exercise testing in CFS/ME research and treatment (Christopher Snell)
- 2012, MECFS Alert Episode 32: Staci Stevens, Director of the Pacific Fatigue Lab (Staci Stevens, ME/CFS Alert)
- 2012, Top 10 Things You Should Know About Post-Exertional Relapse (Staci Stevens)
- 2010, Slide presentation to CFSAC (Staci Stevens, CFSAC)
- 2009, Staci Steven speaking to CFSAC meeting (Staci Stevens)
Studies[edit | edit source]
- 2016, Effect of Acute Exercise on Fatigue in People with ME/CFS/SEID: A Meta-analysis
- 2016, Cochrane meta-analysis
- 2011, PACE trial
Learn more[edit | edit source]
- Oct 2, 2017 - For People With Chronic Fatigue Syndrome, More Exercise Isn't Better - by Michaeleen Doucleff for Shots: Health News From NPR
- Aug 12, 2016 - Neuromuscular Strain in ME/CFS – Research Study Conclusion in Solve ME/CFS Initiative Newsletter
- Jul 6, 2016 - Australian metabolomics study of young women with ME/CFS (CCC) by Sasha Nimmo for ME Australia
- Feb 10, 2016 - Lost in Translation - The ME-Polio Connection and the Dangers of Exercise by Nancy Blake for ProHealth[30]
- Jan 2016 - Review Article: Understanding Muscle Dysfunction in Chronic Fatigue Syndrome by Gina Rutherford, Philip Manning, and Julia L. Newton[31]
- Dec 19, 2015 - Exercise alteration of the CFS Microbiome from CFS Remission blog
- Nov 7, 2015 - Deviant Cellular and Physiological Responses to Exercise in Myalgic Encephalomyelitis and Chronic Fatigue Syndrome by Frank N.M. Twisk, and Keith J. Geraghty[32]
- Jan 17, 2015 - Dr. VanNess on recent press reports by Sally Burch in Just ME blog[33]
- 2014 - ME/CFS and Exercise: VO2 Max Testing with Nancy Klimas M.D. - PREVIEW (this is a preview of a pay-per-view video)
- May 16, 2014 - Sufferers of chronic fatigue, fibromyalgia have hope in new diagnostic tool by Wendy Leonard for Deseret News[34]
- Autumn 2011 - Loss of capacity to recover from acidosis on repeat exercise in chronic fatigue syndrome: a case–control study, an essay for ME Research UK
- 2011 - ME/CFS and Exercise: The VO2 Max Based Exercise Program, A Personal View by Dan Moricoli
See also[edit | edit source]
- Two-day cardiopulmonary exercise testing
- Graded exercise therapy
- Muscle fatigability
- Mitochondria
- Deconditioning
- Post-exertional malaise
- Body by Science
References[edit | edit source]
- ↑ Pederson, B.K.; Saltin, B. (2006). "Evidence for prescribing exercise as therapy in chronic disease" (PDF). Scand J Med Sci Sports. 16(Suppl 1): 3–63.
- ↑ Hovanec, Nina; Bellemore, Derek; Kuhnow, Jason; Miller, Felicia; van Vloten, Alexi; Vandervoort, Anthony A. (March 3 2015). "Exercise Prescription Considerations for Individuals with Multiple Chronic Diseases: Systematic Review". J Gerontol Geriatr Res. 4:201. Check date values in:
|date=(help)<nowiki> - ↑ ME Association (May 2015). "ME Association illness management report: no decisions about me without me" (PDF). ME Association. Retrieved April 25, 2018. Cite has empty unknown parameter:
|dead-url=(help) - ↑ 4.0 4.1 Burton, Deborah Anne; Stokes, Keith; Hall, George M (December 1, 2004). "Physiological effects of exercise". Continuing Education in Anaesthesia Critical Care & Pain. 4 (6): 185–8 – via BJA Education.
- ↑ Gray, J B; Martinovic, A M (July 1994), "Eicosanoids and essential fatty acid modulation in chronic disease and the chronic fatigue syndrome", Medical Hypotheses, 43 (1): 31–42, doi:10.1016/0306-9877(94)90046-9, PMID 7968718
- ↑ Whiteside, Alan; Hansen, Stig; Chaudhuri, Abhijit (2004), "Exercise lowers pain threshold in chronic fatigue syndrome", Pain, 109 (3): 497-9, doi:10.1016/j.pain.2004.02.029, PMID 15157711
- ↑ Romero, S.A.; Hocker, A.D.; Magnum, J.E.; Luttrell, M.J.; Turnbull, D.W. ...; Halliwill, J.R. (2016). "Evidence of a broad histamine footprint on the human exercise transcriptome". The Journal of Physiology. 594 (17): 5009–5023.
- ↑ Rönnberg, E; Calounova, G; Pejler, G (June 2017). "Novel characterisation of mast cell phenotypes from peripheral blood mononuclear cells in chronic fatigue syndrome/myalgic encephalomyelitis patients". Asian Pac J Allergy Immunol. 35 (2): 75–81.
- ↑ Shukla, Sanjay K; Cook, Dane; Meyer, Jacob; et al. (December 18, 2015), "Changes in Gut and Plasma Microbiome following Exercise Challenge in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)", PLoS ONE, doi:10.1371/journal.pone.0145453, PMID 26683192
- ↑ Plioplys, AV; Plioplys, S (1995), "Serum levels of carnitine in chronic fatigue syndrome: clinical correlates", Neuropsychobiology, 32 (3): 132-8, PMID 8544970
- ↑ McCully, KK; Natelson, BH; Iotti, S; Sisto, S; Leigh, JS Jr. (May 1996h), "Reduced oxidative muscle metabolism in chronic fatigue syndrome", Muscle Nerve, 19 (5): 621-5, PMID 8618560
- ↑ Lane, R J; Barrett, M C; Taylor, D J; Kemp, G J; Lodi, R (May 1998), "Heterogeneity in chronic fatigue syndrome: evidence from magnetic resonance spectroscopy of muscle", Neuromuscul Disord, 1998 May, 8 (3–4): 204-9, PMID 9631403
- ↑ Jones, David EJ; Hollingsworth, Kieren G; Taylor, Renee R; Blamire, Andrew M; Newton, Julia L (April 2010), "Abnormalities in pH handling by peripheral muscle and potential regulation by the autonomic nervous system in chronic fatigue syndrome", J Intern Med, 267 (4): 394-401, doi:10.1111/j.1365-2796.2009.02160.x, PMID 20433583
- ↑ Lengert, Nicor; Drossel, Barbara (July 2015), "In silico analysis of exercise intolerance in myalgic encephalomyelitis/chronic fatigue syndrome", Biophysical Chemistry, 202: 21–31, doi:10.1016/j.bpc.2015.03.009, PMID 25899994
- ↑ Jones, David EJ; Hollingsworth, Kieren G; Jakovljevic, Djordje G; et al. (July 12, 2011), "Loss of capacity to recover from acidosis on repeat exercise in chronic fatigue syndrome", Eur J Clin Invest, 2012 Feb, 42 (2): 186-94, doi:10.1111/j.1365-2362.2011.02567.x, PMID 21749371
- ↑ Brown, Audrey E; Jones, David E; Walker, Mark; Newton, Julia L (April 2, 2015), "Abnormalities of AMPK activation and glucose uptake in cultured skeletal muscle cells", PLoS One, 10 (4), doi:10.1371/journal.pone.0122982, PMID 25836975
- ↑ Dobberstein, Linda J. (April 20, 2015), "Master Enzyme Switch Deactivated In Chronic Fatigue Syndrome and Fibromyalgia", Wellness Resources
- ↑ Light, Alan R; White, Andrea T; Hughen, Ronald W; Light, Kathleen C (July 31, 2009), "Moderate exercise increases expression for sensory, adrenergic, and immune genes in chronic fatigue syndrome patients but not in normal subjects", J Pain, 2009 Oct, 10 (10): 1099-112, doi:10.1016/j.jpain.2009.06.003, PMID 19647494
- ↑ 19.0 19.1 Light, Alan R; Bateman, Lucinda; Jo, D; et al. (July 13, 2011), "Gene expression alterations at baseline and following moderate exercise in patients with Chronic Fatigue Syndrome and Fibromyalgia Syndrome", J Intern Med, 2012 271 (1): 64-81, doi:10.1111/j.1365-2796.2011.02405.x, PMID 21615807
- ↑ White, Andrea T; Light, Alan R; Hughen, Ronald W; VanHaitsma, Timothy A; Light, Kathleen C (December 30, 2011), "Differences in metabolite-detecting, adrenergic, and immune gene expression after moderate exercise in patients with chronic fatigue syndrome, patients with multiple sclerosis, and healthy controls", Psychosom Med, 2012 Jan, 74 (1): 46-54, doi:10.1097/PSY.0b013e31824152ed, PMID 22210239
- ↑ VanNess, J Mark; Snell, Christopher R; Stevens, Staci R (2007), "Diminished Cardiopulmonary Capacity During Post-Exertional Malaise", Journal of Chronic Fatigue Syndrome, 14 (2): 77-85, doi:10.1300/J092v14n02_07
- ↑ Snell, Christopher R; Stevens, Staci R; Davenport, Todd E; VanNess, J Mark (October 31, 2013), "Discriminative Validity of Metabolic and Workload Measurements for Identifying People With Chronic Fatigue Syndrome", Physical Therapy (APTA), 93 (11): 1484-1492, doi:10.2522/ptj.20110368, PMID 23813081
- ↑ Keller, Betsy A; Pryor, John Luke; Giloteaux, Ludovic (April 23, 2014), "Inability of myalgic encephalomyelitis/chronic fatigue syndrome patients to reproduce VO₂peak indicates functional impairment", J Transl Med, 2014 Apr 23 (12): 104, doi:10.1186/1479-5876-12-104, PMID 24755065
- ↑ Nijs, J; Nees, A; Paul, L; De Kooning, M; Ickmans, K; Meeus, M; Van Oosterwijck, J (2014), "Altered immune response to exercise in patients with chronic fatigue syndrome/myalgic encephalomyelitis: a systematic literature review", Exercise Immunology Review, 2014 (20): 94-116., PMID 24974723
- ↑ De Becker, P; Roeykens, J; Reynders, M; et al. (November 27, 2000), "Exercise capacity in chronic fatigue syndrome", Archives of Internal Medicine, 160 (21): 3270–3277, doi:10.1001/archinte.160.21.3270, ISSN 0003-9926, PMID 11088089
- ↑ VanNess, JM; Snell, CR; Strayer, DR; Dempsey, L; Stevens, SR (June 2003), "Subclassifying chronic fatigue syndrome through exercise testing" (PDF), Medicine and Science in Sports and Exercise, 35 (6): 908–913, doi:10.1249/01.MSS.0000069510.58763.E8, ISSN 0195-9131, PMID 12783037
- ↑ Fulle, S; Mecocci, P; Fanó, G; et al. (December 15, 2000), "Specific oxidative alterations in vastus lateralis muscle of patients with the diagnosis of chronic fatigue syndrome", Free Radical Biology & Medicine, 29 (12): 1252–1259, doi:10.1016/S0891-5849(00)00419-6, ISSN 0891-5849, PMID 11118815
- ↑ Wong, R; Lopaschuk, G; Zhu, G; et al. (December 1992), "Skeletal muscle metabolism in the chronic fatigue syndrome. In vivo assessment by 31P nuclear magnetic resonance spectroscopy", Chest, 102 (6): 1716–1722, doi:10.1378/chest.102.6.1716, ISSN 0012-3692, PMID 1446478
- ↑ VanNess, J Mark (February 5, 2014), Video: A Realistic Approach to Exercise and Rehabilitation in ME/CFS, Bristol Watershed
- ↑ Blake, Nancy (February 10, 2016), "Lost in Translation - The ME-Polio Connection and the Dangers of Exercise", ProHealth website
- ↑ Rutherford, Gina; Manning, Philip; Newton, Julia L (January 13, 2016), "Review Article: Understanding Muscle Dysfunction in Chronic Fatigue Syndrome", Journal of Aging Research, 2016 (2016) (Article ID 2497348, 13 pages), doi:10.1155/2016/2497348, PMID 26998359
- ↑ Twisk, Frank NM; Geraghty, Keith J (July 11, 2015), "Deviant Cellular and Physiological Responses to Exercise in Myalgic Encephalomyelitis and Chronic Fatigue Syndrome" (PDF), Jacobs Journal of Physiology, 2015, 1(2): 007
- ↑ Burch, Sally; VanNess, J Mark (January 17, 2015), Dr VanNess on recent press reports
- ↑ Deseret News (May 16, 2014), Sufferers of chronic fatigue, fibromyalgia have hope in new diagnostic tool
Cite error: <ref> tag with name "Bateman20151103interview" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "BurchS20151114slideshow" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "Klimas20110724phoenix" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "MyhillExercise" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "Workwell201404rae" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "Workwell201404wwodwo" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "Workwell201512foar" defined in <references> is not used in prior text.
Cite error: <ref> tag with name "Klimas2010" defined in <references> is not used in prior text.